Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 2 - Mar. / Apr. of 2015
Vol. 48 nº 2 - Mar. / Apr. of 2015
|
LETTER TO THE EDITOR
|
|
Enhancing survival with early surgical resection of endobronchial metastasis in a follow-up of ovarian carcinoma |
|
|
Autho(rs): Rafael Marques Franco1; Marcos Duarte Guimaraes2; Bruno Lima Moreira2; Almir Galvão Vieira Bitencourt2; Bruno Hochhegger 3; Edson Marchiori4 |
|
|
Dear Editor,
A 45 year-old female patient presented with a previous history of abdominal pain whose onset had occurred one year earlier. Pelvic ultrasonography demonstrated a suspiciously malignant left adnexal complex cyst, confirmed by pelvic magnetic resonance imaging. After surgical resection, the histological diagnosis was ovarian endometrioid adenocarcinoma. As lymph nodes were negative and there was no clinical or radiological evidence of distant metastasis, the disease stage was IA and the surgery was considered curative. Chest multidetector computed tomography (CT) performed at six-month follow-up demonstrated an unusual finding of a small endobronchial lesion of 6.7 mm in the left lower lobe causing significant bronchial narrowing (Figure 1). The patient had neither complaints nor symptoms and follow-up positron emission tomography/CT did not reveal any abnormal fluoro-2-deoxy-glucose uptake, including by the endobronchial lesion. Transbronchial biopsy of the lesion confirmed a mucin-producing adenocarcinoma positive for CA-125, compatible with metastasis from the ovarian adenocarcinoma. The patient underwent left lower lobectomy followed by chemotherapy. Five years after treatment completion follow-up exams showed no evidence of disease activity. 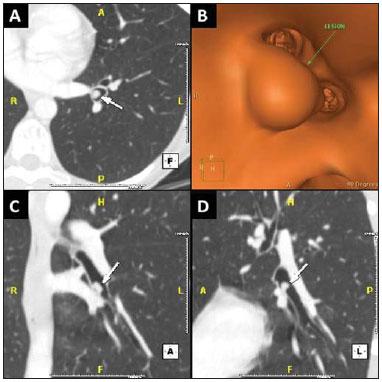 Figure 1. A: CT image shows an endobronchial nodule (arrows) in the lateral basal bronchus of the left lower lobe. B: This nodule measures 6.7 mm. C: CT coronal reconstruction demonstrating > 50% decrease of the endobronchial lumen (arrow). D: Virtual bronchoscopy confirms the endobronchial narrowing. Endobronchial metastases from ovarian carcinoma are rare, and few cases are described in the literature. Clinical and radiological findings are quite similar to those of endobronchial primary lung cancer, so a histopathological diagnosis is critical in such cases(1). Endobronchial metastasis is defined as primary involvement of the bronchial epithelium, originating from extra-pulmonary malignant tumors(2). Salud et al. showed that breast, colorectal and renal carcinomas were the most common primary sites of endobronchial metastasis(3). None of these studies demonstrated ovarian tumor as the primary site as occurred in the present case. Endobronchial metastases may be asymptomatic without any other signs of dissemination from the primary tumor, as demonstrated in the present case(4). Symptoms may be associated with airway obstruction (dyspnea, wheezing), mucosal irritation and ulceration (cough, hemoptysis), or direct invasion and involvement of adjacent structures (recurrent laryngeal nerve palsy, dysphagia). Currently, multidetector CT is the best imaging modality for the diagnosis and characterization of endobronchial metastases. Multiplanar two-dimensional and three-dimensional image reconstruction techniques, including virtual bronchoscopy, can be easily generated to complement conventional axial CT imaging. In addition, virtual bronchoscopy provides a noninvasive method to evaluate airway lesions and plays an essential role as a complement to conventional bronchoscopy, facilitating planning and guidance of bronchoscopic interventions(5). CT is relatively accurate in the evaluation of bronchial abnormalities, and in patients with endobronchial metastases may be used as a complement to bronchoscopy to evaluate lesion extent(6). Finally, endobronchial metastases are rare and have clinical and radiological findings similar to those of primary endobronchial tumors. Although uncommon, oncologists and radiologists should be alert to the occurrence of endobronchial metastases in early follow-up of patients previously treated for ovarian carcinoma, in order to avoid delay in the diagnosis and to allow for proper therapeutic planning. REFERENCES 1. Merrill CR, Hopkirk JA. Late endobronchial metastasis from ovarian tumour. Br J Dis Chest. 1982;76:253-4. 2. Ikezoe J, Johkoh T, Takeuchi N, et al. CT findings of endobronchial metastasis. Acta Radiol. 1991;32:455-60. 3. Salud A, Porcel JM, Rovirosa A, et al. Endobronchial metastatic disease: analysis of 32 cases. J Surg Oncol. 1996;62:249-52. 4. Sørensen JB. Endobronchial metastases from extrapulmonary solid tumors. Acta Oncol. 2004;43:73-9. 5. Lee KS, Boiselle PM. Update on multidetector computed tomography imaging of the airways. J Thorac Imaging. 2010;25:112-24. 6. Ko JH, Jung GS, Kim SM, et al. Endobronchial metastasis: CT findings and its usefulness in bronchoscopic correlation. J Korean Radiol Soc. 2000;43:179-84. 1. Hospital Heliópolis, São Paulo, SP, Brazil 2. A.C.Camargo Cancer Center, São Paulo, SP, Brazil 3. Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA), Porto Alegre, RS, Brazil 4. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil Mailing Address: Dr. Rafael Marques Franco Rua Cônego Xavier, 276, Cidade Nova Heliópolis São Paulo, SP, Brazil, 04231-030 E-mail: rafaelmarquesfranco@gmail.com |
|
GN1© Copyright 2024 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554