Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 6 - Nov. / Dec. of 2014
Vol. 47 nº 6 - Nov. / Dec. of 2014
|
ORIGINAL ARTICLE
|
|
Intensity modulated radiotherapy (IMRT) for patients of the Brazilian unified health system (SUS): an analysis of 508 treatments two years after the technique implementation |
|
|
Autho(rs): Harley Francisco de Oliveira1; Felipe Amstalden Trevisan2; Viviane Marques Bighetti3; Flávio da Silva Guimarães4; Leonardo Lira Amaral5; Gustavo Lázaro Barbi6; Leandro Federiche Borges7; Fernanda Maris Peria8 |
|
|
Keywords: Radiotherapy; Unified Health System; SUS; IMRT. |
|
|
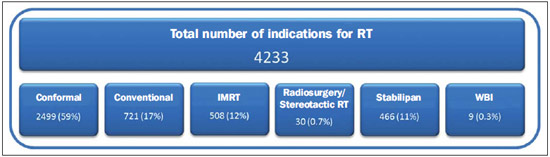
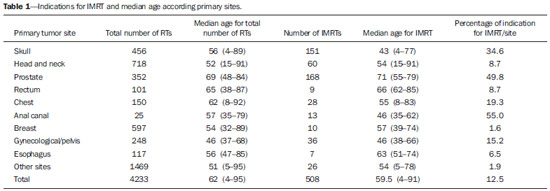
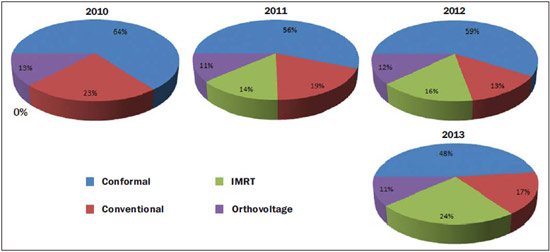
Abstract: INTRODUCTION
In Brazil, health care delivery is a responsibility of the federal administration by means of the Unified (Health System Sistema Único de Saúde - SUS), therefore public health assistance is a State duty at all levels including the tertiary levels involved in the delivery of high-complexity and high-cost health services(1,2). Many times, the universal, comprehensive and costless nature of health services diffused as a cardinal role of SUS is observed in the health assistance structure of the system. In the state of São Paulo, two of the main university hospitals (Universidade de São Paulo - USP, in São Paulo and Ribeirão Preto), besides Instituto do Câncer do Estado de São Paulo Octavio Frias de Oliveira (Icesp) can offer high-technology radiotherapy (RT) such as fractionated stereotactic RT, radiosurgery, intensity-modulated RT (IMRT) and imaging-guided RT (IGRT) to the population covered by SUS. Despite this promising information, such institutions have a limited "installed capacity" and are not able to meet the huge demand for such treatment, so the main challenge is the waiting time for RT, with necessity of a careful selection of patients who will benefit from advanced RT techniques. Despite not being included in the SUS procedures list, IMRT is highlighted as one of the most relevant advances in RT since the introduction of the clinical linear particle accelerator, since it improves the delivery of high radiation doses to a target volume (treatment region) while reducing the toxicity in the healthy adjacent tissues. On the other hand, this technique requires increased time and dedication from the team of physicians, medical physicians, dosimetrists and RT technologists during the planning, quality control activities and optimization of the 3D principles of the modern RT. Such a technique can be utilized for treatment of different types of cancer affecting head and neck, prostate, breast, brain and stomach, either as a healing or palliative measure, demonstrating a reduction of both acute and chronic toxicity, besides improving the local management of tumors. The authors intend to contribute to the creation of clinical IMRT protocols for SUS's patients, besides spreading their acquired experience in the period they had access to the technique. The patients' selection is decisive in the quality of the assistance provided by a public RT service, as this technique demands longer working hours both from the apparatuses and the personnel involved, worsening the problems associated with access to the services and waiting time. The present study was aimed at analyzing the main clinical characteristics of the first 508 SUS's patients submitted to IMRT during the first years following the technique implementation. MATERIALS AND METHODS The first consecutive 508 cases of IMRT treatment in the period from May/2011 to September/2013 at Service of Radiotherapy of Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP) were reviewed. The proposed initial treatment was completed by 98% of the patients. RT was scheduled in the context of integrated oncological care, many times in association with chemotherapy, surgery and/or hormone therapy, but it was not evaluated in the present study. No patient was excluded from the analysis. IMRT was indicated in cases where 3D conformal RT (3DRT) failed to allow for dose restriction in risk organs or significant clinical benefit such as protection of optic tracts or brain stem in brain treatments, and rectum or bladder in prostate treatments. Other clinical indications for IMRT were established in the institution's clinical protocol for the different primary cancer sites, considering the patient's general condition, the histopathological diagnosis and the tumor staging. Previously to the procedure, all the patients signed a term of free and informed consent with information about indications and possible adverse effects of the technique. The inverse IMRT plannings were made with the CMS/XiO version 4.51.02 planning system (Elekta Inc.; Stockholm, Sweden) which received the images by means of a CT DICOM protocol (Philips Brilliance CT Big Bore; Philips Medical Systems, UK). As necessary, particularly in cases of brain tumors, images co-registration with MRI was performed on the same planning week, on a 3T apparatus (Intera 3T; Philips Medical Systems, Best, The Netherlands). Quality controls were individually analyzed by an ion chamber array system (Matrixx, MultiCube, and Omnipro I'MRT QA Software) (IBA Dosimetry; Bartlett, USA) and gamma function was applied between the planes generated by CMS/XiO and Omnipro. Treatment acceptance occurred as the gamma function was < 3%. The treatments were performed in a multileaf (1 cm-thick) linear particle accelerator (Oncor; Siemens, Germany). Step-and-shoot static IMRT was the technique employed, allowing for custom tailored radiation doses delivered to multiple small volumes only as the linear accelerator gantry is fixed on determined positions. RESULTS During the study period, 4233 new cases were admitted for external beam radiation therapy (RT) and 12.5% of them were treated by the IMRT technique. Other treatment modalities were also utilized in this period, with prevalence of 3DRT in 59% of the patients, as shown on Figure 1. Amongst the IMRT plannings, 33% were indicated for prostate tumors; 30% for brain tumors; and 12% for head and neck tumors, despite the fact that such cases represented respectively 8%, 11% and 17% of the total number of RT treatments (Figure 2). Also, the indications for other sites occurred in 25% of IMRTs. 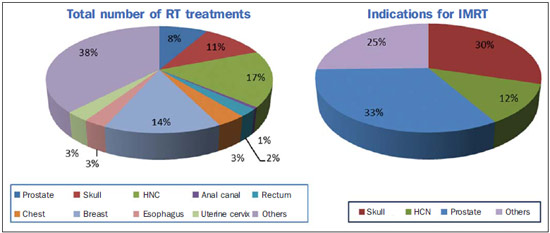 Figure 2. Distribution of primary tumor sites per total number of RT and IMRT treatments in the period between 2010 and 2013. (HNC, head and neck cancer). The lowest age of patients submitted to IMRT was four years, with diagnosis of brain tumor, and the highest, 91 years, with diagnosis of left maxillary sinus tumor (Table 1). Median age at IMRT was 59.5 years, with 25th percentile at 44 years, and 75th percentile at 67.75 years. Men corresponded to 64% of IMRTs, principally for prostate cancer. About 55% of the brain treatments were performed in women. IMRT corresponded to about 35% of the treatments in cases where the primary site was the skull and about half of the treatments were for anal canal and prostate tumors. Few indications of the technique were observed for breast tumors, gastrointestinal tumors and tumors in other sites, at the beginning of the technique implementation. The cases of cranial IMRTs included hypophyseal tumors and cases where IMRT was associated with hypofractionation, with concomitant boost RT in only one treatment phase, besides treatments of high-grade gliomas. Eighteen patients underwent combined chemotherapy/oral temozolemide in cases where histological analysis indicated high-grade glioma. In cases of head and neck tumors, both combined RT/]chemotherapy (73%) and postoperative adjuvant therapy (19%) were indicated. On average, the number of fields and segments was higher than in other primary sites. Also, interruption was observed at some point of the treatment in 13% of the patients, and cases of mucositis and/or radioepithelitis (grade > 3) were observed in five patients. In cases of prostate IMRT, 57% of the treatments were associated with hormone therapy. Such cases include combined RT (either with or without hormone therapy) and adjuvant or salvage RT following radical prostatectomy. Acute actinic rectitis and/or dysuria grade > 3 was observed in 7.5% of the patients and required treatment interruption for 3 to 5 days for recovery. The authors observed a tendency towards indication of IMRT in a higher number of cases. According to Figure 3, in 2013 IMRT represents 24% of the treatments as compared with 16% in 2012 and 14% in 2011. Also, such a tendency may be proved with the number of IMRT plannings corresponding to 20 in 2013. In the previous years, such a number was 13 and 14.5, respectively in 2011 and 2012 (Figure 4). 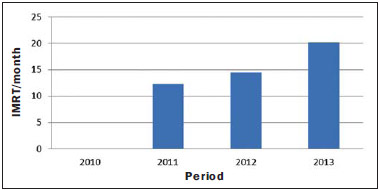 Figure 4. Average number of IMRT plannings per year. DISCUSSION In 2012, estimates indicated the occurrence of 520,000 cases of cancer in Brazil, responsible for 17% of deaths in the country. Approximately 293,000 would require RT(3). The Brazilian government oncology-related expenditures overcome R$ 1.9 billion, not including states, cities and private investments. RT expenditures corresponded to 11.7% of the invested amount(4). Despite the increasing investments in oncology-related care, patients requiring RT still face excessively long waiting time for treatment. In the country, according to the Federal Audit Court - TCU (Tribunal de Contas da União) in a report evaluating the oncology-related care to SUS's users, such a waiting time was estimated to be 113.4 days following the diagnosis, and only 15.9% of treatments were started within the first 30 days(4). The situation the State of São Paulo is a little bit better with 46.6-day waiting time and 52.4% of treatments started within 30 days(4). As compared with international standards, in Canada the median waiting time for RT is six days, and in the United Kingdom, 15 days(5,6). Among the cases included in the present study, the mean waiting time was 49 days following the indication for RT, and 50% of patients started the treatment in up to 30 days after the diagnosis. Also, it was observed that 87% of the patients with diagnosis of brain tumors started IMRT in less than 30 days after the diagnosis, as well as 55% of the patients with diagnosis of head and neck tumors, and 37% of those with diagnosis of prostate tumors. Currently, there are 284 RT apparatuses with the most different technical specifications installed in the whole country. It is estimated that the country is in short of additional 135 apparatuses to appropriately and timely meet the countrywide demand for RT(4). There is a pressing necessity not only for expansion of the number of installed services, but also for insertion of modern technologies into SUS. A survey developed with oncologists responsible for assistance to SUS patients, demonstrated that delay in studies, tests and treatments, particularly RT, was one of the main faults of the public system of oncologic patients care. Additionally, 84.8% of the interviewed physicians highlighted the impossibility of application, in their clinical practice within SUS, of therapeutic approaches recognized by international scientific studies, and that 66.9% of such oncologists define as inappropriate the system for updating compensated values and procedures included in the SUS list of procedures. In such a context, IMRT is one of these procedures that are not covered by SUS. In those interviews, approximately 20% of the oncologists have mentioned the indication and the actual necessity of modern RT, highlighting IMRT as a relevant resource to be offered to patients assisted by SUS. Considering the current situation in terms of RT apparatuses installed in the whole country and the tables of procedures covered by SUS, one observes that only seven out of the 21 services capable of offering the IMRT technique in the country allocate total or part of the procedures to SUS' patients(4). Up to the present moment, HCFMRP-USP was one of the institutions that provided the highest number of treatments with the IMRT technique for SUS' patients. In a recent review discussing the reasoning for a rational utilization of IMRT, the questioning was about how much this technique could improve the local management of the disease, considering the enhanced conformal capability and lower toxicity for organs at risk(7). It also reports that, after 20 years, IMRT became a standard in the treatment of all tumors, with increasing requirements in terms of competence of RT services, team training, financial and equipment resources, besides of the access of the population to IMRT. Some of such questions had to be resolved in the process of IMRT implementation at the authors' institution, particularly those related to the education of a specialized team in spite of the below-average wages in the public sector; to the technical capacitation and stimulation of the team; and to the appropriateness of indications before the patients' demand for RT. The rational utilization of IMRT is justified by clinical evidences, institutional protocols, patients' clinical conditions and socioeconomic factors. Public sector expenses with a more expensive technique are not justifiable if such factors are not well established, since the clinical evidences supporting the utilization of IMRT are still limited to some types of cancer. Only 8 randomized clinical studies comparing IMRT with non-IMRT techniques (4 about breast cancer (8-11) and 4 about head and neck cancer(12-15)), and other 80 comparative studies have been found in the literature for the last 20 years(8). According to controlled studies, up to the present moment, IMRT has not changed the patients' survival, despite the existence of clinical studies and series reports suggesting such benefit for different tumor sites. Most studies report lower toxicity which by itself could justify the use of IMRT in the clinical routine. In the present study, the authors observed an index of 11% of toxicity grade 3/4. Sites presenting with higher indices include: head and neck (23%); prostate (7.5%); and skull (10%). Another potential IMRT benefit is the hypofractionation (treatment with fewer, larger daily fractions). It is the authors' opinion that this is one of the greatest benefits from IMRT for the institutions, considering that the treatment period can be shortened and so the waiting time can be reduced. Developments of the technique, the institutional learning curve, and the lack of an imaging-guided daily localization system have hindered a more extensive utilization of more concise treatments. In the present study, 9.81% of the patients with diagnosis of head and neck cancer were submitted to IMRT. Such patients presented with favorable clinical conditions and tumor staging with great healing potential despite their advanced disease, justifying the reduction of the risk for late toxicity, particularly xerostomia. About 65% of the patients were at the age of < 60 years at the diagnoses. There are three randomized studies demonstrating reduction of xerostomia and better quality of life in patients submitted to IMRT(16). Additionally, four randomized studies approaching breast cancer identify the benefits from IMRT in terms of reduction of both acute and late toxicity to the skin(8), besides a positive impact on the patients' quality of life. In the present study, indications of IMRT for breast cancer were restricted to 2% of cases. According to the institution's protocol, all the patients underwent 3DRT of breast. IMRT is made available as an alternative only in cases where the conformal planning delivers prohibitive radiation doses to risk organs, such as lungs and heart. As regards treatment of prostate cancer, only three case series are found the literature, the largest one with 1571 patients, reporting a significant reduction of toxicity to the genitourinary and gastrointestinal tracts. Five-year quality of life also presented significant improvement with IMRT(17). The indication for treatment with IMRT in 15.48% of cases was justified by the higher radiation dose to risk organs such as rectum, bladder and femoral head in the attempt of conformal planning. About 50% of the indications occurred for patients who had already undergone surgery and required adjuvant or salvage RT at prostate site. At this second year of the technique implementation, gold seeds have been implanted as fiducial markers for IGRT and hypofractionation has been proposed for treatment of prostate cancer. In the present study, the highest number of IMRT indications occurred for brain tumors, corresponding to 28% of all IMRTs and 30% of brain cancer treatments. Among others, gliomas, hypophyseal tumors, medulloblastomas, meningiomas were included in this group. About 60% of IMRTs were performed in patients with diagnosis of high-grade gliomas. IMRT indications have not increased significantly in the second year of the technique implementation, but the authors have observed a higher number of indications for extremity sarcomas and gynecologic/pelvic sarcomas. Equalizing the offering of modern technologies before the huge demand for RT has been a constant challenge. Based on the results of the present study, the authors conclude that the inclusion of IMRT in the SUS procedures list is feasible for cases where its indication is justifiable, principally because of the lowest index of toxicity and improvement in the patients' quality of life as reported in the international literature. Hypofractionation may contribute to reduce the waiting time, but careful attention must be paid to the increase in toxicity as a result of the radiation dose scaling. The high cost of apparatuses in association with high taxes, difficulties in SUS accreditation, team training and issues related to wages also represent a great challenge in the offering of IMRT by SUS. Acknowledgements To the residents of radiotherapy Luiz Henrique de Almeida Ventura and Gabriele Chiamulera. To the medical physicists Edenyse Cristhiane Bertucci Martins and Adriano Bianchini. To the staff of the Radiotherapy Service of HCFMRP-USP. REFERENCES 1. Brasil. Constituição da República Federativa do Brasil. Brasília, DF: Centro Gráfico do Senado Federal; 1988. 2. Brasil. Ministério da Saúde. Conselho Nacional de Saúde. Lei Orgânica do SUS - Lei Nº 8.080, de 19 de setembro de 1990. Brasília, DF. 3. Instituto Nacional de Câncer José Alencar Gomes da Silva. Estimativa 2012 - Incidência de câncer no Brasil. Rio de Janeiro, RJ: INCA; 2011. 4. Tribunal de Contas da União (TCU). Acordão nº 2843/2011. Processo TC 031.944/2010-8. Sessão 25/10/2011. [acessado em 22 de junho de 2012]. Disponível em: http://portal2.tcu.gov.br/portal/page/portal/TCU/imprensa/noticias/detalhes_noticias?noticia= 3898750.. 5. Cancer Research UK. Achieving a world-class radiotherapy service across the UK. A report for Cancer Research UK. (2009). [acessado em 20 de abril de 2012]. Disponível em: www.cancerresearchuk.org/prod_consump/groups/cr_common/@nre/@pol/documents/generalcontent/crukmig_1000ast-3360.pdf. 6. Canadian Institute for Health Information. Wait Times in Canada - A Summary, 2012. [acessado em 20 de abril de 2012]. Disponível em: https://secure.cihi.ca/free_products/WaitTimesSummary2012_EN.pdf. 7. De Neve W, De Gersem W, Madani I. Rational use of intensity-modulated radiation therapy: the importance of clinical outcome. Semin Radiat Oncol. 2012;22:40-9. 8. Pignol JP, Olivotto I, Rakovitch E, et al. A multicenter randomized trial of breast intensity-modulated radiation therapy to reduce acute radiation dermatitis. J Clin Oncol. 2008;26:2085-92. 9. Livi L, Buonamici FB, Simontacchi G, et al. Accelerated partial breast irradiation with IMRT: new technical approach and interim analysis of acute toxicity in a phase III randomized clinical trial. Int J Radiat Oncol Biol Phys. 2010;77:509-15. 10. Barnett GC, Wilkinson JS, Moody AM, et al. Randomized controlled trial of forward-planned intensity modulated radiotherapy for early breast cancer: interim results at 2 years. Int J Radiat Oncol Biol Phys. 2012;82:715-23. 11. Donovan E, Bleakley N, Denholm E, et al.; Breast Technology Group. Randomised trial of standard 2D radiotherapy (RT) versus intensity modulated radiotherapy (IMRT) in patients prescribed breast radiotherapy. Radiother Oncol. 2007;82:254-64. 12. Kam MK, Leung SF, Zee B, et al. Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol. 2007;25:4873-9. 13. Nutting CM, Morden JP, Harrington KJ, et al.; PARSPORT trial management group. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multi-centre randomised controlled trial. Lancet Oncol. 2011;12:127-36. 14. Pow EH, Kwong DL, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys. 2006;66:981-91. 15. Longobardi B, De Martin E, Fiorino C, et al. Comparing 3DCRT and inversely optimized IMRT planning for head and neck cancer: equivalence between step-and-shoot and sliding window techniques. Radiother Oncol. 2005;77:148-56. 16. Caglar HB, Allen AM. Intensity-modulated radiotherapy for head and neck cancer. Clin Adv Hematol Oncol. 2007;5:425-31. 17. Zelefsky MJ, Levin EJ, Hunt M, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70:1124-9. 1. PhD, Professor and Coordinator, Service of Radiotherapy at Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 2. PhD, Professor, Collaborator of Fundação de Apoio ao Ensino, Pesquisa e Assistência (Faepa) – Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil 3. PhD, MD, Radiotherapist, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 4. MD, Radiotherapist, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 5. PhD, Medical Physicist, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 6. Master, Medical Physicist, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 7. Medical Physicist, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 8. PhD, Professor and Coordinator, Service of Clinical Oncology, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil Mailing Address: Dr. Harley Francisco de Oliveira Avenida Bandeirantes, 3900, Campus Universitário, Monte Alegre Ribeirão Preto, SP, Brazil, 14048-900 E-mail: harley@fmrp.usp.br Received September 3, 2013. Accepted after revision May 5, 2014. Study developed at Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554