Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 48 nº 1 - Jan. /Feb. of 2015
Vol. 48 nº 1 - Jan. /Feb. of 2015
|
LETTER TO THE EDITOR
|
|
Giant pilomatrixoma: conventional and diffusion-weighted magnetic resonance imaging findings |
|
|
Autho(rs): Bruno Niemeyer de Freitas Ribeiro1; Edson Marchiori2 |
|
|
Dear Editor,
Over the last two years, a 32-year-old man presented growth of a little painful firm nodule located in the high parietal region. Due to the cosmetic deformity, the patient sought medical assistance and underwent laboratory tests whose results were normal, and magnetic resonance imaging (MRI) (Figure 1) that demonstrated the presence of a heterogeneous lesion with predominance of iso/hyposignal on T1-weighted, low signal intensity on T2-weighted, foci of signal drop on magnetic susceptibility sequences and absence of diffusion restriction. After gadolinium injection, exuberant contrast enhancement was observed. Histopathological analysis revealed the presence of basaloid cells associated with phantom cells, with areas of foreign-body-type granulomatous reaction compatible with pilomatrixoma. Surgical resection was performed and no recurrence has been observed up to the present moment. 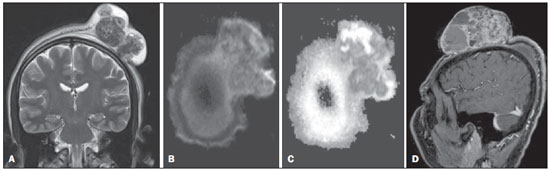 Figure 1. A: Coronal, T2-weighted sequence showing a tumor in the left parietal region with predominance of hyposignal, intermingled with areas of cystic/necrotic degeneration. B: Axial functional MRI, diffusion-weighted sequence does not demonstrate areas of hypersignal. C: Axial image, apparent diffusion coefficient mapping corroborating the absence of areas of diffusion restriction. D: Contrast-enhanced sagittal T1-weighted sequence showing exuberant and heterogeneous contrast enhancement. Most of times, tumor-like processes in the skull are associated with bone or central nervous system lesions, as reported by recent studies developed by Brazilian authors(1-7). However, skin tumors are rarely similar to each other. Pilomatrixoma is a rare benign skin tumor originating from hair follicle matrix, most frequently located in the head or neck(8-10). It is the most common solid skin tumor in patients under the age of 20(9). Giant pilomatrixomas (> 5 cm) are not frequently found and malignant transformation rarely occurs. Clinically, it manifests as a slow-growing, painless or little painful lesion, sometimes in association with bluish coloration of the skin(11). Histopathological analysis gives the definitive diagnosis, and the treatment is surgical resection with margins of 1 to 2 cm to avoid recurrence. At MRI, most lesions are well delimited, measuring up to 3 cm, with homogeneous iso-signal on T1-weighted and low signal intensity on T2-weighted sequences. However, reports about striated lesions with hypersignal from the center to the periphery are found in the literature(8,10,12). Calcifications are commonly found and may not present expressive contrast enhancement or even enhance only in the already described areas of hypersignal on T2-weighted sequences(8,10,12). Besides the uncommon lesion size (10.2 cm), heterogeneous signal was observed on T1- and T2-weighted images, with predominance of iso/hyposignal on T2-weighted images, intermingled with areas of cystic/necrotic degeneration and foci of signal drop on magnetic susceptibility sequences. After gadolinium injection, exuberant contrast enhancement of the solid portions of the tumor was observed. Recent studies highlight the utilization of diffusion-weighted sequences in the evaluation of head and neck lesions, demonstrating that apparent diffusion coefficient values < 1.22 × 10-3 mm2/s are suggestive of malignancy(13). In the present case, such a value was 1.35 × 10-3 mm2/s, corroborating the previously described findings. Other advanced MRI sequences might add further data, particularly in the prediction of benignity and malignancy(14,15). Finally, the diagnosis of pilomatrixoma should be considered in patients under the age of 20 presenting with skin tumors, particularly those located in the head and neck, and typical imaging findings should not be expected in cases of giant pilomatrixomas. REFERENCES 1. Werner Jr H. Evaluation of the central nervous system of fetuses and neonates. Radiol Bras. 2012;45(6):v-vi. 2. Sanches P, Yamashita S, Freitas CCM, et al. Chordoid glioma of the third ventricle: a new case report. Radiol Bras. 2012;45:288-90. 3. Coeli GNM, Tiengo RR, Silva AC, et al. Nodular calcified neurocysticercosis with signs of reactivation. Radiol Bras. 2012;45:291-3. 4. Reis F, Schwingel R, Nascimento FBP. Central nervous system lymphoma: iconographic essay. Radiol Bras. 2013;46:110-6. 5. Brandão LA. Primary and secondary lymphoma of the central nervous system. Conventional and functional magnetic resonance imaging findings. Radiol Bras. 2013;46(2):ix-x. 6. Curioni OA, Souza RP, Amar A, et al. Value of PET/CT in the approach to head and neck cancer. Radiol Bras. 2012;45:315-8. 7. Matushita JP, Matushita JS, Simões LAM, et al. Giant cell tumor of the frontal sinus: case report. Radiol Bras. 2013;46:255-8. 8. Hsieh TJ, Wang CK, Tsai KB, et al. Pilomatricoma: magnetic resonance imaging and pathological evaluation. J Comput Assist Tomogr. 2008;32:320-3. 9. Beaman FD, Kransdorf MF, Andrews TR, et al. Superficial soft-tissue masses: analysis, diagnosis, and differential considerations. Radiographics. 2007;27:509-23. 10. Laffan EE, Ngan BY, Navarro OM. Pediatric soft-tissue tumors and pseudotumors: MR imaging features with pathologic correlation: part 2. Tumors of fibroblastic/myofibroblastic, so-called fibrohistiocytic, muscular, lymphomatous, neurogenic, hair matrix, and uncertain origin. Radiographics. 2009;29:e36. 11. Whittemore KR, Cohen M. Imaging and review of a large pre-auricular pilomatrixoma in a child. World J Radiol. 2012;4:228-30. 12. De Beuckeleer LH, De Schepper AM, Neetens I. Magnetic resonance imaging of pilomatricoma. Eur Radiol. 1996;6:72-5. 13. Gonçalves FG, Ovalle JP, Grieb DFJ, et al. Diffusion in the head and neck: an assessment beyond the anatomy. Radiol Bras. 2011;44:308-14. 14. Wang CK, Li CW, Hsieh TJ, et al. Characterization of bone and soft-tissue tumors with in vivo 1H MR spectroscopy: initial results. Radiology. 2004;232:599-605. 15. Costa FM, Vianna EM, Domingues RC, et al. Espectroscopia de prótons e perfusão por ressonância magnética na avaliação dos tumores do sistema musculoesquelético. Radiol Bras. 2009;42:215-23. 1. Instituto Estadual do Cérebro Paulo Niemeyer, Rio de Janeiro, RJ, Brasil 2. Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brasil Mailing Address: Dr. Bruno Niemeyer de Freitas Ribeiro Instituto Estadual do Cérebro Paulo Niemeyer - Serviço de Radiologia Rua do Rezende, 156, Centro Rio de Janeiro, RJ, Brazil, 20231-092 E-mail: bruno.niemeyer@hotmail.com |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554