Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 55 nº 1 - Jan. /Feb. of 2022
Vol. 55 nº 1 - Jan. /Feb. of 2022
|
ICONOGRAPHIC ESSAY
|
|
Cerebral venous thrombosis: imaging patterns |
|
|
Autho(rs): Isabela Magalhães Oliveira1,a; Juliana Ávila Duarte2,b; Mariana Dalaqua3,c; Vinicius Menezes Jarry1,d; Fernanda Veloso Pereira1,e; Fabiano Reis1,f |
|
|
Keywords: Intracranial venous thrombosis/diagnostic imaging; Tomography, X-ray computed; Magnetic resonance imaging. |
|
|
Abstract: INTRODUCTION
Cerebral venous thrombosis (CVT) is defined as the presence of a thrombus within a venous sinus, superficial intracranial vein, or deep intracranial vein. It is an uncommon condition that is potentially reversible if diagnosed and treated appropriately and promptly. It typically affects young females, correlating with common prothrombotic states (such as Behçet’s disease), the use of oral contraceptives, adjacent infections, trauma, intracranial hypotension, and the peripartum period. Because patients with CVT can present with a wide spectrum of nonspecific manifestations, including headache, focal neurologic deficits, seizures, and decreased level of consciousness, the condition is difficult to diagnose clinically. Consequently, imaging is fundamental to its diagnosis. Therefore, radiologists should be able to recognize this condition, allowing appropriate treatment (anticoagulation therapy), which can reverse the disease process as well as significantly reducing the risk of acute complications and long-term sequelae(1,2). The goals of this article are to illustrate the anatomy of the cerebral venous system (Figure 1); describe the various CVT subtypes; review the main imaging findings of CVT and associated parenchymal abnormalities; highlight the predisposing factors for CVT; and demonstrate the diagnostic pitfalls. The cases presented are from the radiology departments of the participating institutions. 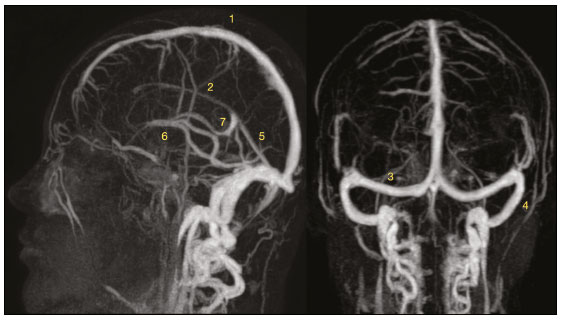 Figure 1. Intracranial contrast-enhanced MR venogram showing the anatomy of the cerebral venous system, consisting of the deep venous system, superficial venous system, and dural venous sinuses (with superior and inferior components). The superior dural sinuses comprise the superior sagittal sinus (1), the inferior sagittal sinus (2) and the straight sinus (5)—which converge at the torcular herophili—as well as the transverse sinus (3) and sigmoid sinus (4). The inferior dural sinuses comprise the cavernous sinuses, which are connected through the anterior and posterior intercavernous sinuses, and the superior and inferior petrosal sinuses, which drain toward the sigmoid sinus and jugular bulb. The deep system includes the vein of Galen (7), the internal cerebral veins (6), and their tributaries; the Rosenthal veins (basal veins) and its tributaries; and the medullary and subependymal veins, which drain the hemispheric white matter. PREDISPOSING FACTORS There is a wide range of causes and risk factors associated with CVT. Causal factors may be local (related to intrinsic or mechanical conditions of the venous system) or systemic (related to prothrombotic states). Local processes that alter venous flow include sinus trauma, regional infection, and neoplastic invasion or compression. Systemic causes include protein S and protein C deficiencies, as well as a peripartum state, oral contraceptive use, and malignancy. In as many as 25% of cases, no cause is identified(3). CLINICAL MANIFESTATIONS The clinical manifestations of CVT vary depending on the extent, location, and time since the onset of the venous thrombotic process, as well as on the venous collateral circulation. They fall broadly into three categories: signs and symptoms of raised intracranial pressure; a focal brain lesion; and a combination of the two. Headache is the most common symptom, although seizures and focal neurological manifestations may also be observed. The time from the onset of the process to the appearance of symptoms varies widely(4): 2–30 days (subacute presentation) is the most common range, followed by < 2 days (acute presentation) and > 30 days (chronic presentation). BEST IMAGING MODALITY It is well established that the current gold standard to depict CVT is the combination of conventional magnetic resonance imaging (MRI) with some kind of magnetic resonance venography, particularly with dynamic time-resolved angiographic techniques, such as time-resolved imaging of contrast kinetics (TRICKS) and time-resolved imaging with stochastic trajectories. The TRICKS modality uses extremely rapid acquisitions to provide dynamic images of intravascular contrast flow. The use of TRICKS provides excellent spatial resolution, as well as dynamic flow information that has not been previously obtained without more invasive studies, such as interventional angiography(5). The combination of conventional MRI and TRICKS demonstrates the location and extent of the thrombus, as well as the patent venous drainage pathways, the temporal evolution of the thrombosis, and associated brain abnormalities(6). IMAGING FINDINGS The imaging findings of CVT are related not only to the actual intraluminal thrombosis but also to the consequences of the obstructed venous drainage, such as parenchymal disturbances due to venous congestion and parenchymal or subarachnoid hemorrhage, as well as late-phase complications. Unenhanced CT Direct signs of CVT are seen in only one third of cases and are rarely visible on unenhanced CT scans. The “cord sign” (Figure 2) represents direct visualization of an acute hyperdense thrombus. More often, unenhanced CT shows only indirect signs of CVT, which may include diffuse brain edema and venous infarction(1,6). 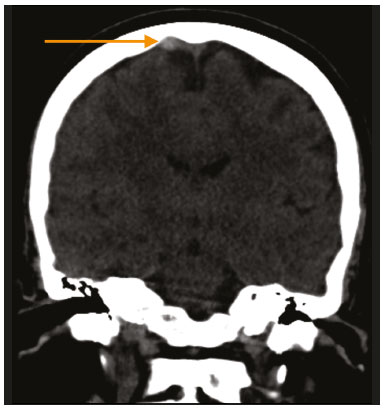 Figure 2. Coronal reconstruction of an unenhanced CT image showing hyperattenuation in the occluded cortical vein—the so-called “cord sign” (arrow). Contrast-enhanced CT Direct evidence of CVT on contrast-enhanced CT includes the “empty delta sign”, which consists of a triangular area of contrast enhancement in the dural sinus surrounding the hypodense thrombus. CT venography In cases of CVT, direct visualization of the thrombus as a filling defect can be achieved with CT venography. MRI On conventional MRI sequences, patent dural sinuses often appear as a flow void, due to the normal fast flow, whereas CVT may manifest as the absence of a flow void, which is often best seen on T2/fluid-attenuated inversion recovery (FLAIR) images. However, it should be emphasized that this finding is not specific for thrombosis and may be associated with transient hemodynamic conditions of slow flow, without thrombosis. On T1-weighted imaging (T1WI), a thrombus with methemoglobin is hyperintense in the subacute phase. The use of susceptibility-weighted imaging improves the detection of acute-phase CVT because magnetic susceptibility of deoxyhemoglobin makes dural sinus CVT hypointense(1,6). On diffusion-weighted imaging, an increased signal corresponding to the presence of intravascular clots may be depicted, even in the absence of parenchymal lesions. The corresponding low apparent diffusion coefficient suggests restriction of the movement of water molecules (i.e., restricted diffusion) at the site of occlusion (Figure 3). 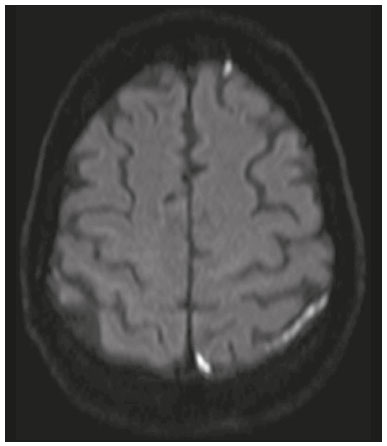 Figure 3. Axial diffusion-weighted image showing hyperintensities in cortical veins. An apparent diffusion coefficient map (not shown) confirmed true restricted diffusion. MR venography The modality known as MR venography may be performed with or without the use of a contrast agent. Time-resolved contrast-enhanced MR venography has the highest accuracy and takes advantage of luminal filling by contrast material rather than relying on the MR flow phenomena using the time-of-flight technique. Parenchymal abnormalities In CVT, vasogenic and cytotoxic edema may be observed and are occasionally seen together. Like intraparenchymal hemorrhage, they can be located in subcortical territories, rather than in the typical arterial vascular distribution. Vasogenic edema, which may be reversible, develops secondary to elevated retrograde venous pressure (Figure 4), whereas cytotoxic edema appears if the cerebral perfusion pressure decreases and provokes tissue distress. Hemorrhages in the frontal and parietal lobes are often associated with superior sagittal sinus CVT (Figure 5), whereas those in the temporal and occipital lobes are more characteristic of transverse sinus CVT. In rare cases, CVT can be accompanied by subarachnoid hemorrhage (Figure 6) in the subacute phase. The pathogenic mechanism is venous hypertension secondary to retrograde pressure due to blocked cerebral venous system, resulting in bleeding into the subarachnoid space(7). 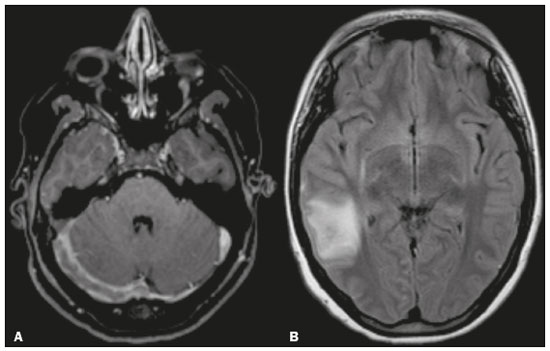 Figure 4. A 23-year-old woman with refractory headache. A: Axial MR angiogram showing a lack of flow in the enlarged right transverse sinus. B: Axial FLAIR MRI scan showing hyperintensity in the posterior right temporal lobe, consistent with vasogenic edema of a venous infarct. 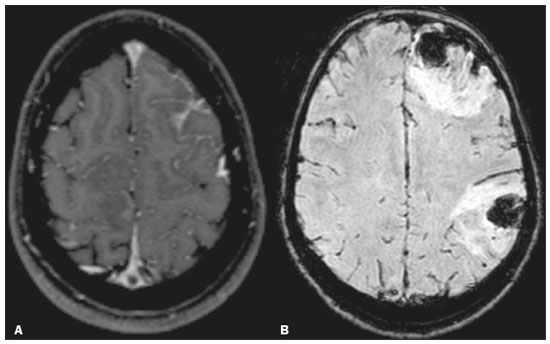 Figure 5. A 15-year-old female patient with CVT. A: Axial contrastenhanced three-dimensional T1-weighted magnetization prepared rapid gradient echo MRI sequence showing a central triangular filling defect (“empty delta sign”) in the superior sagittal sinus. B: Axial susceptibility-weighted MRI showing intraparenchymal hemorrhages in A B the frontal and parietal lobes. 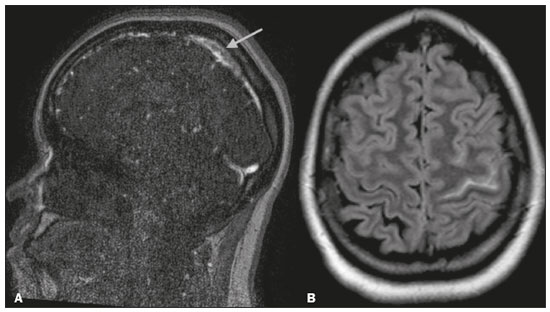 Figure 6. A 20-year-old woman with right-sided headache and hypoesthesia. A: Sagittal MR angiogram showing a lack of flow in the superior sagittal sinus (arrow). B: Axial FLAIR MRI scan showing subarachnoid hemorrhage in the left central A B sulcus. SUBTYPES OF CVT Dural sinus thrombosis In most patients with CVT, multiple dural venous sinuses are involved. Those most commonly affected are the superior sagittal sinus, transverse sinus, and sigmoid sinus(1). Isolated cortical vein thrombosis Isolated cortical vein thrombosis is a relatively rare entity. Typical parenchymal findings are areas of focal cortical edema or hemorrhage, which may be nonspecific. On MR venography, an asymmetric absence of flow signal or reduced enhancement can be seen in the thrombosed cortical veins(3). Deep CVT Deep CVT is defined as thrombosis of the superior striate veins(8), thalamostriate veins, internal cerebral veins, vein of Galen, or straight sinus. Thalamic involvement is the imaging hallmark of this condition, and it may involve the caudate nucleus and deep white matter (Figure 7)(3). 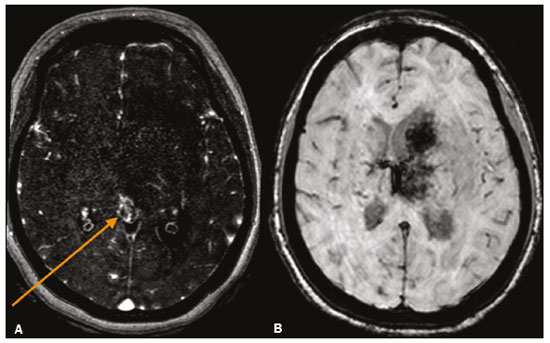 Figure 7. A 27-year-old woman with deep CVT. A: MR venogram showing a lack of flow in the internal cerebral veins (arrow), vein of Galen, and straight sinus (not demonstrated). B: Axial susceptibility-weighted MRI scan showing hemorrhagic transformation of a venous infarct in the left head of the caudate nucleus and thalamus. Chronic CVT Chronic CVT with incomplete recanalization may present a diagnostic challenge on MRI. Although the thrombus typically has a signal that is isointense on T1WI and isointense/hyperintense on T2WI, there is significant variability in the signal intensity. Other findings that may be seen on MR venography are an irregular appearance of the sinus, with multiple serpiginous intrathrombus flow voids and dural collateral vessels, which are characteristics of incomplete recanalization(4). One major complication of chronic venous thrombosis is dural arteriovenous fistula (Figure 8). On follow-up imaging, radiologists should look for dilated cortical arteries and veins in the surrounding affected parenchyma, which may be related to arterial recruiting and venous hypertension, respectively(9). 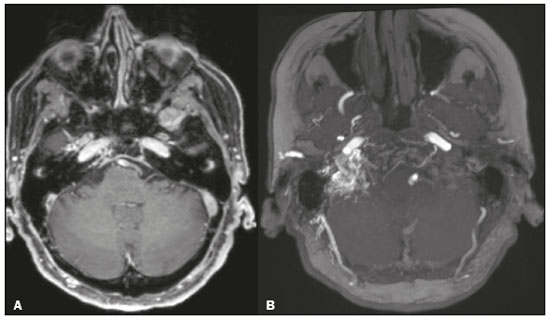 Figure 8. A 75-year-old female patient who underwent MRI for investigation of vertigo of undetermined origin. A: Axial contrast-enhanced three-dimensional (3D) T1-weighted magnetization prepared rapid gradient echo MRI sequence showing a filling defect in the transition between the right transverse and sigmoid venous sinuses. B: Axial maximum intensity projection reformatting of an unenhanced 3D time-of-flight MR angiogram, showing prominence of the right occipital and middle meningeal arteries, as well as branches of the right vertebral and ascending pharyngeal arteries (not shown) supplying a dural arteriovenous fistula consequent to chronic CVT with incomplete recanalization. PREDISPOSING FACTORS FOR CVT Adjacent infections Otitis, mastoiditis, sinusitis, and meningitis can lead to CVT. Mastoiditis is the most common temporal bone infection and may cause septic thrombosis due to suppurative direct spread, sometimes requiring surgical intervention. Infection may also induce increased production of procoagulant compounds, resulting in a prothrombotic state and leading to dural venous sinus thrombosis (Figure 9). 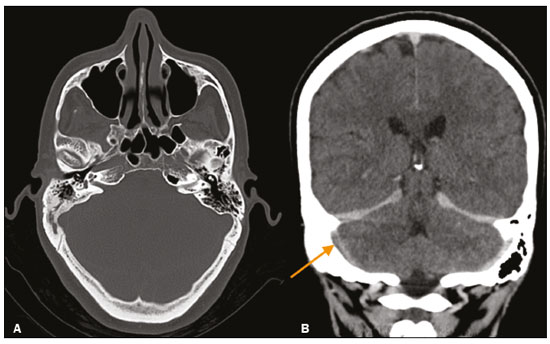 Figure 9. A 52-year-old woman complaining of holocranial headache. A: Axial CT scan showing opacification of some right mastoid air cells associated with bone sclerosis, indicative of chronic mastoiditis. B: Coronal CT angiogram showing a filling defect in the ipsilateral transA B verse sinus (arrow). Prothrombotic states Rheumatologic diseases such as systemic lupus erythematosus and Behçet’s disease may induce CVT. Behçet’s disease is a chronic, multisystem, relapsing inflammatory perivasculitis. Although neurological involvement (neuro-Behçet’s disease) is a rare manifestation, it is one of the most serious causes of long-term morbidity and can result in cerebral venous thrombosis(10,11), as depicted in Figure 10. 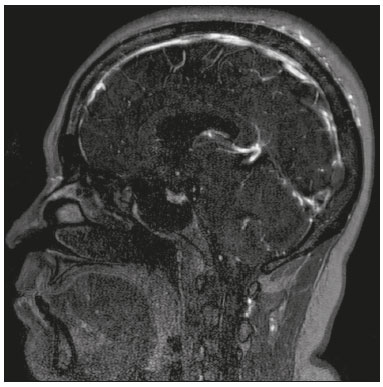 Figure 10. A 43-year-old woman with Behçet’s disease and persistent headache. Sagittal MR venogram showing a lack of flow in the torcular herophili. Prior trauma or surgery It is known that CVT is an underdiagnosed complication of trauma (Figure 11) and surgery. The prevalence of CVT is much higher in patients with skull fractures adjacent to a venous sinus, regardless of age group. Because the occurrence of traumatic CVT is usually not immediate, early imaging can miss that. In this context, contrast-enhanced follow-up CT or MR angiography is important to distinguish true thrombosis from sinus narrowing or occlusion caused by a compressing epidural hematoma(12). 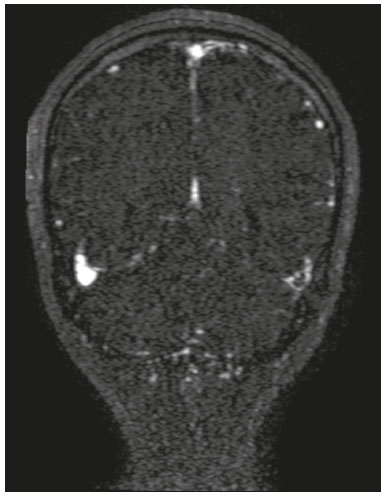 Figure 11. A 40-year-old man with a closed head injury and skull fractures who presented with a three-day history of a decreased level of consciousness. An unenhanced axial CT scan (not depicted) showed a hyperdense thrombus in the left transverse sinus. A coronal MR venogram (depicted) confirmed the corresponding lack of venous flow. Intracranial hypotension syndrome Intracranial hypotension syndrome consists of decreased cerebrospinal fluid volume, resulting in compensatory distention of vessels and downward traction of richly innervated structures. Dural venous sinus and cortical vein thrombosis have been described as uncommon complications of intracranial hypotension syndrome (Figure 12) and are believed to be secondary to slow blood flow in a dilated dural sinus. The risk of the syndrome is increased in patients with thrombotic preconditions(13,14). 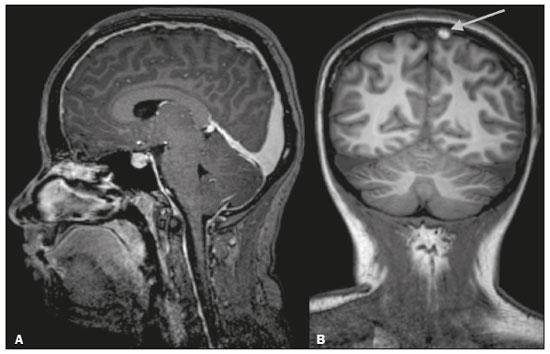 Figure 12. Cortical CVT in a 22-yearold woman who developed intracranial hypotension after epidural anesthesia. A: Sagittal contrast-enhanced three-dimensional T1WI showing dilated venous sinuses and enlargement of the pituitary gland (findings typical of intracranial hypotension). B: Unenhanced coronal T1WI showing a hyperintense thrombus in a cortical vein (arrow). DIAGNOSTIC PITFALLS There are pitfalls associated with all imaging techniques. Anatomical variations Sinus asymmetry is mainly observed in the transverse sinuses. If the corresponding jugular foramen is also small, a narrow sinus may be considered a normal anatomical variation(15). Arachnoid granulations Arachnoid granulations are common projections of the subarachnoid space into a sinus, usually round and not occupying the entire sinus like CVT does. Increased hematocrit levels In newborns with persistence of fetal hemoglobin and in situations such as dehydration and polycythemia, the sinuses and veins may appear relatively hyperdense on unenhanced CT, due to increased hematocrit levels. However, in such cases, the arteries will have a similar appearance(15). Diffuse brain edema Parenchymal hypodensity caused by diffuse brain edema may also make the venous structures appear relatively hyperdense on CT. Flow artifacts on MRI Slow flow leads to inconsistent flow void(15). Another flow pitfall is the “entry section phenomenon”, which is a flow-related enhancement artifact dependent on flow direction. Contrast-enhanced studies clarify the diagnosis. CONCLUSION Albeit relatively uncommon, CVT is a potentially life-threatening disease. Imaging plays a crucial role in the diagnosis and identification of the patterns of CVT. Radiologists should be aware of the potential pitfalls in order to avoid misdiagnosis and allow early treatment, which is essential to decrease the rate of complications—such as dural arteriovenous fistula—and sequelae. REFERENCES 1. Canedo-Antelo M, Baleato-González S, Mosqueira A J, et al. Radiologic clues to cerebral venous thrombosis. Radiographics. 2019;39: 1611–28. 2. Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352:1791–8. 3. Leach JL, Fortuna RB, Jones BV, et al. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics. 2006;26 Suppl 1:S19–41. 4. Behrouzi R, Punter M. Diagnosis and management of cerebral venous thrombosis. Clin Med (Lond). 2018;18:75–9. 5. Kahana A, Lucarelli MJ, Grayev AM, et al. Noninvasive dynamic magnetic resonance angiography with time-resolved imaging of contrast kinetics (TRICKS) in the evaluation of orbital vascular lesions. Arch Ophthalmol. 2007;125:1635–42. 6. Idbaih A, Boukobza M, Crassard I, et al. MRI of clot in cerebral venous thrombosis: high diagnostic value of susceptibility-weighted images. Stroke. 2006;37:991–5. 7. Hassan A, Ahmad B, Ahmed Z, et al. Acute subarachnoid hemorrhage. An unusual clinical presentation of cerebral venous sinus thrombosis. Neurosciences (Riyadh). 2015;20:61–4. 8. Mazini B, Bonvin C, Gailloud P, et al. Isolated superior striate vein thrombosis in adults. Interv Neuroradiol. 2020;26:446–50. 9. Gupta A, Periakaruppan A. Intracranial dural arteriovenous fistulas: a review. Indian J Radiol Imaging. 2009;19:43–8. 10. Vieira RM, Nascimento FBP, Barbosa Júnior AA, et al. Spectrum of central nervous system involvement in rheumatic diseases: pictorial essay. Radiol Bras. 2018;51:262–7. 11. Sorgun MH, Rzayev S, Kural MA, et al. Cerebral venous thrombosis in Behçet’s disease patients compared to other causes of cerebral venous thrombosis: a retrospective study. Arch Rheumatol. 2016;31:248–53. 12. Bokhari R, You E, Bakhaidar M, et al. Dural venous sinus thrombosis in patients presenting with blunt traumatic brain injuries and skull fractures: a systematic review and meta-analysis. World Neurosurg. 2020;142:495–505.e3. 13. Savoiardo M, Armenise S, Spagnolo P, et al. Dural sinus thrombosis in spontaneous intracranial hypotension: hypotheses on possible mechanisms. J Neurol. 2006;253:1197–202. 14. Girão MMV, Sousa RMP, Ribeiro MC, et al. Spontaneous intracranial hypotension and its complications. Arq Neuropsiquiatr. 2018;76:507–11. 15. Poon CS, Chang JK, Swarnkar A, et al. Radiologic diagnosis of cerebral venous thrombosis: pictorial review. AJR Am J Roentgenol. 2007;189(6 Suppl):S64–75. 1. Department of Radiology, Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil 2. Department of Radiology and Diagnostic Imaging, Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, RS, Brazil 3. Department of Diagnostic and Interventional Imaging, Hôpital du Valais, Sion, Valais, Switzerland a. https://orcid.org/0000-0002-2131-7360 b. https://orcid.org/0000-0003-4973-2889 c. https://orcid.org/0000-0001-9360-0547 d. https://orcid.org/0000-0002-7391-1193 e. https://orcid.org/0000-0002-0828-7806 f. https://orcid.org/0000-0003-2256-4379 Correspondence: Dra. Isabela Magalhães Oliveira Universidade Estadual de Campinas – Radiologia e Diagnóstico por Imagem Rua Vital Brasil, 251, Cidade Universitária Campinas, SP, Brazil, 13083-872 Email: isaamagalhaes17@gmail.com Received 22 January 2021 Accepted after revision 19 March 2021 Publication date: 15/06/2021 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554