Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 6 - Nov. / Dec. of 2014
Vol. 47 nº 6 - Nov. / Dec. of 2014
|
ORIGINAL ARTICLE
|
|
Dosimetry and image quality assessment in a direct radiography system |
|
|
Autho(rs): Bruno Beraldo Oliveira1; Marcio Alves de Oliveira2; Lucas Paixão1; Maria Helena Araújo Teixeira3; Maria do Socorro Nogueira4 |
|
|
Keywords: Mean glandular dose; Image; Direct radiography. |
|
|
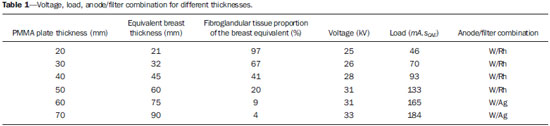
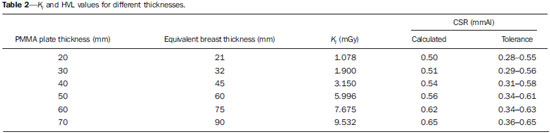
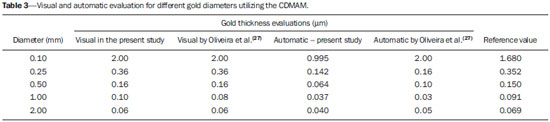
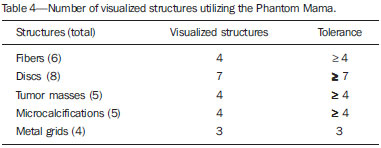
Abstract: INTRODUCTION
Mammography is the radiographic technique that plays a fundamental role in the detection and diagnosis of clinical abnormalities in the breast. It is the method of choice in the screening for breast cancer in asymptomatic women, allowing for the reduction of patients' mortality(1). Two types of mammography are currently available, namely, the conventional type, which utilizes radiographic film cassette and intensifying screens, and the digital type, relying on computed radiography (CR) and direct radiography (DR). The CR systems are equipped with an image digitizer and utilize cassettes containing phosphor imaging plates, while the DR systems rely on digital detectors. Digital mammography enables the incorporation of a number of new technologies, such as digital breast tomosynthesis (DBT)(1), which utilizes a sequence of views acquired along a limited arch around the breast. Recently, several studies in several areas have been published in Brazil, aimed at improving the radioprotection methods(2-4) and demonstrating the importance of the adoption of an appropriate dosimetry procedure(5-11). Particularly in mammography, there is a preoccupation on evaluating the quality of the mammography apparatuses by means of specific performance tests(12-14), with the purpose of providing more accurate and precise diagnosis(15,16). Breast dosimetry plays a relevant role in the equipment quality control and is an essential element in the optimization of the procedures. The International Commission on Radiation Units and Measurements (ICRU)(17) recommends the utilization of the mean dose for glandular tissues, without utilizing the breast as a whole for dosimetry in mammography. This quantity is referred to in the literature as mean glandular dose (DG). There are several standard protocols for dose estimation that provide conversion factors which correlate the incident air kerma (Ki) with DG (18). In the protocols from the Commission of the European Communities (CEC)(13) and from the International Atomic Energy Agency (IAEA)(14), such factors are based on Monte Carlo calculations developed by Dance(19,20) and are available for x-ray spectra from different anode-filter combinations. The study developed by Dance et al.(20) included equivalent thicknesses of polymethylmethacrylate (PMMA) plates which may be utilized to simulate the typical breasts of different thicknesses for dosimetry purposes. In the protocols from the American College of Radiology (ACR), the utilized conversion factor is that calculated by Wu et al.(21,22) and Boone(23,24) by means of Monte Carlo calculations tabulated for different beam qualities, thicknesses and breast glandularity. The Health Surveillance Agency from the State of Minas Gerais, Brazil, in a partnership with Centro de Desenvolvimento da Tecnologia Nuclear (Center for the Development of Nuclear Technology) (CDTN/CNEN), evaluates digital mammography apparatuses in the State(25) on a yearly basis, by means of performance tests based on the CEC(13) and IAEA(14) protocols, with the purpose of verifying whether the obtained results are in compliance with the digital mammography quality assurance program established by IAEA(14). Performance testing includes collimation system (alignment of the x-ray field with the luminous beam); compression force; alignment of the compression paddle; detector response linearity and uniformity; spatial resolution; contrast noise and signal noise ratios. The present study was aimed at performing complementary dosimetry tests together with imaging quality assessment, utilizing the same protocol adopted by the Health Surveillance Agency in a mammography apparatus equipped with the DR system. Such an apparatus was utilized on account of a partnership established with a mammography clinic located in the city of Belo Horizonte, interested in participating in research projects. At dosimetry, the DG results obtained for different PMMA plate thicknesses were estimated by utilizing a solid state detector, with the purpose of comparing such results with the values provided by the adopted equipment. The solid state detector was selected instead of a traditional specific ionization chamber for mammography, on account of its many advantages. Such detectors have a specific material in the lower part to avoid the detection of backscattered radiation, are easier to position and are more stable. Additionally, they directly provide the values of the half value layer (HVL) with a low response time thus allowing swiftness in the experiments and, consequently, reducing the idle time of the equipment at mammography clinics. The obtained DG results were also compared with internationally established acceptable and desirable reference levels(13,14). Two different phantoms were utilized for the image quality test: the Phantom Mama, indicated by Colégio Brasileiro de Radiologia e Diagnóstico por Imagem, and the CDMAM, specific for digital apparatuses. All the images were analyzed and the results were compared with the established reference values(13,26). MATERIALS AND METHODS The DG values are estimated from the Ki values obtained in the irradiations and conversion coefficients that are tabled and dependent upon the HVL of the x-ray beam. The exposures were performed by utilizing the solid state detector Unfors 8202031-H Xi R/F & MAM Detector Platinum and the DR system of the Hologic Selenia Dimensions mammography apparatus located at a mammography clinic in the city of Belo Horizonte. The image from the Phantom Mama was only visually evaluated, while the CDMAM images were both visually and automatically analyzed by the cdcom.exe software. Exposure parameters determination The irradiations for determining exposure parameters were performed by utilizing the automatic exposure control (AEC) of the equipment and PMMA plates with thicknesses ranging from 20 to 70 mm positioned on the compression apparatus. In order to represent breasts with different attenuations, PMMA spacers with thicknesses of 1, 2, 5, 10 and 20 mm were placed on the plates (Figure 1). All voltage values (kV), load (mA.sCAE) and anode/filter composition were recorded for each thickness. 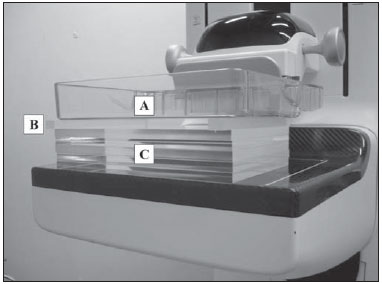 Figure 1. Positioning of materials in the determination of exposure parameters. A: Breast compression paddle. B: PMMA spacers. C: PMMA plates. Determination of the Ki and HVL values The distance between the focal point of the x-ray tube and breast compression paddle was 700 mm. The solid state detector was positioned on the breast paddle with its sensitive center at 60 mm from the chest wall (Figure 2). 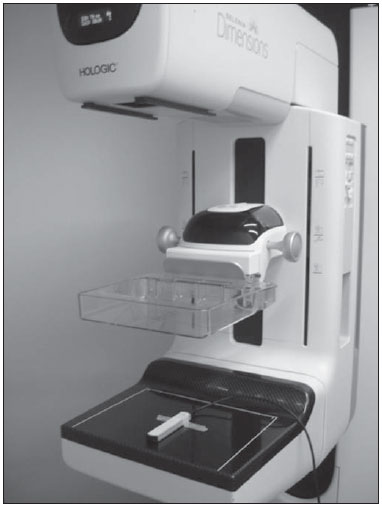 Figure 2. Solid-state detector positioning for measurement of Ki and HVL. The Ki values were determined by utilizing the readings obtained with the mammography apparatus in the manual exposure mode and the obtained exposure parameters in the irradiations with AEC, according to the equation: Ki,25 = MCAE N kTP where: Ki,25 is the Ki value obtained with the sensitive center of the solid state detector positioned at 25 mm from the breast compression paddle; MCAE is the average value of the three readings; N is the value of the calibration factor; and kTP is the factor for correction of temperature and pressure(14). For the measurements with the plates and PMMA spacers, the Ki values were obtained by means of the equation: Ki,t = Ki,25 [(d – 25) / (d – t)]2 where: Ki,t is the Ki value obtained for a t thickness; d is the distance between the focal point of the x-ray tube and the breast compression paddle; and t is the sum of the thicknesses of the PMMA plates and spacers(14). In case it was not possible to select the same load value, the reading values were estimated by utilizing the load value closer to the value utilized with the AEC, as per the equation: MCAE = M (mA.sCAE / mA.sM) where: mA.sCAE is the load value utilized with the AEC; M is the average value of the three readings utilizing the closest load value, mA.sM(14). The HVL were obtained by the solid state detector that automatically provides such values after each irradiation. The respective tolerances of such values were obtained according to the interval: kV / 100 + 0.03 < HVL < kV / 100 + C where: C is a constant with the values 0.12; 0.19; 0.22; 0.30; 0.32; 0.25 for the anode/filter combinations Mo/Mo, Mo/Rh, Rh/Rh, W/Rh, W/Ag, W/Al, respectively(14). Determination of the DG values The DG values were obtained according to the equation: DG = gt ct s Ki,t where: gt is the factor that converts the Ki into DG by utilizing a breast with 50% of fibroglandular tissue and 50% of fat tissue and a thickness t; ct is the conversion factor that allows the utilization of other breast composition; s is the factor for different anode/filter combinations(14,19,20). The results were compared with internationally established, acceptable and desirable reference levels(13,14). Evaluation of image quality The irradiations for the first image quality evaluation were performed with the AEC of the equipment, besides the CDMAM phantom inserted between four PMMA plates positioned on the breast paddle (Figure 3). In total, 12 images were obtained without processing, with the purpose of enabling a reliable result from the cdcom.exe software. A visual analysis of one of the images was performed for comparison with the automated analysis. The evaluation of the images was performed by means of the gold thicknesses with different diameters present in the CDMAM phantom. The results were compared with the established reference values(13).  Figure 3. CDMAM phantom positioning for evaluation of image quality. The irradiation for the second image quality evaluation was also performed by utilizing the equipment's AEC, this time utilizing the Phantom Mama positioned on the breast paddle (Figure 4). The respective non-processed image was obtained and the image evaluation was performed by visualization of the different structures present in the Phantom Mama. The anatomical structures simulated by the structures visualized on the Phantom Mama image include tumor masses; microcalcifications; low-contrast areas or lesions and fibrotic calcifications. The number of each structure was compared with the established reference values(13,26). 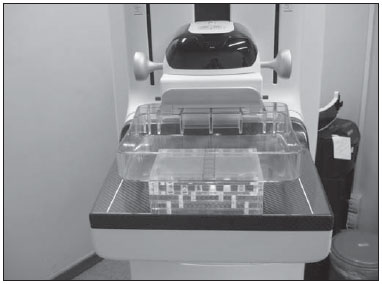 Figure 4. Phantom Mama positioning for evaluation of image quality. RESULTS Determination of the exposure parameters Voltage, load values and anode/filter combination utilized for different thicknesses are shown on Table 1. The proportion of fibroglandular tissue and the equivalent breast thickness was obtained by the sum of the respective PMMA plate and spacer thicknesses(14). Determination of Ki and HVL values The Ki values in mGy, besides the HVL values and their respective tolerances in mmAl obtained for different thicknesses are shown on Table 2. The calculated relative expanded uncertainty (k = 2) for measurements of Ki and HVL is approximately 7.6%. Determination of DG values The calculated DG values in mGy with the respective measurement uncertainties for different PMMA thicknesses, and the respective maximum acceptable and desired levels established by CEC(13) and IAEA(14) are shown on Figure 5. The calculated relative expanded uncertainty (k = 2) for the DG measurements is approximately 9.0%. The calculated DG values ranged between 0.54 ± 0.04 and 2.63 ± 0.24 mGy for the different thicknesses. Figure 5 also indicates the values provided by the DR system, besides the results obtained by Oliveira et al.(27) utilizing a CR system. 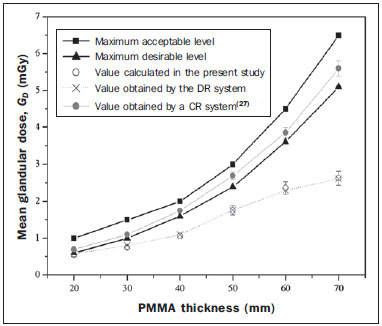 Figure 5. Mean glandular dose for different thicknesses. Image quality evaluation The visual and automatic evaluations of the gold thickness on the CDMAM images obtained in the present study and by Oliveira et al.(27), besides the respective reference values(13) in µm for different material diameters, are shown on Table 3. The number of each visualized structure utilizing the image obtained from the Phantom Mama is shown on Table 3. The number of each visualized structure utilizing the Phantom Mama, besides the respective tolerances(13,26), are shown on Table 4. DISCUSSION The PMMA plates and spacers are easily manipulated and allow for obtaining the correct equivalent breast thicknesses, besides the respective fibroglandular tissue proportions. Such parameters are necessary to allow for determining DG values and verify whether the equipment is correctly providing such values. However, a careful approach is necessary in analysis of results obtained with such materials, as they might be different from those obtained at dosimetry on an actual breast. In their studies, Cassola et al.(28) have concluded that homogeneous materials should be utilized for constancy tests and are not indicated to estimate dosimetry in actual patients. In the present study, DG values increased with the PMMA thickness, and the highest value was found when a 70 mm-thick PMMA plate was utilized, as it has the highest x-ray attenuation. Chen et al.(29) and Chevalier et al.(30) have observed that DG values are a function of the compressed breast thickness. For that reason, the result obtained in the present study was expected, as greater thicknesses require more energetic beams, besides a higher number of photons, causing an increase in dose values. Coutinho(31) has collected clinical data from 1,183 mammograms obtained by different systems, namely, screen/film, CR and DR. From such a sample, DG values for 392 patients were calculated with thermoluminescent (TL) dosimeters and a solid state detector. In the comparison of the two dosimetry methods in the determination of the DG values obtained from Ki and of the tabled conversion factorswere up to 30% higher than the values obtained by direct measurements utilizing the TL dosimeters within a specific phantom. In the present study, the DG results show that the results with the solid state detector were in agreement with the values shown by the equipment, and that such values were below the desirable level for all studied different thicknesses and breast glandularities. However, such values may be overestimated. For this reason, in future studies, it would be interesting to perform measurements utilizing TL dosimeters and a phantom in order to determine the difference between the methods. Coutinho(31) has also concluded that the utilized DR systems presented DG values higher than those calculated with the phantom, and that the mean DG values obtained in those apparatuses are 33% lower than in the screen/film system. However, the CR systems evaluated in that study presented mean DG values 25% higher than the conventional systems. In the digital imaging systems, both DR and CR, automatically adjust the radiation exposure, which contributes to a possible reduction in the number of acquired images. The DR systems also provide a better workflow as they eliminate the utilization of film cassettes, and provide greater opportunities to incorporate new technologies such as the DBT system. In Brazil, one observes an increasing tendency towards adopting digital systems in lieu of conventional ones. For this reason, it is important to compare the obtained DG values between the different digital systems. Oliveira et al.(27) have published DG values obtained with the same method utilized in the present study, but with a CR system of a laboratory in the State of Minas Gerais. All results were within the internationally acceptable and desirable reference levels(13,14), but above the results calculated with the DR system in the present study. In general, despite the elevated results presented by the CR systems, there is still room for dose reduction. It is more difficult to identify overexposure in such systems on account of the automatic adjustment of image brightness and contrast. For this reason, the optimization of the procedures is important to reduce the exposure to acceptable levels while maintaining appropriate image quality. Cassola et al.(28) have compared dosimetry data between different breast phantoms (homogeneous breast phantom and anthropomorphic breast phantom). They recommended the Dance(19,20) model as the best one to evaluate dose values in median breasts with glandular tissue in the medial region. This is the same model utilized in the present study, with basis on DG values instead of that utilized by Wu et al.(21,22) and Boone(23,24), based on the normalized glandular dose. As the questions related to radiological protection were considered, the model proposed by Dance(19,20) was also recommended, even though such model underestimates all calculated values for normalized glandular dose. In their study, Oliveira et al.(32) have concluded that the reference dose level is reached when optimum quality images are produced. The image noise is a limiting factor for radiation dose reduction. Thus, the images obtained with DR systems have a greater potential for reducing irradiation because of a better image quality obtained from a lower exposure. Chen et al.(29) have concluded that the DR systems can provide images with similar quality, from a wide range of dose values. Measurements performed with digital systems utilizing phantoms demonstrated that the image quality is similar when the dose is reduced by up to 50% or 30%, depending on the phantom(29,33). In the present study, considering that the radiation dose in mammography must be kept as low as reasonably achievable without decrease in image quality, in addition to the calculation of the DG values, tests were performed to evaluate the quality of images acquired with the studied equipment with the purpose of assuring a minimum quality for diagnosis. The first evaluation of image quality with this equipment was performed by means of visual and automatic analysis of the images obtained with the CDMAM phantom. In the automatic analysis performed by the cdcom.exe software, the results were slightly different from those reported by Oliveira et al.(32), but all of such results were below the reference values(13) established for each gold diameter. Considering that the visual analysis is not as accurate as the automatic analysis, the visualized results were also considered as being compliant with the reference values, besides being very similar to those found by Oliveira et al.(32). The second evaluation of image quality was performed by means of visual analysis of the image obtained with the Phantom Mama. The number of each visualized structure is compliant with the tolerances(13,26). From the image of this phantom, it was also possible to attain the third metal grid, i.e., one can estimate that the spatial resolution of this equipment corresponds to eight pairs of lines per millimeter. CONCLUSIONS In the present study, the calculated DG values were compared with reference levels(13,14), in addition to the values provided by the adopted DR system. Several studies have demonstrated that the DG values increase with the x-ray attenuation caused by the compressed breast thickness, or, in the present case, by the addition of PMMA plates and spacers.(29-31) As the measurement uncertainties are considered, all DG values are in compliance with the reference desirable levels(13,14) and with the values provided by the DR system for the respective thicknesses. Additionally, the present study allows for the conclusion, by means of the comparison with the results obtained with a specific apparatus and a CR system(27), that the choice of such mammography equipment with a DR system did not cause any increase in the DG values. The wearing and metallization of the x-ray tube represent factors that may result in decrease of performance values (mGy.mAs–1) of the equipment with time. Thus, in order to maintain the same image characteristics, the AEC increases the radiographic technique, maintaining a constant Ki value. Considering that DG values are obtained from Ki values, these are also invariable, and, therefore, utilized in comparisons with different apparatuses and internationally established reference levels. For radiological protection, in addition to dosimetry of the equipment, it is necessary to assess image quality. For this reason, in the evaluation of the images acquired from the two phantoms, all the results were in compliance with the reference values and tolerances(13,26). Based on such results, one concludes that the analyzed images present a correct contrast threshold and appropriate spatial resolution, besides allowing for the differentiation of pertinent anatomical structures for an accurate and precise diagnosis. Therefore, the present study contributes to evaluate the compliance of the equipment in relation to dose and image quality. However, as the present study evaluated a single mammography apparatus, further studies will be required to perform dosimetry and image assessments in a larger sample, with different equipment and characteristics and from different manufacturers, with the purpose of concluding on the dose and image quality in digital mammography. Acknowledgements The authors wish to thank Comissão Nacional de Energia Nuclear (CNEN) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes), for the doctoral scholarships, and Dra. Maria Helena Araújo Teixeira, for providing the DR system. The present study was supported by Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Fapemig) and by Instituto Nacional de Ciência e Tecnologia (INCT) em Metrologia das Radiações em Medicina. REFERENCES 1. Chala LF, Barros N. Avaliação das mamas com métodos de imagem. Radiol Bras. 2007;40(1):iv-vi. 2. Soares FAP, Pereira AG, Flôr RC. Utilização de vestimentas de proteção radiológica para redução de dose absorvida: uma revisão integrativa da literatura. Radiol. Bras. 2011;44:97-103. 3. Hoff G, Andrade JRM, Fischer ACFS, et al. Ferramenta computacional para avaliação de kerma no ar em aplicações de radioproteção em áreas de internação de pacientes: proposição de um método simples para avaliação experimental. Radiol Bras. 2012;45:71-81. 4. Figueiredo FM, Gama ZAS. Melhoria da proteção radiológica mediante um ciclo de avaliação interna da qualidade. Radiol Bras. 2012;45:87-92. 5. Pina DR, Duarte SB, Ghilardi Netto T, et al. Controle de qualidade e dosimetria em equipamentos de tomografia computadorizada. Radiol Bras. 2009;42:171-7. 6. Dalmazo J, Elias Júnior J, Brocchi MAC, et al. Otimização da dose em exames de rotina em tomografia computadorizada: estudo de viabilidade em um hospital universitário. Radiol Bras. 2010;43:241-8. 7. Silva MSR, Khoury HJ, Borrás C, et al. Dosimetria de pacientes e médicos em intervenções coronárias percutâneas em Recife, Pernambuco, Brasil. Radiol Bras. 2011;44:90-6. 8. Sabino T, Rodrigues LN, Furnari L, et al. Caracterização dosimétrica de feixes de fótons com detector de diamante. Radiol Bras. 2012;45:35-8. 9. Navarro VCC, Navarro MVT, Maia AF, et al. Avaliação de exposições médicas em procedimentos pediátricos de radiologia intervencionista. Radiol Bras. 2012;45:210-4. 10. Rodrigues SI, Abrantes AF, Ribeiro LP, et al. Estudo da dose nos exames de tomografia computadorizada abdominal em um equipamento de 6 cortes. Radiol Bras. 2012;45:326-33. 11. Oliveira BB, Mourão AP, Silva TA. Estimativa dos valores de MSAD em procedimentos de tomografia computadorizada utilizando filmes radiocrômicos. Radiol Bras. 2013;46:96-100. 12. Agência Nacional de Vigilância Sanitária. Radiodiagnóstico médico: segurança e desempenho de equipamentos. Brasília: Editora Anvisa; 2005. 13. Commission of the European Communities. European guidelines for quality assurance in breast cancer screening and diagnosis. Luxembourg: CEC; 2006. 14. International Atomic Energy Agency. Quality assurance programme for digital mammography. Vienna: IAEA; 2011. 15. Rodrigues DCN, Freitas-Junior R, Corrêa RS, et al. Avaliação do desempenho dos centros de diagnóstico na classificação dos laudos mamográficos em rastreamento oportunista do Sistema Único de Saúde (SUS). Radiol Bras. 2013;46:149-55. 16. Goto RE, Pires SR, Medeiros RB. Identificação de parâmetros de qualidade de impressão para a garantia da detecção de estruturas presentes na mamografia digital. Radiol Bras. 2013;46:156-62. 17. International Commission on Radiation Units and Measurements. Patient dosimetry for x rays used in medical imaging (Report 74). Bethesda: ICRU; 2006. 18. Dance DR, Young KC, van Engen RE. Further factors for the estimation of mean glandular dose using the United Kingdom, European and IAEA breast dosimetry protocols. Phys Med Biol. 2009; 54:4361-72. 19. Dance DR. Monte Carlo calculation of conversion factors for the estimation of mean glandular breast dose. Phys Med Biol. 1990;35: 1211-9. 20. Dance DR, Skinner CL, Young KC, et al. Additional factors for the estimation of mean glandular breast dose using the UK mammography dosimetry protocol. Phys Med Biol. 2000;45:3225-40. 21. Wu X, Barnes GT, Tucker DM. Spectral dependence of glandular tissue dose in screen-film mammography. Radiology. 1991;179:143-8. 22. Wu X, Gingold EL, Barnes GT, et al. Normalized average glandular dose in molybdenum target-rhodium filter and rhodium target-rhodium filter mammography. Radiology. 1994;193:83-9. 23. Boone JM. Glandular breast dose for monoenergetic and high-energy X-ray beams: Monte Carlo assessment. Radiology. 1999;213:23-37. 24. Boone JM. Normalized glandular dose (DgN) coefficients for arbitrary X-ray spectra in mammography: computer-fit values of Monte Carlo derived data. Med Phys. 2002;29:869-75. 25. Nogueira MS, Oliveira MA, Joana GS, et al. Avaliação da qualidade e requisitos de proteção radiológica em mamografia digital e monitoramento dos serviços de mamografia de Minas Gerais. Gerais: Revista de Saúde Pública do SUS/MG. 2013;1:91-2. 26. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Mamografia: da prática ao controle. Rio de Janeiro: INCA; 2007. 27. Oliveira MA, Dantas MVA, Santana PC, et al. Assessment of glandular dose and image quality in mammography using computerised radiography employing a polymethylmetacrilate breast simulator. Proceedings of the 16th Solid State Dosimetry Conference, 2011 Sep 19-24; Sidney, Australia. Radiat Meas. 2011;46:2081-5. 28. Cassola VF, Hoff G. Estudo comparativo de dosimetria computacional entre modelos homogêneos e um modelo voxel em mamografia: uma discussão de aplicações em testes de constância e cálculo de dose glandular em pacientes. Radiol Bras. 2010;43:395-400. 29. Chen B, Wang Y, Sun X, et al. Analysis of patient dose in full field digital mammography. Eur J Radiol. 2012;81:868-72. 30. Chevalier M, Morán P, Ten JI, et al. Patient dose in digital mammography. Med Phys. 2004;31:2471-9. 31. Coutinho CMC. Avaliação da dose glandular em sistemas de mamografia convencional e digital utilizando um fantoma dosimétrico. [Tese de doutorado]. Rio de Janeiro: Instituto Alberto Luiz Coimbra de Pós-graduação e Pesquisa de Engenharia (COPPE), Universidade Federal do Rio de Janeiro; 2009. 32. Oliveira M, Nogueira MS, Guedes E, et al. Average glandular dose and phantom image quality in mammography. Nuclear Instruments and Methods in Physics Research - Section A. 2007;580:574-7. 33. Huda W, Sajewicz AM, Ogden KM, et al. How good is the ACR accreditation phantom for assessing image quality in digital mammography? Acad Radiol. 2002;9:764-72. 1. Masters, Fellow PhD degree, Course of Science and Technology of Radiations, Minerals and Materials – Centro de Desenvolvimento da Tecnologia Nuclear (CDTN/ CNEN), Belo Horizonte, MG, Brazil 2. Master, Teacher, Department of Anatomy and Imaging, School of Medicine – Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil 3. MD, Radiologist, Technical Director of Clínica Dra. Maria Helena Araújo Teixeira, Belo Horizonte, MG, Brazil 4. PhD, Titular Researcher-Professor, Centro de Desenvolvimento da Tecnologia Nuclear (CDTN), Belo Horizonte, MG, Brazil Mailing Address: Bruno Beraldo Oliveira Centro de Desenvolvimento da Tecnologia Nuclear (CDTN/CNEN) Avenida Presidente Antônio Carlos, 6627, Campus UFMG, Pampulha Belo Horizonte, MG, Brazil, 31270-901 E-mail: boliveira.mg@gmail.com Received August 6, 2013. Accepted after revision April 10, 2014. Study developed in the Program of Post-graduation in Science and Technology of Radiations, Minerals and Materials – Centro de Desenvolvimento da Tecnologia Nuclear (CDTN/CNEN), Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554