Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 3 - May / June of 2008
Vol. 41 nº 3 - May / June of 2008
|
CASE REPORT
|
|
Schwannoma of the inferior turbinate: case report and review of literature |
|
|
Autho(rs): Iman Khodaei, Elgan Davies |
|
|
Keywords: Schwannoma, Inferior turbinate, Nasal tumours |
|
|
Abstract: IFellow of the Royal College of Surgeons, ENT Specialist Registrar, Medical Doctor of the Royal Liverpool University Hospital, Liverpool, United Kingdom
INTRODUCTION The presence of a unilateral nasal mass should alert the clinician to a wide variety of possible diagnoses. While some of these tumours are malignant, the majority are benign. Peripheral nerve sheath tumours include schwannomas and neurofibromas. With the exception of the first and second cranial nerves that lack Schwann cells, these benign, slow growing tumours are reported on the rest of the cranial nerves and therefore been noted to occur in most places within the head and neck(1). As a whole, most schwannomas occur in the head and neck region (45%) or as a solitary mass on the flexor surface of extremities, and in the roots of spinal nerves. Only 4% of schwannomas are found in the sinonasal tract. In contrast to neurofibromas, they do not have a tendence for malignant transformation and are not associated with Recklinghausen's disease, an autosomal dominant condition(2). To our knowledge, only few cases of schwannoma of the inferior turbinate has been reported. We describe the case of a 69 year old female patient with rhinosinusitis and polypoidal changes throughout her sinuses who had endoscopic sinus surgery and trimming of her inferior turbinates. A schwannoma was an incidental finding on the histology of the left inferior turbinate.
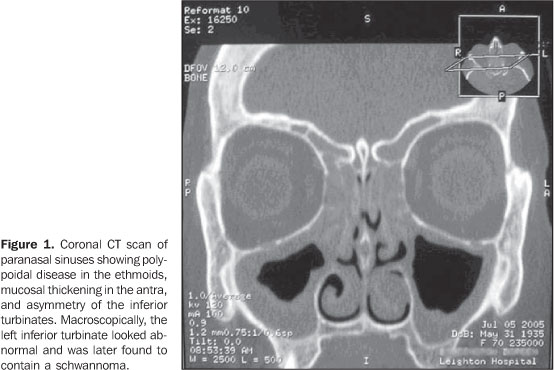
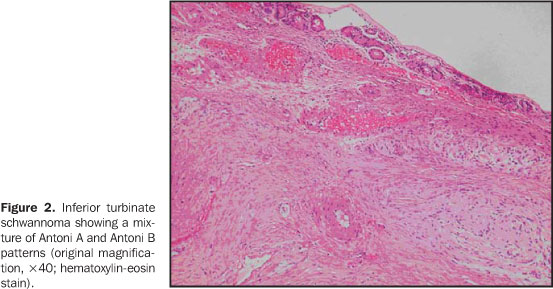
CASE REPORT A 69 year old woman presented to our department with chronic symptoms of rhinosinusitis and a deviated nasal septum. As her symptoms did not improve with medical therapy, a computed tomography (CT) study was requested, which showed polypoid changes in the anterior ethmoids and hypertrophy of the inferior turbinates (Figure 1). She underwent endoscopic surgery, which revealed polypoid middle turbinate and thick, inspissated mucus in the maxillary antrum. Following an anterior ethmoidectomy and middle-meatal antrostomy, she also had excision of both inferior turbinates. However, as the left inferior turbinate looked abnormal, it was sent for histology. Surprisingly, the histology disclose a schwannoma, completely excised. Histological features of the tumour included typical palisades of spindle-shape cells with indistinct cytoplasmic borders (Figure 2). There were no features of malignancy. Four months after the initial operation, the patient remained well with no sign of recurrence.
DISCUSSION The term schwannoma is currently the agreed name for tumours that arise from the neural sheath cells, or Schwann cells, that are ultimately of neuro-ectodermal origin(2). Occurring with equal propensity in men and women, these tumours tend to be more common between the ages from 30 to 60. As the tumour grows, the nerve fibres are pushed aside and onto the surface of the tumour. Loss of sensation or paralysis is therefore rare. While only 3-4% of all schwannomas occur in the sinonasal tract, the ethmoids are the commonest reported site, followed by the antra, nasal cavity and the sphenoid sinus(3). Typical symptoms of a nasal schwannoma include unilateral nasal obstruction and epistaxis. Purulent rhinorrhoea may follow involvement of the middle meatus, while pressure effects can lead to proptosis, facial pain and cranial nerve palsies(4). Radiologically, CT study is indicated in the initial investigation of schwannomas in order to define the tumour's anatomical position and relationship to surrounding structures, in addition to size and presence of bony erosion. If the CT study confirms extension of the schwannoma into the orbit or intracranial cavity, an magnetic resonance imaging (MRI) may further help to distinguish the tumour from its surrounding soft tissues. Macroscopically, these tumours are well demarcated, encapsulated, and may have different colours such as grey, yellow or pink due to increased vascularity. Histologically, they have been divided into two types: Antoni A and Antoni B. This division is of academic interest and does not affect the tumour's behaviour. On MRI scanning, the number of cells can affect the intensity of the image. Often areas of Antoni A (high cellular density) and Antoni B (low cellular density) are seen in the same tumour. Typically, in the Antoni A tumours, whorls of spindle-shaped cells are arranged in palisades with indistinct cytoplasmic borders. Verocay bodies are groups of nuclei arranged in parallel with each other. In contrast, Antoni B areas are far less cellular and the cells appear in a haphazard manner with a myxoid stroma. Degenerative changes such as cyst formation are not uncommon in schwannomas(5). Rarely, the tumour can become very cellular and mistakenly diagnosed as a malignant schwannoma(6); however, malignant degeneration is exceedingly uncommon. Features that distinguish a schwannoma from a neurofibroma include a neurofibroma's lack of a capsule and proliferation of all the elements of a peripheral nerve, such as the axons, Schwann cells, fibroblasts and perineural cells(7). As these tumours are encapsulated, solitary and slow growing, excellent results have been reported with local excision using endoscopic sinus surgery techniques. Excising these tumours endoscopically avoids the external scar of a lateral rhinotomy. However, for larger schwannomas, an external approach may become necessary(8-10). In conclusion, schwannomas of the nose are rare benign tumours that may present with symptoms of nasal obstruction or epistaxis. They are a rare cause of unilateral nasal mass. Initial CT study and a biopsy to confirm the histology can be followed by endoscopic excision and lead to full resolution.
REFERENCES 1.Persaud RA, Hajioff D, Chevretton EB. Intranasal schwannoma in a young woman. Int J Clin Pract. 2004;58:426-8. [ ] 2.Batsakis JG. Tumors of the peripheral nervous system. In: Batsakis JG, editor. Tumors of the head and neck, clinical and pathological correlations. 2nd ed. Baltimore: Williams & Wilkins; 1979. p. 313-33. [ ] 3.Srinivasan V, Deans JA, Nicol A. Sphenoid sinus schwannoma treated by endoscopic excision. J Laryngol Otol. 1999;113:466-8. [ ] 4.Calcaterra TC, Rich JR, Ward PW. Neurilemoma of the sphenoid sinus. Arch Otolaryngol. 1974; 100:383-5. [ ] 5.Sarioglu S, Ozkal S, Guneri A, et al. Cystic schwannoma of the maxillary sinus. Auris Nasus Larynx. 2002;29:297-300. [ ] 6.al-Otieschan AT, Manohar MB, Gangopadhyay K, et al. Cellular schwannoma of the paranasal sinuses: initial report of a case. Ear Nose Throat J. 2002;81:281-4. [ ] 7.Berlucchi M, Piazza C, Blanzuoli L, et al. Schwannoma of the nasal septum: a case report with review of the literature. Eur Arch Otorhinolaryngol. 2000;257:402-5. [ ] 8.Pasquini E, Sciarretta V, Farneti G, et al. Endoscopic endonasal approach for the treatment of benign schwannoma of the sinonasal tract and pterygopalatine fossa. Am J Rhinol. 2002;16: 113-8. [ ] 9.Cakmak O, Yavuz H, Yucel T. Nasal and paranasal sinus schwannomas. Eur Arch Otorhinolaryngol. 2003;260:195-7. [ ] 10.Shinohara K, Hashimoto K, Yamashita M, et al. Schwannoma of the nasal septum removed with endoscopic surgery. Otolaryngol Head Neck Surg. 2005;132:963-4. [ ]
Received April 10, 2008. Accepted after revision May 16, 2008.
* Study developed at the Department of ENT Surgery, Leighton Hospital, Crewe, United Kingdom. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554