Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 2 - Mar. / Apr. of 2008
Vol. 41 nº 2 - Mar. / Apr. of 2008
|
ICONOGRAPHIC ESSAY
|
|
Magnetic resonance imaging in deep pelvic endometriosis: iconographic essay |
|
|
Autho(rs): Antonio Carlos Coutinho Junior, Cláudio Márcio Amaral de Oliveira Lima, Elisa Pompeu Dias Coutinho, Érica Barreiros Ribeiro, Marisa Nassar Aidar, Emerson Leandro Gasparetto |
|
|
Keywords: Magnetic resonance imaging, Endometriosis, Female pelvis, Infertility |
|
|
Abstract:
IMDs, Radiologists at Clínica de Diagnóstico por Imagem (CDPI) and Clínica Multi–Imagem, Rio de Janeiro, RJ, and Centro de Diagnóstico por Imagem Fátima, Nova Iguaçu, RJ, Brazil
INTRODUCTION Firstly described in 1860 by Von Rokitansky(1), endometriosis is defined as the presence of functional endometrial tissue outside the endometrial cavity and myometrium(2,3). Endometriosis is a frequent disease attributed to multifactorial causes, affecting 7% to 10% of women in the general population(3,4). The most widely accepted theory is that viable endometrial cells originating from a physiological phenomenon called retrograde menstruation, result in implantation into the peritoneal cavity (Sampson's theory)(2,5–7). Studies in the literature report a wide range of factors of individual risk such as low parity, age, ethnic origin, height, body mass index, alcohol abuse, tobacco smoking, among others(8). The significant role of MRI in the diagnosis of endometriosis is related to the identification of intermingled lesions in the presence of adhesions, and also the demonstration and evaluation of sub–peritoneal lesions extent in cases where these lesion cannot be visualized by laparoscopy, with accuracy, sensitivity and specificity > 90% for deep endometriosis(9,10). MRI findings are more specific than those of ultrasonography and computed tomography(8,9,11–13). Generally, endometriosis implants are confined to the pelvis, the most common sites, in order of decreasing frequency, being ovaries, broad ligaments, anterior and posterior cul–de–sac, and uterosacral ligaments; however, distant sites may be involved(2,4,7,9). Endometrial tissue implants are affected by cyclic menstrual changes with periodic bleedings. Hemorrhage inside these implants induces an acute pelvic inflammatory reaction and consequential adhesions development, frequently with Douglas cul–de–sac obliteration, Fallopian tubes and ovaries distortion. In patients with deep pelvic endometriosis, by definition, there is a sub–peritoneal ³ 5 mm penetration by endometrial implant. Deep endometriosis generally is found in the retrovaginal septum, rectum, bladder and other pelvic fibromuscular structures such as uterine ligaments and vagina(4,7,8). Despite the asymptomatic nature of the disease in many women affected by peritoneal endometriosis, patients with deep pelvic endometriosis may present with pelvic pain, dysmenorrhea, dyspareunia, urinary symptoms and infertility(2,5,6). MRI presents the advantage of fast acquisition of multiplanar sequences, providing simultaneous images of all the pelvic viscera both at rest and under stress(11,12). Despite some limitations, MRI plays a significant role in the diagnosis of endometriosis, especially for allowing the identification of intermingled lesions in the presence of dense adhesions, and evaluation of sub–peritoneal lesions extent(4,13,14). In the evaluation of deep endometriosis, MRI presents accuracy, sensitivity and specificity > 90%(13,14). In the present iconographic essay, main MRI findings in deep pelvic endometriosis are described.
MRI PROTOCOLS The acquisition of appropriate magnetic resonance images for evaluating patients with suspected deep pelvic endometriosis must follow specific protocols. In our clinics, the examination is performed during menses, with a full bladder. Additionally, immediately before the examination, a venous antispasmodic agent (dipyrone, scopolamine butylbromide) is administered and, most recently, vaginal (50 ml) and rectal (100 ml) aqueous gel introduction has been adopted. The protocol includes the following sequences: axial T1–weighted, and sagittal, coronal and axial T2–weighted; and, after intravenous gadolinium injection, axial, fat–suppressed T1–weighted sequences.
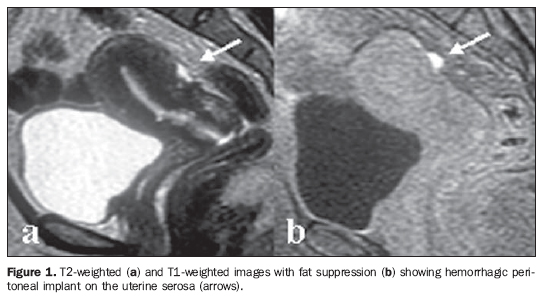
MRI FINDINGS Imaging findings on MRI of patients with deep pelvic endometriosis depend on the type of the lesion: small infiltrative endometrial implants, deep, solid lesions and visceral endometriosis involving the rectal and vesical walls(4). MRI may be a limited method in cases where the endometriosis presents with small infiltrative implants. Especially in cases where the lesions are visualized as whitish foci at laparoscopy, MRI may be negative. However, in some patients hyperintense foci may be characterized on fat–suppressed T1–weighted sequences, representing small areas of hemorrhage(4,13,14) (Figure 1).
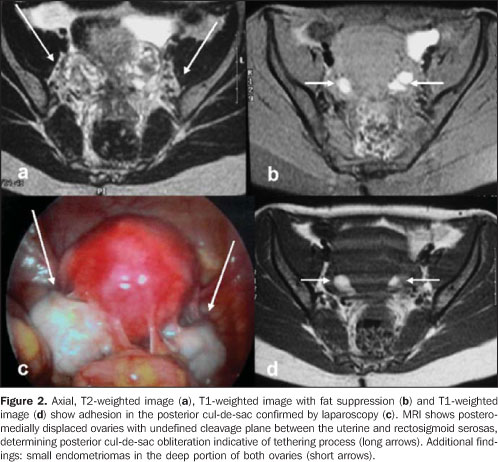
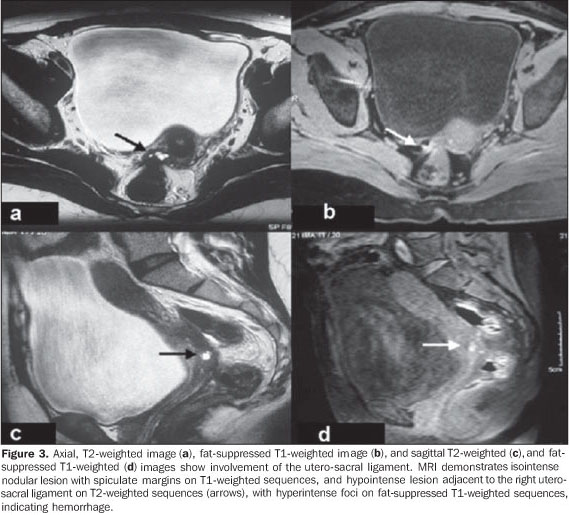
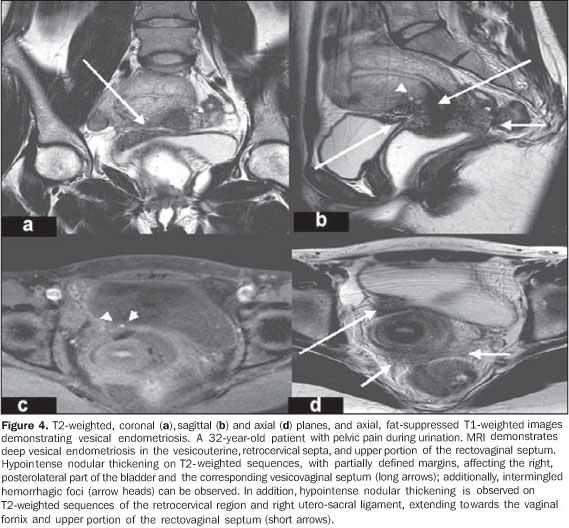
At MRI, deep, solid lesions affecting the posterior cul–de–sac (Figure 2) present low to intermediate intensity signal, with further hyperintense foci on fat–suppressed (blood) T1–weighted images, hyperintense signal on T2–weighted images with variable contrast–enhancement after intravenous gadolinium injection. Hypersignal foci on T1–weighted images result from ectatic endometrial glands with hemorrhagic content surrounded by fibrotic tissue. The extensive fibrosis component (Figure 3) generally characterized in the histological study of these lesions is responsible by the variable post–contrast–enhancement(4,7). Some foci of endometriosis localized in the Douglas cul–de–sac (Figure 4) may present with abundant glandular component with a mild fibrotic reaction. In these cases, high signal intensity is observed on T1–weighted images, and variable signal intensity on t2–weighted images, with the solid glandular component demonstrating variable contrast–enhancement after gadolinium injection(4,8,14). In cases where the utero–sacral ligaments are involved (Figure 5), subtle signal intensity alterations are found at MRI; findings such as bilateral or asymmetrical thickening and nodularity within these ligaments should be taken into consideration(4,8,14).
MRI may demonstrate focal or diffuse vesical involvement by endometriosis (Figure 6). The majority of patients present focal areas of parietal thickening with eventual hypersignal foci on fat–suppressed T1–weighted images. Invasion of the mucosa is not frequent in cases of vesical endometriosis and MRI can demonstrate alterations even in cases of asymptomatic patients with normal cystoscopy(4,8,13).
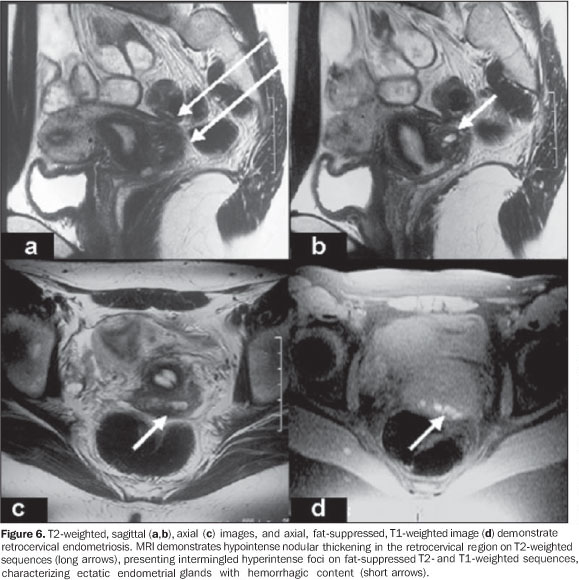
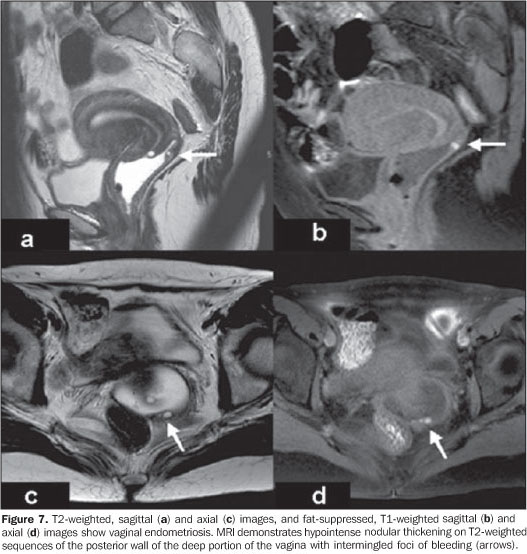
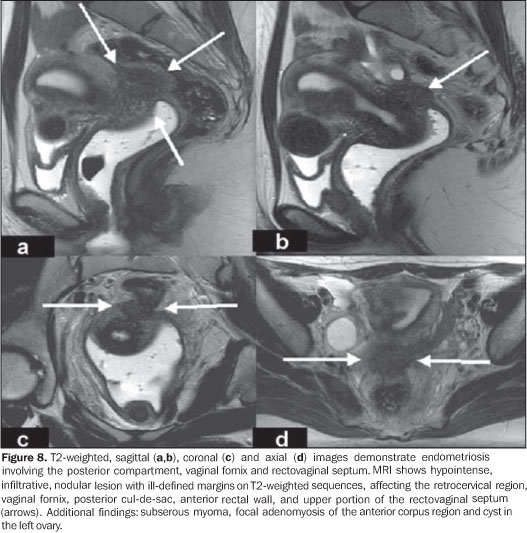
MRI sensitivity in the diagnosis of endometriosis with rectal involvement is relatively low, because of artifacts associated with the rectal content. In our practice, vaginal and rectal introduction of aqueous gel immediately before the examination may improve the MRI accuracy in the evaluation of rectal and retrocervical lesions (Figure 7), lesions in the rectovaginal septum (Figure 8), and in the vaginal wall. Rectal involvement generally is demonstrated by MRI as a parietal thickening with hypointense signal on T2–weighted images. Hyperintense hemorrhagic foci may be identified on fat–suppressed T1–weighted images(4,7,8,13).
CONCLUSION In patients with deep pelvic endometriosis, clinical and sonographic results may be normal or poorly elucidative, difficulting the diagnosis determination. In these cases, MRI is essential for an accurate differential diagnosis. MRI can evaluate areas otherwise inaccessible by laparoscopy, identifying and evaluating the extent of lesions in the sub–peritoneal region and in the presence of dense adhesions. Because of its multiplanar capacity and excellent tissue characterization, MRI plays an essential role in the preoperative evaluation of patients with deep pelvic endometriosis.
ACKNOWLEDGEMENTS The authors thank Dr. Cláudio Crispi, for kindly letting the author have the material utilized in the present study.
REFERENCES 1. Craig V. Endometriosis of the urinary tract. Urol Clin North Am. 2002;29:625–35. [ ] 2. Brandão A. Endometriose. In: Brandão A, Werner Jr H, Daltro P, editores. Ressonância magnética em obstetrícia e ginecologia. Rio de Janeiro: Revinter; 2003. p.133–50. [ ] 3. Kuligowska E, Deeds L, Lu K. Pelvic pain: overlooked and underdiagnosed gynecologic conditions. Radiographics. 2005;25:3–20. [ ] 4. Frate CD, Girometti R, Pittinno M, et al. Deep retroperitoneal pelvic endometriosis: MR imaging appearance with laparoscopic correlation. Radiographics. 2006;26:1705–18. [ ] 5. Zacharia TT, O'Neill MJ. Prevalence and distribution of adnexal findings suggesting endometriosis in patients with MR diagnosis of adenomyosis. Br J Radiol. 2006;104:303–7. [ ] 6. Crosignani P, Olive D, Bergqvist A, et al. Advances in the management of endometriosis: an update for clinicians. Hum Reprod. 2006;12: 179–89. [ ] 7. Bazot M, Darai E, Hourani R, et al. Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiology. 2004;232:379–89. [ ] 8. Woodward PJ, Sohaey R, Mezzetti Jr TP. Endometriosis: radiologic–pathologic correlation. Radiographics. 2001;21:193–216. [ ] 9. Olive DL, Schwartz LB. Endometriosis. N Engl J Med. 1993;328:1759–69. [ ] 10. Wykes CB, Clark TJ, Khan KS. Accuracy of laparoscopy in the diagnosis of endometriosis: a systematic quantitative review. Br J Obstet Gynaecol. 2004;111:1204–12. [ ] 11. Francisco VV, D'Ippolito G, Silva GPA, et al. Prevalência de artefatos em exames de ressonância magnética do abdome utilizando a seqüência GRASE: comparável com as melhores seqüências rápidas? Radiol Bras. 2005;38:323–8. [ ] 12. Bezerra MRL, Soares AFF, Faintuch S, et al. Identificação das estruturas músculo–ligamentares do assoalho pélvico na ressonância magnética. Radiol Bras. 2001;34:323–6. [ ] 13. Kinkel K, Chapron C, Balleyguier C, et al. Magnetic resonance imaging characteristics of deep endometriosis. Hum Reprod. 1999;14:1080–6. [ ] 14. Kataoka ML, Togashi K, Yamaoka T, et al. Posterior cul–de–sac obliteration associated with endometriosis: MR imaging evaluation. Radiology. 2005;234:815–23. [ ] Received August 9, 2007. Accepted after revision September 11, 2007. * Study developed at Clínica de Diagnóstico por Imagem (CDPI), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554