RESUMO
OBJETIVO: Determinar fatores de risco radiológicos e clínicos para o desfecho de óbito em recém-nascidos com enterocolite necrosante.
MATERIAIS E MÉTODOS: Estudo de coorte retrospectivo de exames radiológicos e prontuários de 66 recém-nascidos com enterocolite necrosante confirmada pela presença de pneumatose intestinal (estágio IIA, segundo os critérios modificados de Bell). Foram estudados achados radiológicos e variáveis clínicas.
RESULTADOS: Catorze casos (21,2%) apresentaram pneumatose nos intestinos grosso e delgado, 7 (10,6%) apresentaram ar no sistema porta e 12 (18,2%) faleceram. As análises bivariadas indicaram que as variáveis significativas para o óbito foram: perfuração intestinal, pneumatose localizada nos intestinos grosso e delgado, ar no sistema porta, menor idade gestacional, longos períodos de ventilação mecânica até a identificação da pneumatose e longos períodos de ventilação mecânica até a data de alta/óbito. Na regressão multivariada, mantiveram-se como preditores do óbito: pneumatose localizada nos intestinos grosso e delgado (odds ratio [OR] = 12,4; intervalo de confiança de 95% [IC 95%] = 1,2-127,4; p = 0,035), perfuração (OR = 23,2; IC 95% = 2,2-246,7; p = 0,009) e ar no sistema porta (OR = 69,7; IC 95% = 4,3-não calculado; p = 0,003).
CONCLUSÃO: Pneumatose extensa, pneumoperitônio e ar no sistema porta compuseram o melhor conjunto de fatores associados ao óbito. Esses achados corroboram a importância da radiografia simples de abdome no diagnóstico e acompanhamento da enterocolite necrosante.
Palavras-chave:
Enterocolite necrosante/diagnóstico; Recém-nascido prematuro; Nascimento prematuro; Morte perinatal.
ABSTRACT
OBJECTIVE: The aim of this study was to identify radiological and clinical risk factors for death in newborns with necrotizing enterocolitis.
MATERIALS AND METHODS: This was a retrospective cohort study, based on radiological examinations and medical charts of 66 infants with necrotizing enterocolitis, as confirmed by a finding of intestinal pneumatosis (stage IIA, according to modified Bell’s staging criteria). Radiological and clinical variables were evaluated.
RESULTS: Of the 66 infants evaluated, 14 (21.2%) presented pneumatosis in the large and small bowel; 7 (10.6%) presented air in the portal system; and 12 (18.2%) died. Bivariate analysis revealed that the following variables were associated with death: bowel perforation; pneumatosis in the large and small bowel; air in the portal system; earlier gestational age; longer time on mechanical ventilation before the identification of pneumatosis; and longer time on mechanical ventilation before discharge or death. In the multivariate regression, the following variables remained as predictors of death: pneumatosis in the large and small intestines (odds ratio [OR] = 12.4; 95% confidence interval [95% CI] = 1.2-127.4; p = 0.035), perforation (OR = 23.2; 95% CI = 2.2-246.7; p = 0.009), and air in the portal system (OR = 69.7; 95% CI = 4.3-[not calculated]; p = 0.003).
CONCLUSION: The set of factors most strongly associated with death in infants with necrotizing enterocolitis comprised extensive pneumatosis, pneumoperitoneum, and air in the portal system. Our findings confirm the importance of radiological imaging in the diagnosis and monitoring of necrotizing enterocolitis.
Keywords:
Enterocolitis, necrotizing/diagnosis; Infant, premature; Premature birth; Perinatal death.
INTRODUÇÃO
A enterocolite necrosante (ECN) é uma doença inflamatória grave do trato gastrintestinal que acomete principalmente recém-nascidos (RNs), afetando 1% a 5% de todas as admissões de uma unidade de tratamento intensivo neonatal(1-3). A prematuridade é o principal fator de risco e mais de 90% dos RNs afetados têm idade gestacional inferior a 37 semanas(1,2). Essa doença representa uma das principais causas de intervenção cirúrgica entre RNs, sendo associada a taxas de mortalidade de até 50%(2).
A radiografia simples de abdome representa o método de imagem mais empregado para o diagnóstico e acompanhamento de RN com suspeita de ECN ou doença confirmada, em razão da sua facilidade de acesso e por não representar um procedimento invasivo(4). O sinal radiológico mais precoce, porém inespecífico, é a distensão difusa e assimétrica de alças intestinais. Os achados mais específicos são a presença de ar no sistema porta e a pneumatose intestinal, este último virtualmente patognomônico para ECN(4). Mais recentemente, o ultrassom de abdome vem sendo utilizado para o diagnóstico da ECN, já que sua sensibilidade é maior que a da radiografia simples em alguns aspectos, como na identificação de líquido livre na cavidade abdominal e na determinação da espessura e perfusão das alças intestinais. Entretanto, o ultrassom ainda tem valor limitado na avaliação prognóstica da doença e deve ser usado de forma complementar ao exame radiológico(4,5).
O valor prognóstico dos achados radiológicos para indicação de cirurgia tem sido reconhecido(6,7), entretanto, o valor prognóstico para o óbito foi pouco estudado e não é consistente nos diferentes estudos(8,9). Diante desse contexto, o presente estudo teve como objetivo avaliar variáveis clínicas e radiológicas que possam atuar como fatores de risco para a evolução a óbito em RNs com ECN, de forma a contribuir para os protocolos de atendimento desses pacientes.
MATERIAIS E MÉTODOS
Trata-se de um estudo de coorte retrospectivo. Os casos foram selecionados com base nos exames radiológicos dos RNs com diagnóstico clínico e radiológico (presença de pneumatose intestinal) de ECN IIA, segundo os critérios modificados de Bell(10), internados na unidade de tratamento intensivo neonatal de um hospital-escola entre 1991 e 2013. Foram excluídos os RNs provenientes de outros serviços e os com malformações congênitas. Preen cheram os critérios de inclusão 66 casos. O estudo foi aprovado pelo Comitê de Ética em Pesquisa da instituição onde o trabalho foi realizado.
Variáveis
As variáveis independentes radiológicas estudadas (Figuras 1 a 4) foram: a) distribuição da pneumatose intestinal, de padrão central (provável correspondência com o intestino delgado), periférico (provável correspondência com o intestino grosso), ou em ambos; b) extensão de acometimento da pneumatose intestinal, classificada como localizada (restrita a um quadrante abdominal acometido), moderada (dois ou três quadrantes acometidos), ou extensa (os quatro quadrantes acometidos); c) morfologia da pneumatose intestinal, caracterizada como radiolucência linear ou radiolucência bolhosa; d) presença de ar no sistema porta, definido como ramificações radiolucentes lineares que se estendem da região da veia porta principal para a periferia de ambos os lobos hepáticos(4); e) pneumoperitônio.
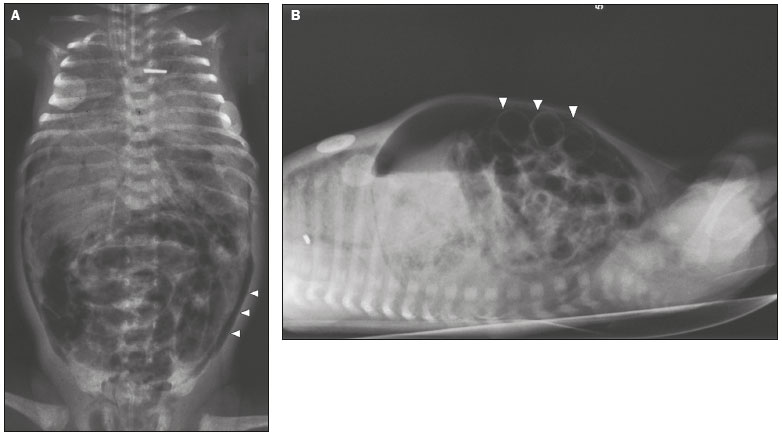
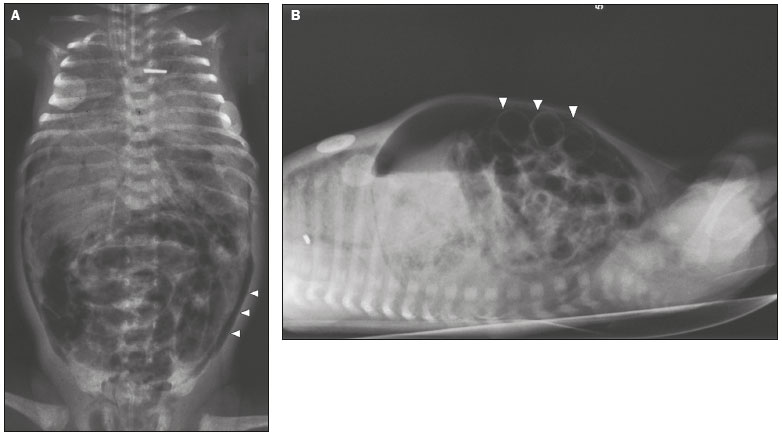 Figura 1
Figura 1. RN prematuro, com dois dias de vida, apresentando ECN.
A: Radiografia simples de abdome em decúbito dorsal com raios verticais demonstrando distensão de alças intestinais, pneumatose intestinal, ar no sistema porta e pneumoperitônio (cabeças de setas).
B: Radiografia simples realizada em decúbito dorsal com raios horizontais comprovando extenso pneumoperitônio, visível entre a parede abdominal anterior e as alças intestinais (cabeças de setas). Sinal de Rigler presente (visualização da parede das alças intestinais). O RN evoluiu para óbito.
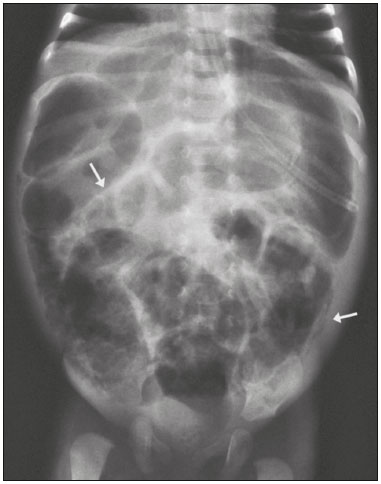
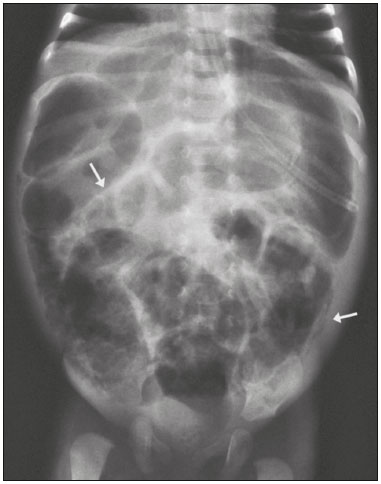 Figura 2
Figura 2. Radiografia de RN pré-termo, efetuada em decúbito dorsal com raios verticais, indicando distensão generalizada de alças intestinais e presença de pneumatose (setas) em segmentos dos intestinos grosso e delgado.
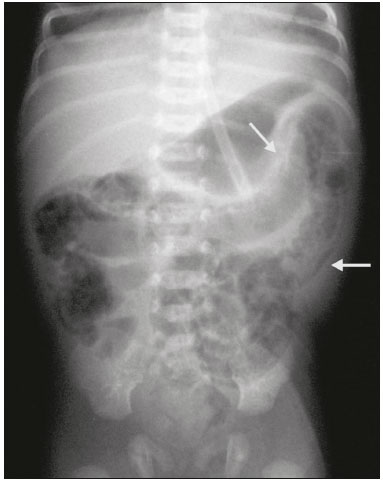
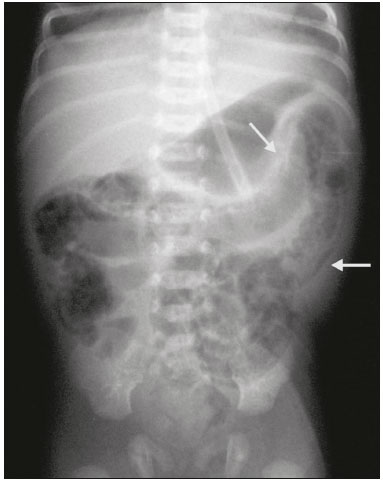 Figura 3
Figura 3. Radiografia simples de abdome em decúbito dorsal com raios verticais demonstrando pneumatose no intestino grosso (setas). O RN evoluiu com formação de pontos de estenose no cólon, necessitando de correção cirúrgica aos 38 dias de vida.
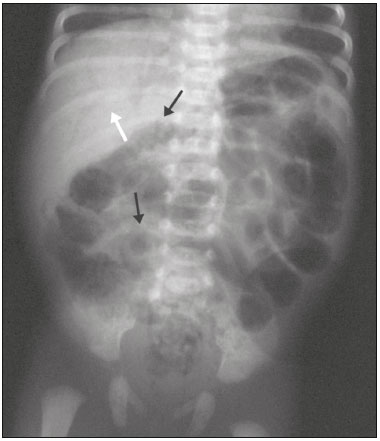
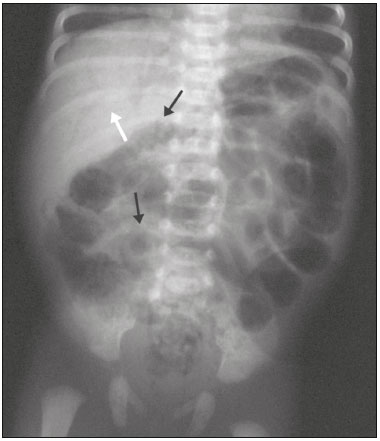 Figura 4
Figura 4. Radiografia simples de abdome em decúbito dorsal com raios verticais de RN pré-termo mostrando pneumatose intestinal (setas pretas) e ar no sistema porta (seta branca). O RN faleceu com 31 dias de vida.
As variáveis clínicas independentes estudadas foram: idade gestacional, estabelecida pelo tempo de amenorreia, pela ecografia ou pelo método clínico de Ballard
(11); peso ao nascer; gênero; tipo de parto; Apgar do 5º minuto; adequação do peso para a idade gestacional
(12); gemelaridade; e idade cronológica, quando identificada a pneumatose. Foram analisadas, ainda, as variáveis: a duração total da ventilação mecânica até o final da internação, mensurada em dias desde o momento da internação até a data de alta/óbito; e a duração da ventilação mecânica até a data de identificação da pneumatose. A variável dependente estudada foi o óbito.
Exames radiológicosAs radiografias de abdome foram realizadas em aparelho radiológico portátil VMX plus (GE Healthcare; Little Chalfont, Reino Unido), com o RN em decúbito dorsal, nas incidências anteroposterior (raios verticais) e perfil (raios horizontais).
Coleta de dadosA coleta de dados foi realizada pela pesquisadora responsável por meio da revisão de prontuários médicos. A avaliação radiológica foi realizada por um radiologista com especialização e experiência em radiologia neonatal. Todas as radiografias disponíveis de cada caso foram analisadas, sendo um mínimo de duas radiografias por caso. Foi sempre valorizado o pior achado e, diante de dois ou mais achados simultâneos, ambos foram incluídos na análise estatística de forma independente, não sendo avaliada a associação de dois achados radiográficos simultâneos como fator de pior prognóstico.
Análise estatísticaPara estabelecer a associação entre as variáveis categóricas, foram utilizados os testes qui-quadrado e exato de Fisher. Para comparar as variáveis numéricas, foi utilizado o teste de Mann-Whitney. Para analisar os fatores relacionados ao óbito, foi utilizada a análise de regressão logística nos modelos univariado e multivariado, com critério
step wise de seleção de variáveis.
O nível de significância adotado para os testes estatísticos foi 5% e o programa utilizado para análise estatística foi The SAS System for Windows (Statistical Analysis System), na versão 9.4 (SAS Institute Inc., 2002-2012, Cary, NC, EUA).
RESULTADOSDos 66 casos analisados, 56 (84,8%) foram RNs pré- termo, 57 (86,4%) tiveram baixo peso ao nascer e 36 (54,5%) tiveram muito baixo peso ao nascer. Em 51 casos (78,5%) a pneumatose estava restrita ao intestino grosso (padrão periférico) e em 14 (21,5%) casos estava presente nos intestinos grosso e delgado. Durante a evolução, 7 RNs (10,6%) apresentaram ar no sistema porta, 15 RNs (22,7%) apresentaram perfuração intestinal e 12 RNs (18,2%) faleceram. Dentre os casos que faleceram, 7 (58,3%) tiveram perfuração, 1 (8,3%) era RN a termo e 9 (75%) tiveram muito baixo peso ao nascer.
A análise bivariada das variáveis categóricas entre os grupos de RNs com e sem óbito revelou uma significativa associação da ocorrência de óbito com a distribuição simultânea da pneumatose nos intestinos grosso e delgado (padrões central e periférico), com pneumoperitônio e com a presença de ar no sistema porta (Tabela 1). Os RNs que faleceram tinham menor idade gestacional e maior duração da ventilação mecânica até a data de identificação da pneumatose e durante toda a internação.
A análise de regressão logística univariada identificou as seguintes variáveis como fatores de risco para o óbito: tempo de ventilação mecânica até a identificação da pneumatose (
odds ratio [OR] = 1,14; intervalo de confiança de 95% [IC 95%] = 1,04-1,26), perfuração de alças intestinais (OR = 8,05; IC 95% = 2,04-31,72), localização simultânea da pneumatose nos intestinos delgado e grosso (OR = 6,90; IC 95% = 1,69-28,10) e presença de ar no sistema porta (OR = 21,67; IC 95% = 3,43-137,08).
Os resultados da análise multivariada estão descritos na Tabela 2. Segundo essa análise, os pacientes com maior risco de óbito foram os que exibiram ar no sistema porta (risco 69,7 vezes maior), perfuração de alças intestinais (23,2 vezes maior) e pneumatose com distribuição central e periférica simultaneamente (12,4 vezes maior).
DISCUSSÃONo presente trabalho identificamos que os sinais radiológicos ar no sistema porta, pneumoperitônio e pneumatose de distribuição central e periférica compuseram o melhor modelo para identificar o risco de mortalidade associado a ECN em RNs com média de idade gestacional de 32,7 semanas.
Na análise bivariada, as variáveis clínicas idade gestacional, duração da ventilação mecânica até o aparecimento da pneumatose intestinal e até alta/óbito diferiram entre os grupos com óbito e sem óbito. Na regressão univariada, a duração da ventilação até o diagnóstico foi o único fator clínico indicativo de maior risco, provavelmente por ser um marcador de maior gravidade clínica. A análise multivariada, que é um poderoso instrumento de supressão de efeitos de confundimento, descartou essa variável clínica como fator significativo para o óbito. Esse achado difere de outros autores
(2,13), que apontam maior mortalidade em RNs com menor idade gestacional, menor peso ao nascer e em uso de ventilação mecânica no dia do diagnóstico da ECN. Tal diferença de resultados pode estar associada a variações nos tamanhos amostrais e nos desenhos dos estudos. O estudo de Clark et al.
(13), por exemplo, analisou apenas variáveis clínicas, enquanto o presente trabalho incluiu variáveis radiológicas na análise de regressão.
Existem controvérsias na literatura quanto ao papel do ar no sistema porta no prognóstico da ECN. Frequentemente, os autores identificam que o achado de ar no sistema porta e de pneumoperitônio são indicadores de necessidade cirúrgica
(6,7,14). A intervenção cirúrgica, por sua vez, é relacionada a maior mortalidade
(2). Alguns autores não mostram associação do ar no sistema porta com maiores taxas de óbito
(9), enquanto outros associam esse sinal a um estágio mais grave da doença
(8,15). Os resultados do presente estudo estiveram de acordo com a segunda observação, demonstrando que o ar no sistema porta foi a variável que esteve associada ao maior risco de óbito.
A perfuração de alças é uma variável bem estudada e estabelecida na literatura como importante fator de risco para óbito
(16,17), representando um sinalizador de gravidade e de necessidade imediata de intervenção cirúrgica
(6,17). A relevância dessa variável no desfecho do óbito foi corroborada pelo presente estudo.
Nosso trabalho mostrou significativa associação do óbito com a distribuição simultânea da pneumatose nos intestinos grosso e delgado (padrão central e periférico). Em última análise, a localização mais ampla da pneumatose é uma medida de maior extensão do envolvimento da ECN, correspondendo a maior extensão do processo inflamatório secundário à doença e repercutindo em piora do prognóstico. Cabe aqui ressaltar que a variável extensão da pneumatose, avaliada pelo critério de quadrantes abdominais descrito na literatura
(8), e aparentemente de mais fácil avaliação, não se mostrou significativa em nenhuma das análises estatísticas. A identificação do intestino grosso é geralmente mais difícil em RN, pela pobreza de haustrações
(18). Utilizamos o critério do sítio das alças intestinais para reconhecer os dois segmentos intestinais e esse critério foi mais sensível que o critério de número de quadrantes envolvidos. Isso pode ser consequência da transitoriedade da pneumatose, que pode desaparecer rapidamente, e de sua dimensão, que pode variar muito ao longo da evolução do paciente
(4).
A associação dos achados radiológicos com indicação cirúrgica e com óbito foi frequentemente obtida em estudos mais antigos, que tomaram como base análises estatísticas menos sofisticadas, ou seja, simples análises de frequências. Encontramos poucos estudos nos quais as variáveis radiológicas foram estudadas pelo modelo de regressão. Esse aspecto parece ser um diferencial do nosso estudo. Por outro lado, o estudo de Sharma et al.
(9), utilizando o mesmo método de análise estatística, encontrou que o ar no sistema porta não aumentou o óbito, resultado nitidamente diferente do obtido por nós. Todavia, Sharma et al.
(9) usaram uma amostra na qual predominaram RNs de muito baixo peso e que tiveram ocorrência significativamente menor de ar no sistema porta e de pneumatose, em relação aos RNs de maior peso do mesmo estudo. Essa observação também já foi descrita em outra publicação
(15). Dessa forma, o ar no sistema porta, a pneumatose e o pneumoperitônio foram menos comuns entre RNs de menor peso e, portanto, têm menor sensibilidade para o diagnóstico e seguimento da ECN nessa população.
Segundo o modelo obtido pela análise multivariada, os RNs mais suscetíveis ao óbito foram os que apresentaram ar no sistema porta, perfuração de alças intestinais e pneumatose intestinal com distribuição central e periférica simultaneamente. Esses achados justificam o óbito, pois permitem inferir que grandes extensões de intestino foram acometidas, determinando um desfecho desfavorável. Essa associação de óbito e pneumatose extensa (isolada ou com ar no sistema porta), cursando com grandes extensões de necrose intestinal, já foi anteriormente sugerida
(8).
É necessário apontar que o nosso estudo apresenta limitações. Foram avaliados 66 casos em 12 anos, pois a incidência de ECN no serviço é baixa (3,1%) quando comparada à descrita por outros autores
(1-3). Esse tamanho amostral limitado repercutiu sobre a amplitude dos intervalos de confiança no modelo gerado pela regressão multivariada. Dessa forma, a amplitude desse intervalo limita a precisão do risco, mas não tira a importância da variável como determinante do óbito, já que na análise univariada os IC 95% foram estreitos, confirmando a importância de cada fator isoladamente no aumento na mortalidade.
CONCLUSÃOAinda que longos períodos de ventilação mecânica até o aparecimento da pneumatose intestinal tenham representado um fator de risco clínico para o óbito, a pneumatose extensa, o pneumoperitônio e a presença de ar no sistema porta compuseram o melhor conjunto de fatores associados a esse desfecho. Tal associação corrobora a importância da radiologia convencional no diagnóstico e acompanhamento da ECN em RNs.
REFERÊNCIAS1. Srinivasan PS, Brandler MD, D''Souza A. Necrotizing enterocolitis. Clin Perinatol. 2008;35:251-72.
2. Lin PW, Stoll B. Necrotising enterocolitis. Lancet. 2006;368:1271-83.
3. Neu J, Walker WA. Necrotizing enterocolitis. N Engl J Med. 2011; 364:255-64.
4. Epelman M, Daneman A, Navarro OM, et al. Necrotizing enterocolitis: review of state-of-the-art imaging findings with pathologic correlation. Radiographics. 2007;27:285-305.
5. Bohnhorst B. Usefulness of abdominal ultrasound in diagnosing necrotising enterocolitis. Arch Dis Child Fetal Neonatal Ed. 2013;98:F445-50.
6. Coursey CA, Hollingsworth CL, Wriston C, et al. Radiographic predictors of disease severity in neonates and infants with necrotizing enterocolitis. AJR Am J Roentgenol. 2009;193:1408-13.
7. He Y, Zhong Y, Yu J, et al. Ultrasonography and radiography findings predicted the need for surgery in patients with necrotising enterocolitis without pneumoperitoneum. Acta Paediatr. 2016;105:e151-5.
8. Kosloske AM, Musemeche CA, Ball WS Jr, et al. Necrotizing enterocolitis: value of radiographic findings to predict outcome. AJR Am J Roentgenol. 1988;151:771-4.
9. Sharma R, Tepas JJ 3rd, Hudak ML, et al. Portal venous gas and surgical outcome of neonatal necrotizing enterocolitis. J Pediatr Surg. 2005;40:371-6.
10. Walsh MC, Kliegman RM. Necrotizing enterocolitis: treatment based on staging criteria. Pediatr Clin North Am. 1986;33:179-201.
11. Ballard JL, Khoury JC, Wedig K, et al. New Ballard Score, expanded to include extremely premature infants. J Pediatr. 1991;119:417-23.
12. Alexander GR, Himes JH, Kaufman RB, et al. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163-8.
13. Clark RH, Gordon P, Walker WM, et al. Characteristics of patients who die of necrotizing enterocolitis. J Perinatol. 2012;32:199-204.
14. Kosloske AM. Indications for operation in necrotizing enterocolitis revisited. J Pediatr Surg. 1994;29:663-6.
15. Tam AL, Camberos A, Applebaum H. Surgical decision making in necrotizing enterocolitis and focal intestinal perforation: predictive value of radiologic findings. J Pediatr Surg. 2002;37:1688-91.
16. Swischuk LE. Alimentary tract. In: Swischuk LE, editor. Imaging of the newborn, infant, and young child. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. p. 341-589.
17. Kastenberg ZJ, Sylvester KG. The surgical management of necrotizing enterocolitis. Clin Perinatol. 2013;40:135-48.
18. Morrison SC, Jacobson JM. The radiology of necrotizing enterocolitis. Clin Perinatol. 1994;21:347-63.
1. Médica Residente da Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brasil
2. Doutora, Professora do Departamento de Pediatria da Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brasil
3. Doutora, Professora do Departamento de Radiologia da Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brasil
Endereço para correspondência:Dra. Isabela Gusson Galdino dos Santos
Rua Patrocínio do Sapucaí, 820, ap. 2, Jardim Flamboyant
Campinas, SP, Brasil, 13091-105
E-mail:
isagusson@gmail.comRecebido para publicação em 10/3/2017
Aceito, após revisão, em 13/6/2017

 |
|