Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 52 nº 1 - Jan. /Feb. of 2019
Vol. 52 nº 1 - Jan. /Feb. of 2019
|
NEWS IN RADIOLOGY
|
|
Percutaneous transhepatic cholangiobiopsy |
|
|
Autho(rs): Thiago Franchi Nunes1,a; Tiago Kojun Tibana2,b; Rômulo Florêncio Tristão Santos3,c; Bernardo Bacelar de Faria4,d; Edson Marchiori5,e |
|
|
Keywords: Bile duct neoplasms; Biliary tract; Biopsy/methods; Biopsy, needle/methods; Cholangiography. |
|
|
Abstract: strong>INTRODUCTION
Bile duct tumors are, for the most part, too small to have specific imaging characteristics or to allow percutaneous puncture that collects sufficient material for diagnosis(1,2). In addition, malignant neoplasms are not easily distinguished from benign lesions on the basis of the pathology findings. The results of fine-needle aspiration biopsy (FNAB) of the biliary system are inferior to those of FNAB of other sites(2). Therefore, other techniques for obtaining histological samples have been developed for use in the biliary tract(3-10). Percutaneous transhepatic biliary drainage (PTBD), in addition to being a well-established technique for the treatment of obstructive jaundice, provides adequate access for the sampling of obstructive lesions. In cases of biliary lesions, forceps biopsy during PTBD is a good diagnostic technique, with a reported accuracy of over 90% at some referral centers(3,4). Prior to any approaches to the biliary tract, it is paramount to have in-depth knowledge in the interpretation of imaging tests, especially magnetic resonance cholangiography(2,11,12). Possible biliary or vascular anatomical variants should be identified, the degree of biliary obstruction should be determined, and the extent of tumor invasion toward the hepatic hilum, according to the Bismuth classification(13). Patients who benefit most from forceps biopsy during PTBD are those with a serum bilirubin level > 10 mg/dL and an obstruction of the upper biliary tract, in the hepatic hilum (Klatskin-like lesion), that is classified as Bismuth type II, III, or IV, involves more than two thirds of the circumference of the bile duct, and has long (> 2 cm) stenoses. PROCEDURE Initially, puncture of the bile duct (right or left), based on previous imaging examinations, is performed. That is followed by cholangiography with a right anterior oblique projection, the objective of which is to visualize the point of obstruction, as well as the morphology and extent of the stenosis. If possible, fiberoptic endoscopy is used in order to characterize the target lesion more accurately. After passing through the stenosis, an angled introducer sheath is implanted in the region to be biopsied. If a 9F sheath is chosen, the corresponding guidewire should be 0.035 in. long, whereas it should be 0.014 in. long if an 8F sheath is chosen. With endoscopic forceps, at least five fragments of various sizes are collected from the perihilar region lesion (Figures 1 and 2). At the end of the procedure, it is recommended that a biliary drain (with its distal end in the duodenum) be inserted or that external drainage be performed, in case there are technical difficulties in bypassing the stenosis. 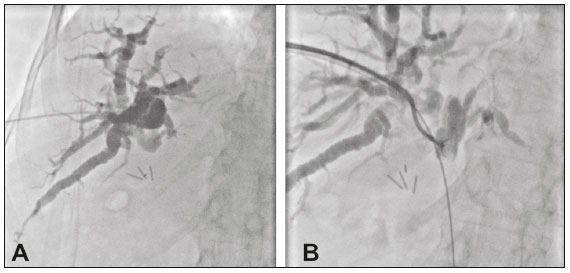 Figure 1. A: Puncture of the right bile duct in a patient with Bismuth type II stenosis. B: Passage of a 0.035-in guidewire, placement of a 9F sheath, and throughthe- needle forceps biopsy. The pathology report revealed cholangiocarcinoma. 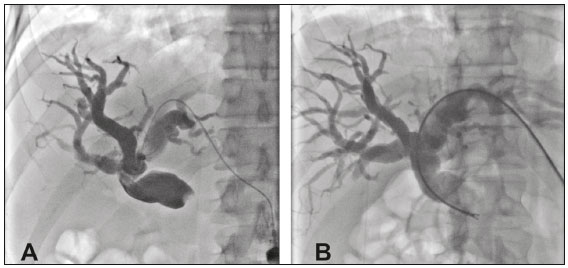 Figure 2. A: Puncture of the left bile duct in a patient with Bismuth type I stenosis. B: Placement of an 8F sheath and through-the-needle forceps biopsy with no guidewire. The pathology report revealed liver metastasis of colorectal carcinoma. Forceps biopsy during PTBD is a technically simple, minimally invasive procedure, with low complication rates and high diagnostic success rates in comparison with other known techniques(1,4). Its use has expanded the scope of research into biliary diseases. In clinical practice, it has proven to be an accurate, reliable method for the histopathological diagnosis of biliary tumors, as well as having a wide range of other applications. REFERENCES 1. Li Z, Li TF, Ren JZ, et al. Value of percutaneous transhepatic cholangiobiopsy for pathologic diagnosis of obstructive jaundice: analysis of 826 cases. Acta Radiol. 2017;58:3-9. 2. Smith I, Monkemuller K, Wilcox CM. Incidentally identified common bile duct dilatation: a systematic review of evaluation, causes, and outcome. J Clin Gastroenterol. 2015;49:810-5. 3. Tapping CR, Byass OR, Cast JE. Cytological sampling versus forceps biopsy during percutaneous transhepatic biliary drainage and analysis of factors predicting success. Cardiovasc Intervent Radiol. 2012;35:883-9. 4. Boos J, Yoo RJ, Steinkeler J, et al. Fluoroscopic percutaneous brush cytology, forceps biopsy and both in tandem for diagnosis of malignant biliary obstruction. Eur Radiol. 2018;28:522-9. 5. Schiavon LHO, Tyng CJ, Travesso DJ, et al. Computed tomography-guided percutaneous biopsy of abdominal lesions: indications, techniques, results, and complications. Radiol Bras. 2018;51:141-6. 6. Ribeiro KCP, Guimarães JPO, Aidar LB, et al. Hemobilia in a patient with arteriobiliary fistula after liver contusion. Radiol Bras. 2018;51:413-4. 7. Nunes TF. Percutaneous biopsy of abdominal lesions: what is currently the best diagnostic strategy? Radiol Bras. 2018;51(3):v-vi. 8. Zattar-Ramos LC, Bezerra RO, Siqueira LTB, et al. Hepatocyte-specific contrast agent-enhanced magnetic resonance cholangiography: perioperative evaluation of the biliary tree. Radiol Bras. 2017;50:389-94. 9. Zurstrassen CE, Bitencourt AGV, Guimaraes MD, et al. Percutaneous stent placement for the treatment of malignant biliary obstruction: nitinol versus elgiloy stents. Radiol Bras. 2017;50:97-102. 10. Cardarelli-Leite L, Fornazari VAV, Peres RR, et al. The value of percutaneous transhepatic treatment of biliary strictures following pediatric liver transplantation. Radiol Bras. 2017;50:308-13. 11. Tanaka H, Matsusaki S, Baba Y, et al. Usefulness of endoscopic transpapillary tissue sampling for malignant biliary strictures and predictive factors of diagnostic accuracy. Clin Endosc. 2018;51:174-80. 12. Li TF, Ren KW, Han XW, et al. Percutaneous transhepatic cholangiobiopsy to determine the pathological cause of anastomotic stenosis after cholangiojejunostomy for malignant obstructive jaundice. Clin Radiol. 2014;69:13-7. 13. Bismuth H, Nakache R, Diamond T. Management strategies in resection of hilar cholangiocarcinoma. Ann Surg. 1992;215:31-8. 1. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; a. https://orcid.org/0000-0003-0006-3725 2. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; b. https://orcid.org/0000-0001-5930-1383 3. Universidade Federal de Mato Grosso do Sul (UFMS), Campo Grande, MS, Brazil; c. https://orcid.org/0000-0002-8679-7369 4. Santa Casa de Campo Grande, Campo Grande, MS, Brazil; d. https://orcid.org/0000-0002-4258-2198 5. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil; e. https://orcid.org/0000-0001-8797-7380 Correspondence: Dr. Thiago Franchi Nunes Avenida Senador Filinto Müller, 355, Vila Ipiranga Campo Grande, MS, Brazil, 79080-190 Email: thiagofranchinunes@gmail.com Received November 3, 2017 Accepted after revision January 7, 2018 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554