Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 1 - Jan. /Feb. of 2009
Vol. 42 nº 1 - Jan. /Feb. of 2009
|
REVIEW ARTICLE
|
|
Imaging diagnosis in snapping syndromes |
|
|
Autho(rs): Henrique Ribeiro da Silva, Marcelo Novelino Simão, Jorge Elias Júnior, Valdair Francisco Muglia, Marcello Henrique Nogueira-Barbosa |
|
|
Keywords: Joints, Snapping, Ultrasonography, Computed tomography, Magnetic resonance imaging |
|
|
Abstract:
IMD, Resident, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HC-FMRPUSP), Ribeirão Preto, SP, Brazil
INTRODUCTION Snapping syndrome corresponds to a group of changes that affect the limbs joints. Clinical presentation includes snapping during joints movement and may be associated with other clinical symptoms such as pain and, less frequently, neurological alterations(1,2). This is a challenging clinical condition, considering the wide range of causes, for example, tumors, anatomic abnormalities, loose intra-articular bodies, previous surgery or trauma, articular degeneration and inflammatory processes. These causes may be extra- or intra-articular. Snapping joints can be found with no association with other complaints and in these cases no treatment is required. The diagnosis is primarily based on the clinical history and physical examination of the patient. At clinical examination an audible snapping can be identified or a palpable prominence is observed, generally during specific maneuvers or when there is an attempt to reproduce the movements that result in complaint by the patient. Imaging diagnosis methods are utilized for confirming and documenting the anatomic structures or lesions associated, and can be useful for the management of the case, allowing the planning or choice of the an appropriate treatment. It is important to know the most frequent causes of this syndrome in the different joints to allow the choice of the appropriate imaging diagnosis method. Treatment, if required, is generally conservative. Eventually, surgery or arthroscopy may be required, and outcomes vary, depending on the etiology of the syndrome(3-10). The most frequent presentations of snapping syndromes in large limb joints will be discussed in the present review and the role played by the different imaging techniques in these cases is emphasized.
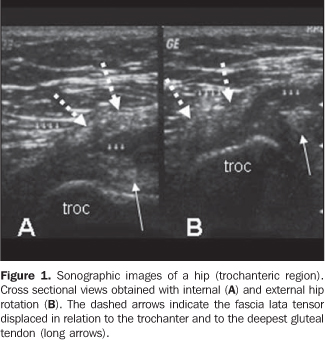
SNAPPING HIP The most frequently reported form of snapping syndrome occurs in hip, generally with extra articular causes(11-14). Many times, snapping hip syndrome, or coxa saltans, presents as an audible snapping or popping sound or palpable prominence associated with pain when the hip is flexed and extended. Medial snapping hip is related to the sudden displacement of the iliopsoas tendon over the iliopectineal eminence or adjacent bone structures. Lateral snapping hip is related to the sudden displacement of the tensor fascia lata or gluteus maximus over the greater trochanter of the femur. Sometimes the cause of the snapping may be related to intra-articular factors or lesions. Intra articular causes include loose bodies, synovial osteochondromatosis and acetabular labral tears(5,6,15). If further clinical investigation of snapping hip is indicated, plain radiography can be initially utilized for allowing identification of bone exostosis or articular and bone tumors, besides loose intra-articular bodies. In the past, iliopsoas tenography and bursography were utilized for allowing a dynamic study and characterization of sudden snapping of the iliopsoas tendon on fluoroscopic images(16). However, ultrasonography is currently a preferable method for being non-invasive and allowing a dynamic evaluation during maneuvers that trigger the snapping(17). Generally, plain radiography and ultrasonography are sufficient for investigating the majority of cases of extra-articular snapping hip. In these cases, ultrasonography is performed with high-frequency (5-12 MHz) linear transducers. Initially, the patient should be positioned in dorsal decubitus, with extended limbs, and subsequently, in lateral decubitus for evaluation of the anterior and lateral regions of the hip, including the greater trochanter and adjacent soft parts in the transverse and longitudinal planes. In the investigation of the medial snapping hip, the study should be focused on the iliopsoas and, in case of lateral snapping hip, on the fascia lata tensor muscle and gluteus maximus. Lateral snapping hip should also be evaluated with the transducer transversally placed over the greater trochanter (Figure 1), with the patient standing on the opposite leg. The movements that trigger the snapping must be reproduced by the patient both in dorsal decubitus and orthostatic positions. The presence or not of painful snapping should be evaluated during the examination.
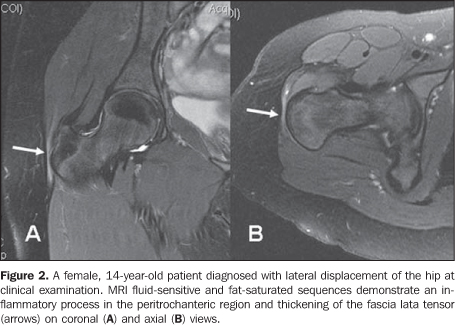
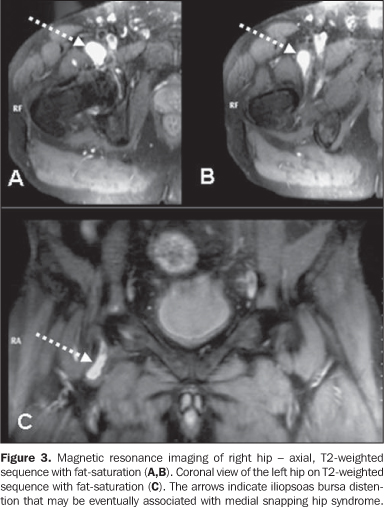
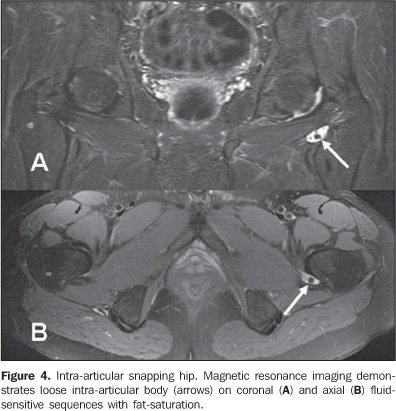
Medial snapping should be evaluated with the transducer transversally positioned or slightly oblique anteriorly over the hip joint, with the patient in dorsal decubitus, hip flexion with abduction and external rotation, in the frog position. Sectional imaging methods should be indicated if a diagnosis is not achieved by radiography and ultrasonography. Magnetic resonance imaging can eventually demonstrate inflammatory processes in the snapping tendon region or identifying a bursa probably associated with the snapping (Figures 2 and 3). Intra-articular snapping syndrome can be investigated by means of magnetic resonance imaging (Figure 4) or one of the sectional imaging methods preceded by arthrography: arthro-magnetic resonance imaging and arthro-computed tomography(15).
Treatment is usually clinical and conservative, most of times with good outcomes. Surgical management or arthroscopy is considered in cases where a good clinical response is not achieved, particularly in the presence of intra-articular causes(5,6,11,12,15).
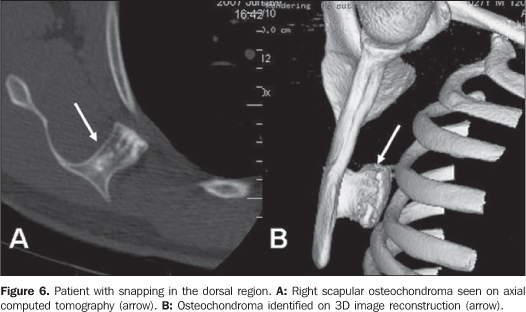
SNAPPING SCAPULA Palpable and, sometimes audible crepitation of the scapulo-thoracic joint should not always be considered as pathological. This is a relatively frequent and, most of times, painless alteration. Scapulocostal syndrome can be identified in overhead-throwing athletes(3). Some authors, however, have not found any direct relation between symptoms and type of activity, sports of postural alterations, and diagnosis is reported even in sedentary patients or in non-dominant limbs(18). The patients generally complain of pain with increase in activities involving the shoulder. One of the most consistent findings is crepitation with motion of the scapula. Inspection at clinical examination can demonstrate scapular asymmetry, and it is important to evaluate the minor pectoris, trapezium and elevator muscles in order to detect the presence of tension in these muscles of the affected side. Several bursae lying around represent potential causes of crepitation(3,8). Although elastofibromas (Figure 5), osteochondromas (Figure 6) and other tumors are reported as causes of this syndrome in the scapulothoracic region, associated lesions or tumors are not easily identified, and the cause may be dynamic and related to repetitive microtraumas, bursitis and anatomical variations(3,8,9,19,20).
The initial step for radiological investigation of scapula snapping syndrome is plain radiography to rule out obvious lesion of the scapula and ribs such as post-traumatic exostosis, osteochondromas or other expansile bone lesions. Fluoroscopy can be utilized to visualize the snapping during motion. If any bone abnormality that could explain the syndrome is not found, computed tomography and magnetic resonance imaging can better detect the presence of lesions of soft parts such as an inflamed bursa, a dorsal elastofibroma or infection. Magnetic resonance imaging has contrast resolution as its primary advantage to identify soft parts abnormalities, for example, inflammatory processes or hemorrhage in the involved bursa(9,18). Three-dimensional computed tomography can be utilized to evaluate the bone incongruity between the anterior aspect of the scapula and the chest wall(21). Elastofibroma is a non-neoplastic, reactive and rare type of lesion that is most frequently unilateral, although it can be unilateral or bilaterally found. Most frequently, this type of lesion is found deeply in relation to the rhomboid and great dorsal muscles, between the subscapular area and the chest wall. Because of this typical localization, this lesion is called dorsal elastofibroma. Typically, this lesion develops in mid-aged or elderly patients. Although it can be identified by ultrasonography and computed tomography, magnetic resonance imaging, if available, should be the method of choice. Magnetic resonance imaging may suggest a presumptive diagnosis, particularly in cases where the lesion is found in the most typical site, i.e., the infrascapular region, and especially when demonstrates a fibrotic and fatty content. The definite diagnosis is achieved by means of histopathologic study. The treatment of snapping scapula is generally clinical and conservative, the latter including the utilization of anti-inflammatory drugs, local analgesia, judicious utilization of corticosteroid infiltration and, mainly, muscular rehabilitation. In cases where no clinical improvement is observed in three to six months, surgical management may be considered(3,8,9,18). Surgical resection may be required in cases where an elastofibroma or osteochondroma is identified.
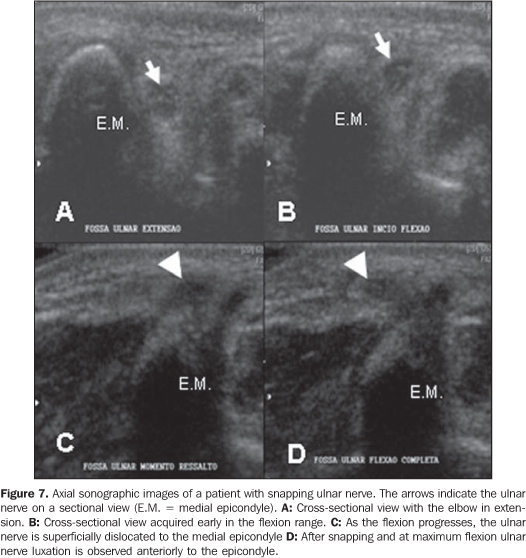
SNAPPING ELBOW Snapping elbow syndrome is a less frequent clinical entity, and as such, is poorly recognized. The snapping elbow may progress with no other manifestation such as pain and neurological symptoms(1,2,6,7). Several causes are reported, the most frequent one being the elbow relationship with medial anatomical structures. Other causes include inflammatory processes and anatomical alterations, particularly cubitus varus deformity, that may result in displacement of the ulnar nerve in combination or not with dislocation of the medial head of the triceps over the medial epicondyle with elbow flexion(1,2,4,22). Most frequently, ultrasonography and magnetic resonance imaging are indicated for snapping elbow investigation(2,4,22). Ultrasonography (Figure 7), may be preferred because of its wide availability and dynamic evaluation capability, and should be performed with a 7.0 MHZ (at minimum) linear transducer. Before ultrasonography, the olecranon and the medial epicondyle should be palpated with the limb in extension with subtle supination. The transducer must be placed on the axis between these structures, for identification and measurement of the sectional area of the ulnar nerve inside its groove. Subsequently, the patient should be asked to flex the elbow with the transducer in the same position, and the diagnosis of the dislocation is made as the ulnar nerve passes the medial epicondyle apex, in association or not with displacement of the medial head of the triceps(2). The flexion against resistance facilitates the diagnosis and should be utilized. In some cases, passive or active dynamic studies without counter-resistance may not reproduce the snapping. With magnetic resonance imaging, the sequences should be acquired with the limb at maximum extension and flexion for evaluation of the initial and end positions of the ulnar nerve and medial head of the triceps(4,22).
It is very important for the radiologist to differentiate an isolate displacement of the ulnar nerve from a combination with dislocation of the medial head of the triceps(2). A considerable number of patients with snapping ulnar nerve are asymptomatic or at least do not require surgical management. However, the symptoms may persist after surgery, if a surgical transposition of the ulnar nerve is indicated, and association with dislocation of the medial head of the triceps has not been identified. Lateral snapping of the elbow is much less frequently found and may be associated with poster lateral rotator instability, a menisci interposition with the radiohumeral joint, snapping annular ligament over the radial head or even a lateral displacement of the distal triceps(1,23-25).
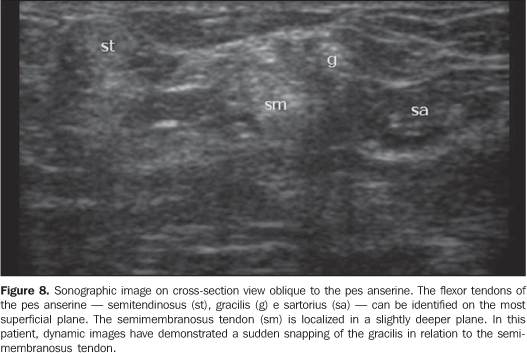
SNAPPING KNEE In the knee, the snapping syndrome is most frequently associated with traumatic or non-traumatic meniscal lesions. Lateral discoid meniscus, which is the most frequently found abnormality of children, may be the cause, particularly the lateral discoid meniscus type III or Wrisberg's ligament. This rare alteration occurs when the posterior fixation between the meniscus and the tibia is absent with a significantly higher meniscal mobility(7,26). Other less frequent causes, such as tendon dislocation and intra-articular tumors have also been described(10,26-28). Investigation with imaging methods should be initiated with conventional radiology. Evaluation of snapping tendons may be performed with ultrasonography (Figure 8). On the other hand, the utilization of magnetic resonance imaging should be encouraged if an intra-articular lesion is suspected. Arthroscopy, despite its invasiveness, can also be utilized(7,26). The treatment must be individualized, and can be clinical, by arthroscopy or open surgery, as the case requires(7,10,26-28).
SNAPPING ANKLE Snapping ankle is rare and may be associated with subluxation or luxation of the tendon. Most rarely, it is reported in association with intra-articular bodies. Among reports in the literature, the most frequently found situation is luxation or subluxation of fibular tendons, with or without concurrent tendineal rupture(29). In most of recorded cases, this abnormality is found in athletes or dancers. Flattened or convex fibular groove is mentioned by the literature as a predisponent factor for luxation of fibular tendons, but the majority of cases is reported after trauma. Luxation may be diagnosed in patients with acute or chronic presentations. The dynamic evaluation of fibular tendons by ultrasonography should be performed with cross-sectional views on the retromalleolar region and the tendons are observed during passive or active foot flexion and eversion. A recently published casuistic reports 14 cases of intrasheath subluxation of peroneal tendons, and in this case the tendons remain in the retromalleolar region, but transitorily switch their relative positions with a reproducible painful click(30). Most rarely, snapping syndrome can also be caused by a third fibular tendon(31) or being related to the posterior tibial tendon(32), in this latter case, with medial snapping. In a systematic literature review(32) published in 2008, the authors observed that 58.5% of lesions with luxation of the posterior tibial tendon were caused by sports trauma, and 53.1% of all the cases with luxation of the posterior tibial tendon have initially remained without a correct diagnosis. The authors have also observed that 35.6% of the patients experienced recurrent snapping of the tendon. Surgical management with different techniques was the most frequent approach adopted (83.1%) and outcomes were considered as excellent and asymptomatic in 80% of cases and good in other 12%. Like in other joints, the investigation of snapping of superficial tendons can be effectively performed by ultrasonography. Computed tomography and magnetic resonance imaging (Figure 9) can statically demonstrate luxation or subluxation and also allow the evaluation of the fíbula or other lesions that may be associated.
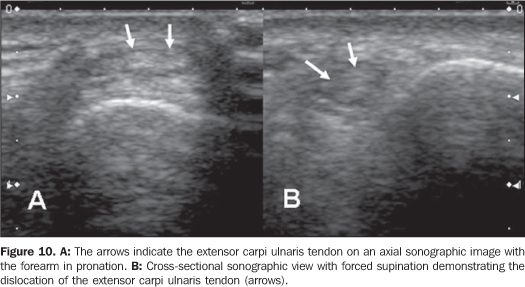
SNAPPING WRIST Cases of snapping wrist syndrome have been rarely reported. Tumors, loose articular bodies, and dislocation of tendons can cause snapping(30,33-35). Also, another study describes a case of snapping of superficial flexor tendon of the fifth finger over the hamate hook after surgical carpal tunnel decompression(36). Instability of the extensor carpi ulnaris tendon may cause snapping during subluxation and luxation and has been reported as the most frequent cause of snapping of the wrist. The evaluation of this condition can be performed by means of ultrasonography (Figure 10). This condition may eventually be clinically confused or being concurrent with subluxation of the distal radioulnar joint. In rheumatoid arthritis, the tendon may dislocate towards the volar region, while ulnar subluxation may occur posteriorly to the distal radioulnar joint.
In normal wrists there is a certain acceptable degree of subluxation of the extensor carpi ulnaris tendon as related to its osseous groove(37). The literature reports normality values for this dislocation in terms of percentage of the width of the tendon's osseous groove. The tendon may displace by up to 40% of the osseous groove width towards the volar region with wrist flexion, and towards the dorsal region up to 33% with wrist extension. Generally, the traumatic mechanism that causes subluxation of the extensor carpi ulnaris tendon corresponds to forced supination, palmar flexion and ulnar dislocation. With the pronation, the tendon generally returns to its usual position. Magnetic resonance imaging can characterize the inflammatory process in the synovial sheath and, eventually, the inappropriate positioning of the tendon. Acute subluxation has been rarely reported in the literature, and can be managed with immobilization in pronation and a slight radial deviation of the wrist. Surgical reconstruction may be required in cases of symptomatic and chronic subluxation.
CONCLUSION Snapping syndrome is a challenging clinical condition with several causes and relatively poorly commented. In most of cases, it is characterized by mild clinical manifestations, but eventually the syndrome may cause a significant physical limitation. It may be difficult to define a diagnosis because of the absence of knowledge on the nature of this syndrome. The knowledge on this syndrome is relevant for guiding in the selection of the appropriate imaging method. The present review discusses the main causes of this syndrome and indicates the most appropriate diagnostic methods according to the joint involved and the clinical suspicion.
REFERENCES 1. Spinner RJ, An KN, Kim KJ, et al. Medial or lateral dislocation (snapping) of a portion of the distal triceps: a biomechanical, anatomic explanation. J Shoulder Elbow Surg. 2001;10:561-7. [ ] 2. Jacobson JA, Jebson PJL, Jeffers AW. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography - report of three cases. Radiology. 2001;220:601-5. [ ] 3. Manske RC, Reiman MP, Stovak ML. Nonoper-ative and operative management of snapping scapula. Am J Sports Med. 2004;32:1554-65. [ ] 4. Spinner RJ, Goldner RD. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J Bone Joint Surg Am. 1998;80:239-47. [ ] 5. White RA, Hughes MS, Burd T, et al. A new operative approach in the correction of external coxa saltans: the snapping hip. Am J Sports Med. 2004; 32:1504-8. [ ] 6. Provencher MT, Hofmeister EP, Muldoon MP. The surgical treatment of external coxa saltans (the snapping hip) by Z-plasty of the iliotibial band. Am J Sports Med. 2004;32:470-6. [ ] 7. Kelly BT, Green DW. Discoid lateral meniscus in children. Curr Opin Pediatr. 2002;14:54-61. [ ] 8. Nicholson GP, Duckworth MA. Scapulothoracic bursectomy for snapping scapula syndrome. J Shoulder Elbow Surg. 2002;11:80-5. [ ] 9. Majó J, Gracia I, Doncel A, et al. Elastofibroma dorsi as a cause of shoulder pain or snapping scapula. Clin Orthop Relat Res. 2001;(388):200-4. [ ] 10. Cooper DE. Snapping popliteus tendon syndrome. A cause of mechanical knee popping in athletes. Am J Sports Med. 1999;27:671-4. [ ] 11. Pelsser V, Cardinal E, Hobden R, et al. Extraartic-ular snapping hip: sonographic findings. AJR Am J Roentgenol. 2001;176:67-73. [ ] 12. Choi YS, Lee SM, Song BY. Dynamic sonography of external snapping hip syndrome. J Ultrasound Med. 2002;21:753-8. [ ] 13. Janzen DL, Partridge E, Logan PM, et al. The snapping hip: clinical and imaging findings in transient subluxation of the iliopsoas tendon. Can Assoc Radiol J. 1996;47:202-8. [ ] 14. Costa FP, Canto RST. Quadril em ressalto. Rev Bras Ortop. 1990;25:369-72. [ ] 15. Wunderbaldinger P, Bremer C, Matuszewski L. Efficient radiological assessment of the internal snapping hip syndrome. Eur Radiol. 2001;11: 1743-7. [ ] 16. Staple TW, Jung D, Mork A. Snapping tendon syndrome: hip tenography with fluoroscopic monitoring. Radiology. 1988;166:873-4. [ ] 17. Cardinal E, Buckwalter KA, Capello WN, et al. US of the snapping iliopsoas tendon. Radiology. 1996;198:521-2. [ ] 18. Carrera EF, Matsumoto MH, Archetti Netto N, et al. Elastofibroma dorsi: relato de casos e revisão da literatura. Rev Bras Ortop. 2004;39:468-75. [ ] 19. Edelson JG. Variations in the anatomy of the scapula with reference to the snapping scapula. Clin Orthop Relat Res. 1996;(322):111-5. [ ] 20. Hayes AJ, Alexander N, Clark MA, et al. Elasto-fibroma: a rare soft tissue tumour with a pathognomonic anatomical location and clinical symptom. Eur J Surg Oncol. 2004;30:450-3. [ ] 21. Mozes G, Bickels J, Ovadia D, et al. The use of three-dimensional computed tomography in evaluating snapping scapula syndrome. Orthopedics. 1999;22:1029-33. [ ] 22. Yiannakopoulos CK. Imaging diagnosis of the snapping triceps syndrome. Radiology. 2002;225: 607-8. [ ] 23. Huang GS, Lee CH, Lee HS, et al. A meniscus causing painful snapping of the elbow joint: MR imaging with arthroscopic and histologic correlation. Eur Radiol. 2005;15:2411-4. [ ] 24. Mehta JA, Bain GI. Posterolateral rotatory instability of the elbow. J Am Acad Orthop Surg. 2004; 12:405-15. [ ] 25. Aoki M, Okamura K, Yamashita T. Snapping annular ligament of the elbow joint in the throwing arms of young brothers. Arthroscopy. 2003;19: E4-7. [ ] 26. Mine T, Ihara K, Taguchi T, et al. Snapping knee caused by intra-articular tumors. Arthroscopy. 2003;19:E21. [ ] 27. Lokiec F, Velkes S, Schindler A, et al. The snapping biceps femoris syndrome. Clin Orthop Relat Res. 1992;(283):205-6. [ ] 28. Bae DK, Kwon OS. Snapping knee caused by the gracilis and semitendinosus tendon. A case report. Bull Hosp Jt Dis. 1997;56:177-9. [ ] 29. Arrowsmith SR, Fleming LL, Allman FL. Traumatic dislocations of the peroneal tendons. Am J Sports Med. 1983;11:142-6. [ ] 30. Raikin SM, Elias I, Nazarian LN. Intrasheath subluxation of the peroneal tendons. J Bone Joint Surg Am. 2008;90:992-9. [ ] 31. Sammarco GJ, Henning C. Peroneus tertius muscle as a cause of snapping and ankle pain: a case report. Am J Sports Med. 2007;35:1377-9. [ ] 32. Lohrer H, Nauck T. Posterior tibial tendon dislocation. A systematic review of the literature and presentation of a case. Br J Sports Med. 2008 Jan 16 Epub ahead of print. [ ] 33. Zachee B, DeSmet L, Fabry G. A snapping wrist due to a loose body. Arthroscopic diagnosis and treatment. Arthroscopy. 1993;9:117-8. [ ] 34. Rupnik E, Szloboda J. "Snapping wrist" caused by tumor of the flexor tendon. Magy Traumatol Orthop Helyreallito Seb. 1991;34:57-8. [ ] 35. Renard M, Simonet J, Bencteux P, et al. Intermittent dislocation of the flexor hallucis longus tendon. Skeletal Radiol. 2003;32:78-81. [ ] 36. Itsubo T, Uchiyama S, Takahara K, et al. Snapping wrist after surgery for carpal tunnel syndrome and trigger digit: a case report. J Hand Surg [Am]. 2004;29:384-6. [ ] 37. Pratt RK, Hoy GA, Bass Franzcr C. Extensor carpi ulnaris subluxation or dislocation? Ultrasound measurement of tendon excursion and normal values. Hand Surg. 2004;9:137-43. [ ] Received June 8, 2008. * Study developed at Unit of Radiodiagnosis, Center of Imaging Sciences and Medical Physics - Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (CCIFM/HC-FMRPUSP), Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554