Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 2 - Mar. / Apr. of 2015
Vol. 48 nº 2 - Mar. / Apr. of 2015
|
ORIGINAL ARTICLE
|
|
An ABC for decision making |
|
|
Autho(rs): Luiz Henrique Costa Garcia1; Bruna Cortez Ferreira2 |
|
|
Keywords: Intensive care; Neuroimaging; Emergency medicine; Computed tomography; Traumatic brain injury; Intracranial hemorrhage. |
|
|
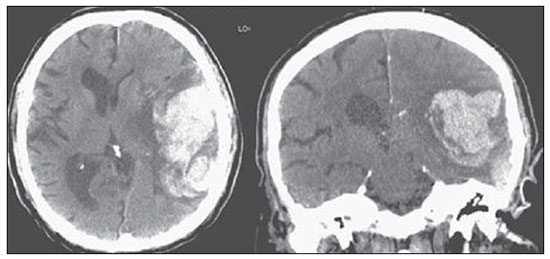
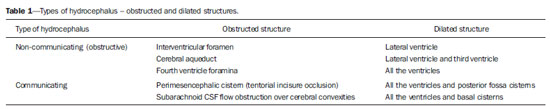
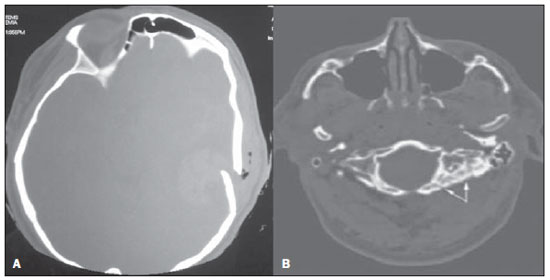
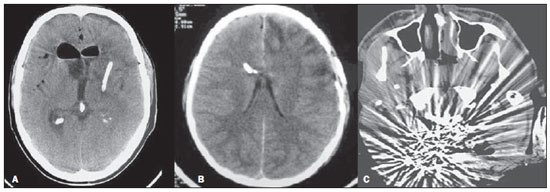
Abstract: INTRODUCTION
Cranial computed tomography (CT) is an extremely useful and common imaging method, particularly in the intensive care environment and at emergency departments in most hospitals both in Brazil and worldwide. Differently from magnetic resonance imaging, CT is widely available and many times is the initial imaging modality of choice both for diagnosis and treatment guidance(1). There are several and varied indications for this examination, namely, Glasgow coma scale alterations, acute confusional state, sudden onset of intense headache, severe cranioencephalic trauma, persistent somnolence, epilepsy disease state, postictal state with decreased level of consciousness or focal deficit, cerebral hypoxic lesion (post-cardiac arrest syndrome)(2). In emergency settings, cranial CT is the cerebral investigation method of choice for its noninvasiveness, wide availability, easy and rapid utilization, besides the relatively low cost(3). Cranial CT can, for example, distinguish between hemorrhagic and ischemic stroke at an early phase, which is a determining factor in the prognosis and treatment. After the hemorrhagic event, one can quickly visualize the abnormality at CT due to the high density of the blood as compared with the cerebral tissue. However, CT presents a low sensitivity to demonstrate ischemic non-hemorrhagic stroke at the first hours following the acute event(4-7). For a long time it has been known that the agility in the diagnosis allows for an immediate treatment with better outcomes. Additionally, many times, physicians on duty, particularly those on night shifts, are neither neurology/neurosurgery specialists nor radiologists, so that they lack the required expertise to interpret CT images in an emergency setting. And besides, most hospitals do not have an established night shift plan in radiology, so there is a dilemma, as despite the constant increase in the use of this technological apparatus, who is going to interpret the images? In the greatest majority of hospitals, as a routine, the requesting physicians himself/herself analyses the images, makes decisions and indicates the approach to be adopted. The medical training programs have increasingly included the training in radiology. Similarly, the interpretation of electrocardiograms that, initially, should be done by cardiologists, is a routine for generalist physicians who must know how to interpret them. Therefore, it is not impracticable that the same occurs with cranial CT images, at least as regards a baseline evaluation(8). The present study proposes a systematization of cranial CT evaluation, indicating the main items to be observed, in order to guide those physicians working at emergency departments in hospitals as well those working at intensive care units. For such a purpose, the authors propose a systematic evaluation based on the ABCDEFG sequence according to the model of the Advanced Trauma Life Support (ATLS) guidelines to evaluate chest radiography. A descriptive study was developed after literature review at the following databases: Access Medicine and Access Emergency Medicine (McGraw-Hill Education); Bristish Medical Journal Evidence Center; UptoDate; Bireme; PubMed; Lilacs; SciELO; ProQuest; Micromedex (Thomson Reuters); Embase. Once the literature review was completed, the authors identified the main pathologies with tomographic repercussions and proposed the present system to evaluate cranial CT images. DISCUSSION The main clinically and neurosurgically significant conditions are the following: intraparenchymal, subdural, subarachnoid and extradural hemorrhages; diffuse axonal lesions; stroke (either ischemic or hemorrhagic); cerebral edema; tumors; hydrocephalus and other causes of ventricular and cisterns dilation; trauma. Based on such information, the authors propose a systematics adapted from the ABC included in the Advanced Cardiovascular Life Support (ACLS) guidelines. The English language was utilized with the purpose of universalizing the use of this systematics. A: ATTENUATION - evaluation of the difference in the attenuation of the white and gray matter, as well as of the different densities of the cerebral parenchyma, searching for signs of cerebral edema, stroke and tumors. B: BLOOD - evaluation of the presence of bleeding in the parenchyma, cisterns and ventricles, as well as of the reaction to the presence of such blood as midline shift. The nature of the bleeding is determined, whether intraparenchymal, extradural or subdural. C: CAVITIES - assessment of cranial cavities: ventricles and cisterns. D: DILATION - evaluation of ventricular and cisterns dilation, as postoperative complication or disease. E: EXTERIOR - assessment of the bone plate and subcutaneous tissue. F: FISHER SCALE - Fisher grading, in the case of subarachnoid hemorrhage; G: GHOSTS, DRAINS AND ARTIFACTS - drains, catheters and artifacts are observed. At cranial CT, the following findings should be observed: A: ATTENUATION - CT captures cross-sectional images by means of x-rays, and reconstructs them via computer. Black and white images are formed with variations of grayscale shades according to the structure density as well as to the x-ray energy level. Such a phenomenon is called x-ray attenuation. The degree of imaging beam attenuation is quantified and expressed in Hounsfield units (HU). The attenuation values range from -1000 HU, corresponding to air, to 3000 HU, corresponding to bone, while the water density corresponds to zero HU(9). At cranial CT, each tissue attenuation occurs by the difference in absorption between the white and gray matters, according to their myelinic and, consequently, fatty contents. Fat and air present low attenuation values and can be easily identified. The cerebrospinal fluid (CSF) has an attenuation value similar to the one of water, and appears black. The different pathological processes may become apparent as a result of the presence of edema in the lesion or in adjacent structures. The edema appears less dense than the adjacent structures(8). In this first step, one should search for attenuation differences between tissues that might suggest ischemic event, edema or masses. Stroke is a common event and is divided into two types with diametrically opposite causes, namely: hemorrhagic stroke, resulting from bleeding within the cranial cavity; and ischemic stroke - corresponding to about 80% of all strokes -, resulting from lack of blood supply (and, consequently, lack of oxygen) to the brain tissue. Hemorrhagic stroke, that will be later approached on B in the present study, may be subdivided into parenchymal hemorrhagic stroke (blood in the parenchyma) and stroke with subarachnoid hemorrhage (blood in the CSF)(8). The infracted brain is initially pale and, as the hours and days pass, the grey matter becomes swollen, with blood vessels dilatation and small petechias. When an embolus occluding a vessel undergoes lysis or migrates, there is a blood inflow into the infarcted area, possibly causing blood extravasation and consequential hemorrhagic transformation. In most of times, ischemic strokes occur due to decreased cerebral blood flow generating oxygen and nutrients deficit in this tissue. Another genesis is explained by occlusion of drainage veins, resulting in cerebral edema, possibly leading to either cerebral ischemia or hemorrhage. As regards causes, three main events might lead to ischemic stroke: arterial thrombosis resulting from arterial wall diseases by atherosclerosis, dissection or fibromuscular dysplasia; embolism, where particles coming from elsewhere in the body migrate to any region of the brain; but as this is not a process restricted to a defined area, local therapy can only solve the problem temporarily; systemic hypoperfusion, where there is a general decrease in blood supply, consequently depriving the brain tissue of blood. Yet there is the nosological entity called transient ischemic attack, where the neurological symptoms last less than 24 hours(10-12). The literature reports rates approaching 60% of non detection of strokes at the first 12 hours, so at such moment CT scan is indicated to evaluate a possible bleeding. A study utilizing only CT evaluation at the first 6 hours following symptoms onset reports a diagnostic accuracy of 61%(4). It is important to mention that, in cases of middle cerebral artery (MCA) stroke, CT demonstrates abnormalities in up 75% of cases already at the first three hours. A hyperdense signal can be seen, corresponding to the presence of an intraluminal thrombus in the region of the MCA (sylvian fissure). The first signs of ischemic stroke are the following: hypoattenuation of the MCA region, effacement of the lentiform nucleus and cortical sulci, focal hypoattenuation of the parenchyma, obscuration of the sylvian fissure, MCA hyperdensity - observed in 30% to 40% of patients, due to thrombus in the arterial lumen (Figure 1) -, and loss of gray-white differentiation in the basal ganglia (Figure 2).  Figure 1. Arrow shows MCA hyperdensity. 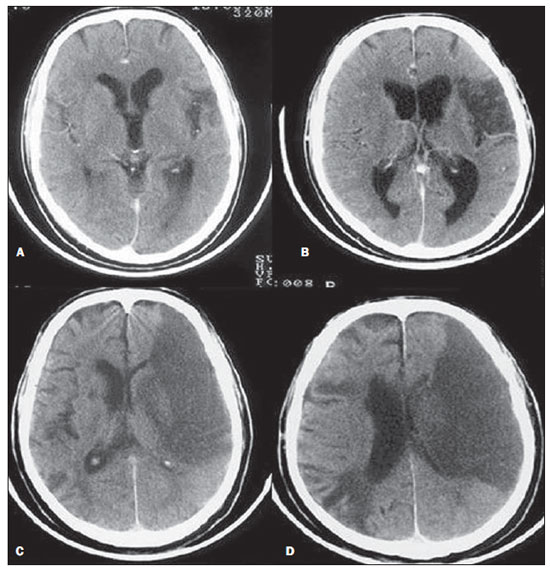 Figure 2. CT showing MCA ischemic stroke. A,B: Partial infarction with involvement restricted to the left hemisphere. C,D: Complete infarction at left, with mass effect compressing the lateral ventricle; minor hypodensity at left of the right hemisphere. Between 12 and 24 hours, there is an alteration in the normal white-gray differentiation resulting from edema. After 24 hours, up to the seventh day, an area of hypodensity is seen in a vascular distribution (in 70% of cases), due to cytotoxic edema. Also, a mass effect may occur, with total or partial compression of ventricles and cisterns. Hemorrhagic transformation may occur and in 70% of cases can be seen between the second and fourth days. With the mass effect decrease, if any, ex vacuo dilatation of the ventricles may be observed. Later there might be a loss of parenchymal mass, with associated sulci and ventricular enlargement consequential to encephalomalacia(13,14). In some cases, tomographic signs may be already visualized within 6 six hours after the ischemic stroke symptoms onset (Figure 3). 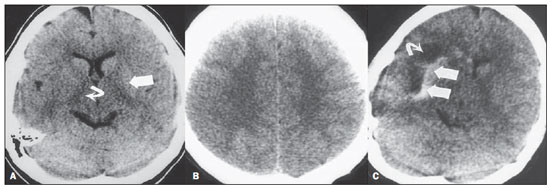 Figure 3. A: CT 6 hours after symptoms onset. The curved arrow indicates medial demarcation of the posterior portion of the right internal capsule. Observe that the lateral margin of the internal capsule is ill defined by the decreased attenuation of the lentiform nucleus. The straight arrow indicates the normal left internal capsule and lentiform nucleus. B: Decreased white-gray differentiation in the right cerebral hemisphere, corresponding to the MCA distribution. C: Three days after the event, with a larger area of attenuation (straight arrows) corresponding to hemorrhage in a region of infarction. Non hemorrhagic areas of infarction demonstrate hypoattenuation (curved arrow). B: BLOOD - Relevant cerebral bleedings are intraparenchymal, subarachnoid, subdural, and extradural hemorrhages, in addition to diffuse axonal lesions. Intracranial hemorrhage accounts for 15% of all strokes with greater mortality as compared with the other stroke subtypes (up to 50% at the first 48 hours following onset)(15). It affects mainly hypertensive men users of thrombolytic and anticoagulant drugs, cocaine and amphetamines, besides smokers and those with diabetes(16). The location of the bleeding predicts the underlying clinical condition, for example, putaminal hemorrhages may present with contralateral deviation and/or hemiparesis/hemiplegia, aphasia, neglect or agnosia; thalamic hemorrhages may present with aphasia (dominant side), neglect (non dominant side), contralateral sensory or motor deficit; brainstem injuries may present with coma, tetraparesis, nystagmus, hyperthermia and abnormal respiratory patterns. Cerebellar hemorrhages may present with ataxia and nystagmus. Signs of increased intracranial pressure/hydrocephalus: complete effacement of the fourth ventricle or cerebral aqueduct(17)(Figure 4). Subarachnoid hemorrhage (SAH), with an annual incidence of 1/10,000 in the United States of America, is not by far the main reason for hospital admission, but presents a high morbimortality, and for this reason an early recognition and aggressive treatment can improve the outcomes(18). It occurs most commonly in women around the age of 50. Up to 12% of patients die before reaching a hospital, and 50% die within six months. Additionally, 33% to 66% of the survivals have a significant neurological deficit. SAH is bleeding into the subarachnoid space, whose cause in 75% of cases is aneurysm rupture; and in 25% is caused by arteriovenous malformations, cerebral arterial dissection, coagulopathies, moyamoya syndrome, mycotic aneurysm, pituitary apoplexy, vasculopathy, brain tumor and utilization of sympathomimetic drugs. Considering the devastating potential of an erroneous and delayed diagnosis, measures should quickly be taken for the management of subarachnoid hemorrhage. Despite all the technology available, 5% to 12% of patients presenting with suggestive symptoms are not diagnosed with SAH at their first visit to the hospital after the event(19). Non-contrast enhanced cranial CT should be the first study to be requested, with estimated sensitivity of 98% at the first 12 hours after symptoms onset (Figure 5). After 24 hours, its sensitivity decreases to 93%, followed by a rapid decrease after complete or almost complete resorption at the first ten days(20). 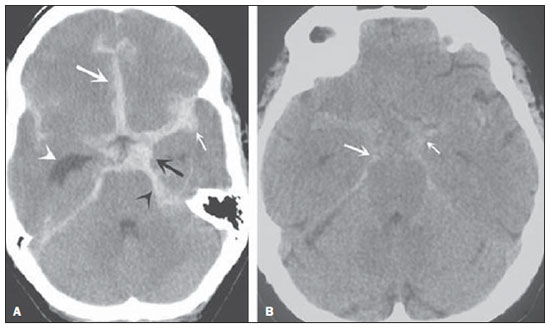 Figure 5. A: Hyperdensity on the suprasellar cistern (black arrow), interhemispheric fissure (larger white arrow), cerebellopontine cistern (black arrowhead) and sylvian fissure (thinner white arrow). The smaller white arrow indicates secondary hydrocephalus in the lateral ventricle. B: Moderate hyperdensity on the suprasellar spaces (thinner arrow) and perimesencephalic cisterns (larger arrow). Subdural hemorrhage (SDH) is the bleeding between the dura mater and the arachnoid membranes, affecting principally men aged between 31 and 47, as a result from blunt trauma due car accidents, falls and assaults. There is also a group of individuals with chronic SDH: elderly people, people with history of chronic alcohol abuse, and those with previous cerebral trauma/injury. SDH is caused by rupture of veins that drain from the brain surface to the dural sinuses. The rupture of such vessels causes bleeding into the space between the dura mater and the arachnoid membranes, contained by the increased intracranial pressure or by the direct compression by the clot itself. About 20% to 30% of SDHs occur due to arterial rupture. A decrease in the CSF pressure (hypotension caused either by spontaneous CSF leak or after CSF puncture) can also lead to SDH. With the decreased CSF pressure, the brain fluctuation is impaired, causing traction over the support and fixation structures, and consequential traction and rupture of vessels. Differently from epidural (or extradural) hematoma, SDH can cross the suture lines, although limited by subdural processes, generating a crescent-shaped extra-axial lesion (Figure 6)(21,22). This nosological entity is peculiar as it is present since the very moment of the injury in approximately 50% of cases. However, about 12% to 38% of patients present a "lucid interval" following the acute trauma (a period where the patient does not present with any clinical sign or symptom, after which he/she may present progressive neurological decline up to coma). Eventually, due either to the increased intracranial pressure or to the mass effect, cerebral hypoperfusion and consequential infarction might occur, particularly in those cases of SDH because of the greater vulnerability to the posterior cerebral arteries compression along the tentorial edge. A study developed in 1988 identified diagnostic accuracy of 91% in SDH > 5 mm. An even higher diagnostic accuracy is estimated nowadays with the developments in the CT techniques(23,24). 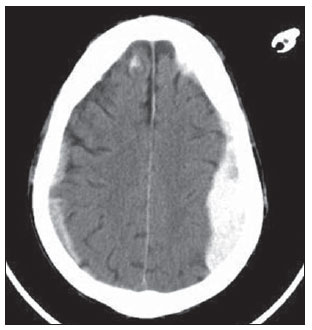 Figure 6. SDH at left. Still in this topic, it is important to mention extradural or epidural hematoma (EDH), which results from the accumulation of blood in the space between the skull and the dura mater. The main injury mechanism is contuse trauma either in the temporal or temporoparietal region, with skull fracture associated with middle meningeal artery rupture. Occasionally, a trauma in the parieto-occipital region or in the posterior fossa leads to injury to the venous sinuses with consequential EDH. Classically, there is a massive craniocerebral trauma with consciousness loss or sensory alterations, followed by a lucid period and subsequent sudden neurological death. Biconvex shape hemorrhage is seen at CT, with high density located in the periphery of the cranial cavity. Epidural hemorrhage crosses the dural reflection, but not the suture lines (differently from SDH), and a mass effect may be observed with consequential signs of herniation and edema(2) (Figure 7). The high-pressure arterial bleeding of EDH may cause herniation within hours after the injury, thus early recognition and evacuation are vital(25). 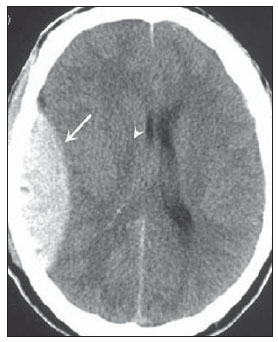 Figure 7. Acute EDH demonstrated by the biconvex lens shape (arrow). The arrowhead indicates the decreased lumen of the right lateral ventricle, associated with midline shift, suggesting subfalcine herniation. Diffuse axonal injury (DAI) is the rupture of axonal fibers of the white matter and brainstem caused by traumatic shearing forces, as a result from sudden deceleration. Classically, it occurs after a contuse trauma (car accident), and may also occur in children (shaken baby syndrome). In cases of DAI one may observe rapid development of edema, with devastating, frequently irreversible neurological deficits. CT may be either normal or, classically, demonstrate punctate hemorrhagic lesions along the grey-white junction of the cerebral cortex and within the deep cerebral structures(26) (Figure 8). 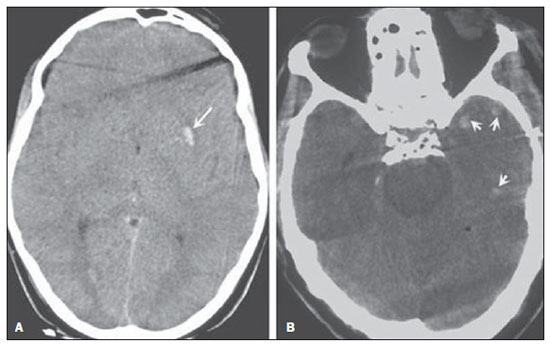 Figure 8. A: DAI with focus of hyperdensity on the grey-white interface (arrow). B: Contusions with hyperdense foci (arrows) compatible with blood in the parenchyma. C: CAVITIES - Ventricles, cisterns, sulci and fissures patency is evaluated. Generally, such structures are filled with CSF. The ventricular system is system of communication between cavities which are lined by ependyma and filled with CSF. There are two lateral ventricles, the third ventricle (between the halves of the diencephalon), the cerebral aqueduct, and the fourth ventricle within the brainstem. The lateral ventricles are the larger ones, each including two central portions (body and atrium) and three extensions (horns). The two interventricular foramina (or foramina of Monro) are channels located between the fornix column and the anterior extremity of the thalamus. The two lateral ventricles communicate with the third ventricle by means of these foramina. The third ventricle is a narrow vertical fissure located between the two halves dos the diencephalon. Its lateral walls are formed principally by the medial surfaces of the two thalami. The inferior lateral wall and the floor of the ventricle are formed by the hypothalamus; the anterior commissure and the terminal lamina of hypothalamus form the rostral limit. The cerebral aqueduct is a narrow, curved channel connecting the posterior portion of the third ventricle to the fourth ventricle. The fourth ventricle is a pyramid-shaped cavity ventrally delimited by the pons and by the spinal cord, and its floor is also known as rhomboid fossa. The lateral recess is a projection of the fourth ventricle which extends into the inferior cerebellar peduncle of the brainstem. The fourth ventricle extends under the obex into the central canal of the medulla. The point at which the fourth ventricle passes up into the cerebellum is called apex or fastigium. The position of the cerebellum, immediately above the fourth ventricle, has significant clinical implications. Expansile cerebellar lesions (tumors, for example) or cerebellar edema following stroke may compress the fourth ventricle, generating acute obstructive hydrocephalus. The lateral aperture (foramen of Luschka) is the opening of the lateral recess into the subarachnoid space near the floccullus of the cerebellum. A tuft of choroid plexus is usually present in the opening and partially obstructs the CSF flow from the fourth ventricle to the subarachnoid space. The medial aperture (foramen of Magendie) is an opening in the caudal portion of the roof of the ventricle. Most of the CSF outflow from the fourth ventricle occurs trough this foramen. The cisterns are subarachnoid cavities fulfilled with CSF, which communicate to each other and with the subarachnoid space. Such cisterns can be better visualized at magnetic resonance imaging, but it is possible to detect them at CT, where they appear normally open. The cisterna magna is the common space of CSF between the medulla and the cerebellum hemispheres. The pontine cistern surrounds the ventral aspect of the pons and contains the basilar artery and some veins. Under the brain there is a wide space between the two temporal lobes. Such space is divided into chiasmatic cistern, above the chiasma; the suprasellar cistern above the sella turcica; and the interpeduncular cistern between the cerebral peduncles The space between the frontal, parietal and temporal lobes is called cistern of lateral fissure (cistern of Sylvius)(27) (Figure 9). 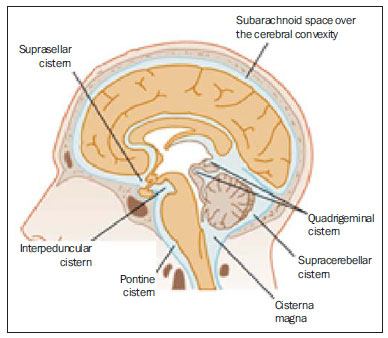 Figure 9. Cisterns. (Adapted from Waxman(27)). In practice, the ventricles are evaluated as regards absence, presence or dilatation (completing the following evaluation D: DILATION). Also, the presence or absence of the cisterns is evaluated, and their absence result either from encephalic herniation or severe cerebral edema(28). The sulci and fissures separate the frontal, parietal, occipital and temporal lobes and the insula. Their patency may also be compromised in the presence of other diseases(29). D: DILATION - At this point, the presence of dilation of the ventricles is evaluated, as it suggests hydrocephalus. Previously to hydrocephalus as a disease, there are two clinical entities which appear as hydrocephalus at CT, but without increase in the intracranial pressure. The first one is ex vacuo hydrocephalus, and the second one, normal pressure hydrocephalus (NPH). It may be difficult to differentiate between hydrocephalus and ventriculomegaly due to cerebral atrophy (ex vacuo hydrocephalus). The following characteristics are suggestive of hydrocephalus instead of ventriculomegaly secondary to cerebral atrophy: widening of third ventricle recess, dilation of temporal horns of the lateral ventricles, tissues interstitial edema, cortical sulcal effacement(30) (Figure 10). 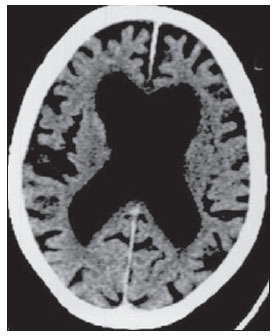 Figure 10. Hydrocephalus secondary to atrophy. On the other hand, NPH is characterized by the clinical features of hydrocephalus (abnormal gait either with or without urinary incontinence or cognitive dysfunction), but without a significant increase in the CSF pressure. Nonetheless, it responds to a decrease in the CSF pressure and/or to a shunting procedure. NPH is a confuse and misleading denomination as the term "hydrocephalus" is generally utilized to describe a high CSF pressure in the brain, and in NPH the pressure in the ventricular system is not significantly abnormal(31). In NPH, the image may be normal or show evidences of ventricular widening or periventricular leukomalacia (i.e., injury to white matter surrounding the cerebral ventricles). Disproportionate central atrophy may be observed, resulting in larger ventricles with relative preservation of the cortical sulci in the atrophic process. The presence of an obstructive lesion rules out the diagnosis(32). The disease hydrocephalus may be divided into communicating and non communicating hydrocephalus. Non communicating (obstructive) hydrocephalus, that is more prevalent, occurs because the CSF accumulates in the ventricles and does not reach the subarachnoid space due to the obstruction of one or both interventricular foramina, the cerebral aqueduct (the most common site of obstruction), or the outflow foramina of the forth ventricle (medial and lateral apertures). In communicating hydrocephalus, the obstruction occurs in the subarachnoid space and may result from prior hemorrhage or meningitis, generating thickening of the arachnoid membrane with obstruction of the drainage ducts (Table 1). Hydrocephalus may occur after neurosurgeries, with incidence of 8% in cases of tumors resection. It results from bleeding into the subarachnoid or into the ventricles due to inappropriate hemostasis or extension of surgery to the ventricles. Also, it may occur as a function of edema in the surgical site, with consequential secondary obstruction of the CSF drainage sites (particularly in cases where the surgery is performed around the aqueduct or foramen of Monro). It may also result from postoperative CSF infection (i.e., ventriculitis or meningitis) Also, it may occur between two and four postoperative weeks as a consequence of progressive arachnoiditis caused by aseptic bacterial meningitis or even subarachnoid hemorrhage resulting from aneurysm. For this reason, some centers perform routine postoperative CT as a protocol, since many patients are intubated and under sedation as they return from surgery(27). E: EXTERNAL - Bone plate and, consequently, skull bone fractures, skull base fractures included, are evaluated. Contuse or penetrating head trauma may cause injury to the scalp or even to the bone. The skull fracture may be either an open or blunt (either with or without break in continuity of the skin, respectively). Fracture lines may be simple (linear), multiple with lines radiating from a point (stellate), or multiple, creating bone fragments (comminuted). Skull base fractures are common in patients with significant trauma kinematics (Figure 11). Such fractures are generally seen at non-contrast-enhanced CT. Eventually, subgaleal hematoma may also be found(33,34). F: FISHER SCALE - In cases of subarachnoid hemorrhage, the Fisher scale is a resort based on the amount and distribution of the hemorrhage that is useful to predict the risk for vasospasm. There is a more recent version of this scale - the modified Fisher scale -, which provides a qualitative value for the presence of blood bilaterally in the ventricles and cisterns, predicting a higher risk for vasospasm(35,36) (Table 2). 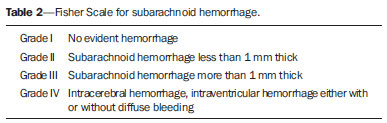 G: GHOSTS, DRAINS AND ARTIFACTS - Some diseases require drainage and, consequently, CT demonstrates the presence of drains. Also, invasive monitoring by means of catheters is necessary, just like in the case of intracranial pressure catheters (Figure 12). Artifact is the visual impression of the image of an object that actually does not exist in the scanned tissue. It is important to recognize artifacts in order to avoid confusion with diseases. Artifacts may occur due to failure of the digitizing apparatus, patient motion, and presence of foreign bodies. Motion artifacts tend to result in ray patterns. In cases of metal artifacts, whose attenuation coefficient is much higher than that for any internal structure, the result is loss of definition of the adjacent structures(8). For example, a patient with cranial trauma in the 1940' required the placement of a metal plate on the left frontal region, and CT demonstrates a significant artifact caused by the presence of such a metal plate(37). CONCLUSION The systematization of CT images evaluation reduces the chances of equivocal diagnoses as well of missing lesions which should be found otherwise. Additionally, considering that 100% of hospitals lack specialists to discuss the imaging findings in emergency settings on a 24-hours-per-day basis, the presently proposed system may facilitate the work of physicians, particularly in the environment of intensive care units and emergency departments, with lower chances of medical errors. Acknowledgements To Doctors Uri Adrian Prync Flato, Daniela Pino Vinho, Fabiano Hirata and Roberto Marcó, and all the assistants at Irmandade da Santa Casa de Misericórdia de São Paulo. REFERENCES 1. Grossman RI. Head trauma. In: Yousem DM, editor. Neuroradiology: the requisites. 2nd ed. Philadelphia: Mosby; 2003. p. 243. 2. Krishnam MS, Curtis J. Emergency radiology. Cambridge: Cambridge University Press; 2010. 3. John C, Elsner E, Müller A, et al. Computed tomographic diagnosis of acute cerebral ischemia. Radiologe. 1997;37:853-8. 4. Marks MP, Holmgren EB, Fox AJ, et al. Evaluation of early computed tomography findings in acute ischemic stroke. Stroke. 1999;30:389-92. 5. Pressman BD, Tourje EJ, Thompson JR. An early CT sign of ischemic infarction: increased density in a cerebral artery. AJR Am J Roentgenol. 1987;149:583-6. 6. von Kummer R, Allen KL, Holle R, et al. Acute stroke: usefulness of early CT findings before thrombolytic therapy. Radiology. 1997;205:327-33. 7. Scarabino T, Salvolini U, Jinkins JR. Emergency neuroradiology. Berlin: Springer; 2006. 8. Holmes EJ, Forest-Hay AC, Misra RR. Interpretation of emergency head CT: a practical handbook. Cambridge: Cambridge University Press; 2008. 9. Roper W, Abbuhl S. Computed tomography. In: Tintinalli JE, Stapczynski JS, Ma OJ, et al., editors. Tintinalli's emergency medicine: a comprehensive study guide. 7th ed. New York: McGraw-Hill; 2011. e299.2. 10. Caplan LR. Intracranial branch atheromatous disease: a neglected, understudied, and underused concept. Neurology. 1989;39:1246-50. 11. Caplan LR. Basic pathology, anatomy, and pathophysiology of stroke. In: Caplan LR, editor. Caplan's stroke: a clinical approach. 4th ed. Philadelphia: Saunders Elsevier; 2009. p. 22. 12. Caplan LR, Manning WJ. Brain embolism. New York: Informa Healthcare; 2006. 13. Beauchamp NJ Jr, Barker PB, Wang PY, et al. Imaging of acute cerebral ischemia. Radiology. 1999;212:307-24. 14. Tomandl BF, Klotz E, Handschu R, et al. Comprehensive imaging of ischemic stroke with multisection CT. Radiographics. 2003;23:565-92. 15. Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Stroke. 2007;38:2001-23. 16. Ariesen MJ, Claus SP, Rinkel GJ, et al. Risk factors for intracerebral hemorrhage in the general population: a systematic review. Stroke. 2003;34:2060-5. 17. Barrocas AM, Longenecker BA. Intracranial hemorrhage. In: Farcy DA, Chiu WC, Flaxman A, et al., editors. Critical care emergency medicine. New York: McGraw-Hill; 2012. p. 285-92. 18. Wojak JC, Flamm ES. Intracranial hemorrhage and cocaine use. Stroke. 1987;18:712-5. 19. Schievink WI. Intracranial aneurysms. N Engl J Med. 1997;336:28-40. 20. Al-Shahi R, White PM, Davenport RJ, et al. Subarachnoid hemorrhage. BMJ. 2006;333:235-40. 21. Besenski N. Traumatic injuries: imaging of head injuries. Eur Radiol. 2002;12:1237-52. 22. Koç RK, Akdemir H, Oktem IS, et al. Acute subdural hematoma: outcome and outcome prediction. Neurosurg Rev. 1997;20:239-44. 23. Victor M, Ropper A. Craniocerebral trauma. In: Victor M, Ropper A, editors. Adams and Victor's principles of neurology. 7th ed. New York: McGraw-Hill; 2001. p. 925-53. 24. Gentry LR, Godersky JC, Thompson B, et al. Prospective comparative study of intermediate-field MR and CT in the evaluation of closed head trauma. AJR Am J Roentgenol. 1988;150:673-82. 25. Wright DW, Merck LH. Head trauma in adults and children. In: Tintinalli JE, Stapczynski JS, Ma OJ, et al., editors. Tintinalli's emergency medicine: a comprehensive study guide. 7th ed. New York: McGraw-Hill; 2011. [acessado em 25 de junho de 2013]. Disponível em: http://accessmedicine.mhmedical.com/content.aspx?bookid=348&Sectionid=40381742. 26. King WJ, MacKay M, Sirnick A; Canadian Shaken Baby Study Group. Shaken baby syndrome in Canada: clinical characteristics and outcomes of hospital cases. CMAJ. 2003;168:155-9. 27. Waxman SG. Ventricles and coverings of the brain. In: Waxman SG, editor. Clinical neuroanatomy. 26th ed. New York: McGraw-Hill; 2010. p. 149-62. 28. Sinagra A, Pérez M, Acuña M. Tercer ventrículo. Endoneuroanatomía de las estructuras adyacentes. Revista Argentina de Anatomía Online. 2010;1:16-20. 29. Waxman SG. Cerebral hemispheres/telencephalon. In: Waxman SG, editor. Clinical neuroanatomy. 26th ed. New York: McGraw-Hill; 2010. p. 131-47. 30. Schwartz DT. Hydrocephalus - use of CT before LP. In: Schwartz DT, editor. Emergency radiology: case studies. New York: McGraw-Hill; 2008. p. 487-96. 31. INPH Guidelines Study Group. Guidelines for the diagnosis and management of idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57(Suppl 3):S1-52. 32. Ropper AH, Samuels MA. Disturbances of cerebrospinal fluid and its circulation, including hydrocephalus, pseudotumor cerebri, and low-pressure syndromes. In: Ropper AH, Samuels MA, editors. Adams and Victor's principles of neurology. 9th ed. New York: McGraw-Hill; 2009. p. 591-5. 33. Smith ML, Bauman JA, Grady MS. Neurosurgery. In: Brunicardi FC, Andersen DK, Billiar TR, et al., editors. Schwartz's principles of surgery. 9th ed. New York: McGraw-Hill; 2010. p. 1515-56. 34. Koizumi H, Suzuki S, Utsuki S, et al. A case of non-traumatic subgaleal hematoma effectively treated with endovascular surgery. Interv Neuroradiol. 2010;16:317-21. 35. Vivancos J, Gilo F, Frutos R, et al. Guía de actuación clínica en la hemorragia subaracnoidea. Sistemática diagnóstica y tratamiento. Neurología. 2014;29:353-70. 36. Novelline RA, Rhea JT, Rao PM, et al. Helical CT in emergency radiology. Radiology. 1999;213:321-39. 37. Hackett MT, Shih WJ, Kiefer VH. Brain SPECT artifacts in patients having metallic cranioplasty. J Nucl Med Technol. 2001;29:189-92. 1. General Surgeon, Intensive Medicine Specialist, Associação de Medicina Intensiva Brasileira (AMIB), and Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brazil 2. MD, Resident of Medical Practice at Hospital de Base de São José do Rio Preto, São José do Rio Preto, SP, Brazil Mailing Address: Dr. Luiz Henrique Costa Garcia Rua Frederico Straube, 600, Casa 13, Vila Oliveira Mogi das Cruzes, SP, Brazil, 08790-310 E-mail: luiz_mogi@yahoo.com.br Received July 1, 2013. Accepted after revision February 7, 2014. Study developed at Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554