Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 3 - May / June of 2008
Vol. 41 nº 3 - May / June of 2008
|
CASE REPORT
|
|
Lung metastasis of benign giant cell tumor: a case report |
|
|
Autho(rs): Thiago Carneiro da Cunha Bosi, Fernando Coelho Goulart de Andrade, Celso Montenegro Turtelli, Hélio Antonio Ribeiro Júnior, Marcelo Cunha Fatureto, Renata Margarida Etchebehere |
|
|
Keywords: Giant cell tumor, Benign, Metastasis |
|
|
Abstract:
IMD, Residents in Radiology and Imaging Diagnosis at Universidade Federal do Triângulo Mineiro (UFMT), Uberaba, MG, Brazil
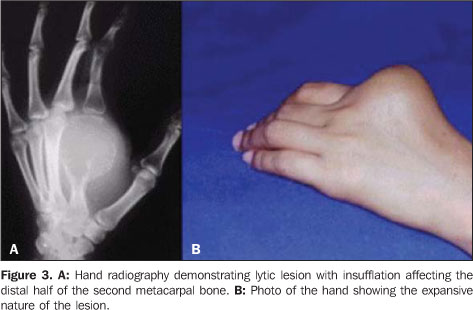
INTRODUCTION Giant cell tumors (GCT) are frequent bone neoplasms, corresponding to about 5-10% of all the primary bone tumors, and 15-25% of benign bone tumors(1). Typical sites of these lesions include the distal femur, proximal tibia, distal radius, and, less frequently, bones of hands where studies demonstrate a higher tendency towards metastasis as compared with other sites(2). The majority of patients affected are in the age range between 20 and 40 years, with a female 2:1 predominance. The highest incidence is found in the Chinese population. Typical radiological findings include lytic lesion with insufflation, trabeculation, with no periosteal reaction, and eccentric localization in the metaphysis of long bones. Histological findings include mononucleated stromal cells and multinucleated giant cells. The present study reports a case of benigsn GCT affecting the metacarpus of a young patient who five year after undergoing surgery developed lung metastases, among which one was giant.
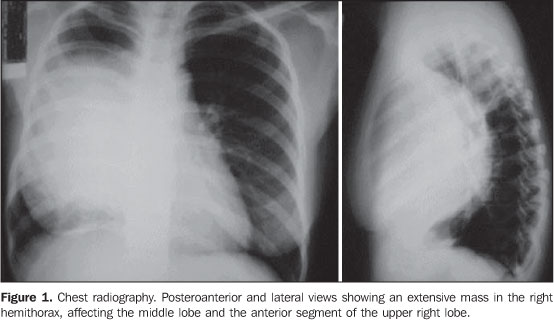
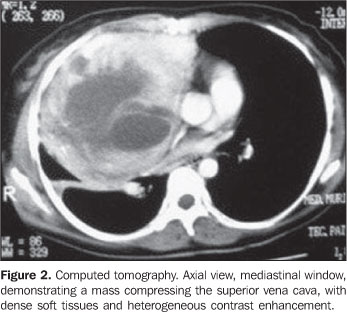
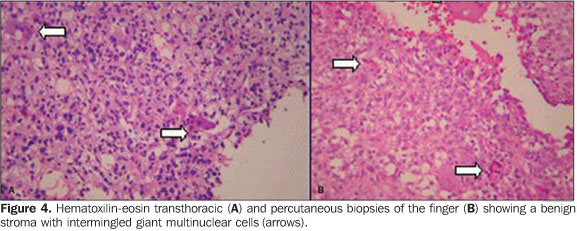
CASE REPORT A female, 28-year-old patient complaining of effort dyspnea and mild chest pain in the right hemithorax, with a tobacco smoking history and pneumonia being treated for one month in another institution where a chest radiograph demonstrated a mass in the right hemithorax. The patient was referred to our institution where a chest computed tomography confirmed the presence of an extensive mass, with dense soft tissues, besides small nodules - two in the pulmonary apices and another on the right lung base. Five years ago, the patient had been submitted to surgery for excision of a tumor localized in the second metacarpal bone of her left hand. Amputation of the metacarpal bone and correspondent chirodactilus was performed. The anatomopathological study demonstrated the presence of a benign GCT, but with extensive adherence of soft tissues. Anatomopathological study of the pulmonary mass performed by means of transthoracic biopsy confirmed the presence of GCT metastasis showing features identical to those of the previously excised hand tumor. Because of the extensive pulmonary involvement, polychemotherapy was adopted as initial treatment of the lesions. Presently, the patient still remains under treatment. The pulmonary nodules disappeared and a moderate decrease in the volume of the mass can be observed.
DISCUSSION Two malignant GCT variants are described: one, with a typical seemingly malignant stroma with intermingled giant cells, and another, with malignant transformation into fibrosarcoma, malignant fibrotic histiocytoma or osteosarcoma, particularly following radiotherapy in cases of recurrent GCTs. Additionally, like in the present case, distant metastases from histologically benign lesions occur in 0% to 9% of cases, with a mild prevalence in women(1-3). Metastases occur preponderantly to the lungs, and rarely to the brain, kidneys, adrenal glands, gastrointestinal tract, other bones and skin. Authors suggest a higher rate of metastases in patients with at least a single episode of local recurrence and in radiologically aggressive tumors extending towards soft tissues. Campanacci et al.(4) have classified this type of tumor into grades I, II and III, according to radiographic findings, grade II and grade III tumors with higher probability of recurrence and metastasis than a grade I tumor. Grade I tumors present well-defined margins and a thin halo of mature bone. Grade II tumors also present well-defined margins, however, the sclerotic halo is absent. Grade III lesions present ill-defined margins suggesting aggressiveness. Meanwhile, the histopathological classification of GCT of bone is not indicative of prognosis(5).
Immunohistochemical studies have been developed with a-SMA, MIC-2, p53, cyclin D1, tc-erb-B2 and Ki-67 antibodies in primary, recurrent and metastatic tumors. Authors have demonstrated a higher ratio of Ki-67-positive cells in more aggressive tumors(5). In the present case, the immunohistochemical analysis was negative for p53 expression in the primary tumor, indicating a low risk for metastatic disease. The lung metastasis resulted positive for CD-68, and negative for S 100 protein, confirming the presence of GCT metastasis. Regarding chronology, in about 75% of benign GCTs with lung metastasis, the time interval between the primary tumor diagnosis and metastasis detection is < 3 years. There are cases with simultaneous primary lesion/metastasis detection. In the present case, the time interval was longer than expected (five years). Metastases tend to present a slow growth, in some circumstances, they stop growing and, rarely a spontaneous regression occurs(3). Tubbs et al.(6) have described the radiological findings of lung metastasis from benign GCT in 13 cases, such as round or oval nodular opacities, homogeneous density, sizes ranging between 0.5 cm and 8.0, well-defined margins, and a narrow transition zone between the lesions and the adjacent pulmonary parenchyma. The greatest majority of these lesions were peripherically located (85%) and in the pulmonary base (62%). In this study, CT was superior to chest radiography for detecting a higher number of nodules and presence of calcifications within these lesions. In the present study, the lesion presented with well-defined margins, but with huge dimensions (18.0 cm × 13.0 cm × 12.0 cm), heterogeneous density, localized in the middle and right upper lobes. The smaller nodules presented with the same features of those described by Tubbs et al.(6).
CONCLUSION Although rare, CGT metastases must always be considered, requiring periodical followup after the primary tumor resection, considering that the symptoms show up late in the disease process, when these lesions may no longer be curable by resection.
REFERENCES 1.Catalan J, Fonte AC, Lusa JRB, et al. Tumor de células gigantes ósseo: aspectos clínicos e radiográficos de 115 casos. Radiol Bras. 2006;39:119-22. [ ] 2.Kay RM, Eckardt JJ, Seeger LL, et al. Pulmonary metastasis of benign giant cell tumor of bone. Six histologically confirmed cases, including one of spontaneous regression. Clin Orthop Relat Res. 1994;(302):219-30. [ ] 3.Greenspan A. Radiologia ortopédica. 3ª ed. Rio de Janeiro: Guanabara Koogan; 2001. [ ] 4.Campanacci M, Giunti A, Olmi R. Giant cell tumors of bone: a study of 209 cases with long-term follow-up in 130. Ital J Orthop Traumatol. 1975;1: 249-77. [ ] 5.Osaka S, Sugita H, Yoshida Y, et al. Clinical and immunohistochemical characteristics of benign giant cell tumour of bone with pulmonary metastases: case series. J Orthop Surg (Hong Kong). 2004;12:55-62. [ ] 6.Tubbs WS, Brown LR, Beabout JW, et al. Benign giant-cell tumor of bone with pulmonary metastases: clinical findings and radiological appearance of metastases in 13 cases. AJR Am J Roentgenol. 1992;158:331-4. [ ] Received October 24, 2006. Accepted after revision January 19, 2007. * Study developed at Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554