RESUMO
Biópsia percutânea guiada por tomografia computadorizada é uma alternativa segura e eficaz para avaliação de lesões intraorbitárias selecionadas, em que o diagnóstico pré-operatório é importante para o planejamento terapêutico. Descrevemos dois casos de pacientes com tumores orbitários incomuns em que o diagnóstico foi obtido por biópsia com agulha grossa guiada por tomografia computadorizada, dando ênfase para os aspectos técnicos do procedimento.
Palavras-chave:
Neoplasias orbitárias; Biópsia por agulha; Tomografia computadorizada; Diagnóstico.
ABSTRACT
Computed tomography-guided percutaneous biopsy is a safe and effective alternative method for evaluating selected intra-orbital lesions where the preoperative diagnosis is important for the therapeutic planning. The authors describe two cases of patients with uncommon primary orbital tumors whose diagnosis was obtained by means of computed tomography-guided core needle biopsy, with emphasis on the technical aspects of the procedure.
Keywords:
Orbital neoplasms; Needle biopsy; Computed tomography; Diagnosis.
INTRODUÇÃO
As biópsias guiadas por métodos de imagem, seja ultrassonografia (US) ou tomografia computadorizada (TC), têm sido largamente aceitas como procedimento efetivo e seguro, com alta acurácia no diagnóstico de tumores em diferentes órgãos(1,2). No entanto, existem poucos relatos da utilização destes procedimentos como método diagnóstico minimamente invasivo nos tumores orbitários.
O objetivo deste trabalho é relatar dois casos de tumores primários da órbita diagnosticados por biópsia percutânea guiada por TC.
RELATO DOS CASOS
Caso 1 - Paciente de 56 anos, masculino, com história de carcinoma papilífero de tireoide, durante exames de controle foi detectado processo expansivo intraorbitário direito na TC de face (Figura 1A). Ao exame físico, apresentava-se sem queixas visuais e com movimentos oculares externos preservados. Foi solicitada ressonância magnética (RM) da órbita, que demonstrou lesão retrobulbar sólidocística na região posterior e superolateral da órbita direita, extraconal, que promovia deslocamento inferomedial do músculo reto superior e do nervo óptico (Figuras 1B e 1C). Exibia aspecto ovalado, de contornos regulares, com realce tardio pós-contraste nas porções sólidas. A lesão media cerca de 28 × 16 × 12 mm. Notava-se afilamento ósseo do teto orbitário adjacente à lesão.
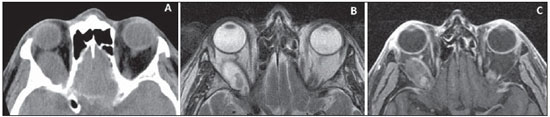
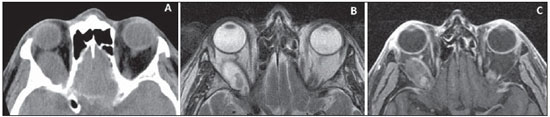
Figura 1.
Caso 1 – Achados de imagem de paciente de 56 anos com lesão orbitária à direita. A: Tomografia computadorizada sem contraste mostrando lesão ovoide retrobulbar à direita, isodensa, de contornos regulares, em íntimo contato com o ápice da órbita. B,C: Ressonância magnética demonstrando a mesma lesão, deslocando medialmente a musculatura extraocular, com alto sinal heterogêneo em T2 (B), apresentando realce após administração do contraste paramagnético nas áreas de mais baixo sinal em T2 (C).
- Paciente de 32 anos, masculino, sem histórico oncológico prévio, com queixa de proptose ocular direita há seis meses. Durante a investigação foi diagnosticado processo expansivo intraorbitário na TC de face (Figura 2). Ao exame físico, apresentava-se sem queixas visuais e com movimentos oculares externos preservados. A RM de órbita (Figura 2) mostrou lesão expansiva extraconal direita na porção inferior e lateral da órbita, deslocando os músculos reto lateral e inferior, apresentando extensão intraconal, sem nítido envolvimento do nervo óptico, que exibia morfologia e intensidade de sinal preservadas. Era bem delimitada, apresentando halo de baixo sinal em todas as sequências, alto sinal em T1, intermediário em T2 e intenso realce ao meio de contraste paramagnético.
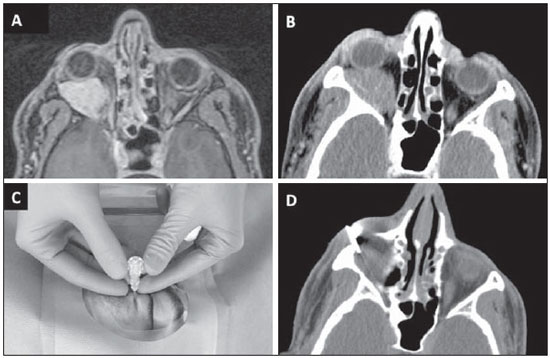
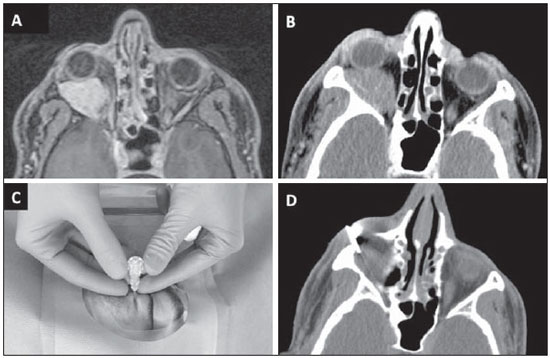
Figura 2.
Caso 2 – Paciente de 32 anos com lesão orbitária à direita. A: Ressonância magnética identificando lesão extraconal à direita, de contornos regulares, deslocando anteriormente o globo ocular e medialmente a musculatura extraocular e nervo óptico, apresentando intenso realce homogêneo após administração do contraste paramagnético. B: Tomografia computadorizada sem contraste mostrando a mesma lesão. C,D: Posicionamento da agulha coaxial por via transpalpebral inferior (C) e corte tomográfico confirmando a localização da ponta da agulha adjacente à lesão (D).
Ambos os pacientes foram submetidos a biópsia percutânea das lesões orbitárias guiada por TC, com anestesia local e sob sedação consciente. Os procedimentos foram realizados pelo método coaxial, com entrada da agulha introdutora coaxial 17-
gauge, via transpalpebral lateral, entre o globo ocular e a asa maior do esfenoide, num trajeto paralelo ao nervo óptico (caso 1) e via transpalpebral inferior, entre o globo ocular e o zigoma, num trajeto inferior à musculatura do músculo reto lateral (caso 2). Após posicionamento das agulhas coaxiais, foram introduzidas as agulhas cortantes de 18-
gauge, sendo colhidos três e cinco fragmentos com disparo de 1,5 cm, respectivamente nos casos 1 e 2, ambos sem intercorrências (Figuras 2 e 3). Os resultados anatomopatológicos das biópsias foram de schwannoma sem indícios de malignidade e neoplasia melanocítica de grau intermediário (melanocitoma), nos casos 1 e 2, respectivamente.
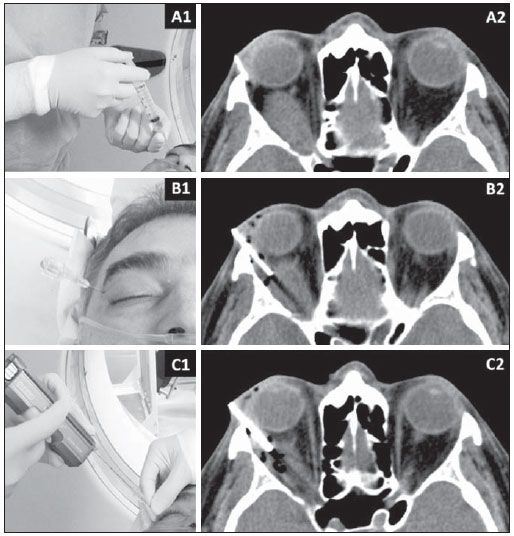
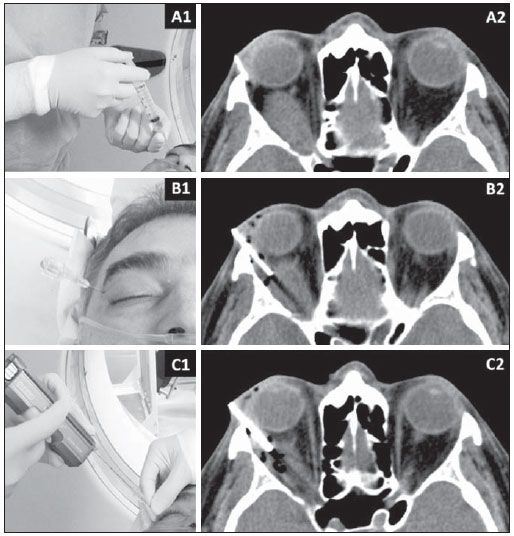
Figura 3.
Caso 1 – Biópsia com agulha grossa guiada por tomografia computadorizada de lesão orbitária à direita. A: Anestesia local com lidocaína 2% no tecido subcutâneo (A1) e corte tomográfico mostrando localização e angulação da agulha (A2) para programação do procedimento. B: Posicionamento da agulha coaxial por via transpalpebral lateral (B1) e corte tomográfico confirmando a localização da ponta da agulha adjacente à lesão (B2). C: Colocação da agulha para biópsia no interior da agulha coaxial para coleta dos fragmentos (C1) e corte tomográfico demonstrando presença de focos gasosos no interior da lesão (C2), que confirmam que os fragmentos foram retirados dessa área.
Optou-se por ressecção cirúrgica, sendo realizada, no caso 1, craniotomia frontal direita com orbitotomia para ressecção radical do tumor, aparentemente relacionado ao complexo neural trigeminal intraorbitário. No caso 2, a orbitomia foi lateral com remoção da parede óssea e ressecção com descolamento cuidadoso da lesão. Ambos os pacientes evoluíram sem complicações no pós-operatório. Os resultados das peças foram coincidentes aos das biópsias, confirmando schwanoma no caso 1 e melanocitoma no caso 2.
DISCUSSÃOSchwannoma é um tumor incomum na órbita, mais comum em adultos, com início insidioso e usualmente não invasivo. A apresentação clínica é variada e pode incluir neuropatia óptica, proptose e diplopia. O tratamento é cirúrgico
(3). Na TC, o schwannoma aparece como lesão retrobulbar ovoide, de contornos regulares, que pode ter localização intra ou extraconal. Na RM, estes tumores são geralmente isointensos à musculatura extraocular nas sequências ponderadas em T1, com hipersinal heterogêneo nas sequências ponderadas em T2 e realce variável pelo contraste. Áreas de alto sinal em T2 estão associadas a áreas de degeneração cística ou mucinosa
(3,4). O diagnóstico definitivo é dificilmente realizado apenas pelos aspectos de imagem, em razão da sobreposição dos achados com outros tumores orbitários. Deste modo, a maioria dessas lesões é diagnosticada após ressecção cirúrgica. Em alguns casos, no entanto, o diagnóstico pré-operatório é fundamental para o adequado planejamento terapêutico.
Os melanocitomas são tumores pigmentares raros no sistema nervoso central, mais frequentemente vistos nas doenças metastáticas. Os locais de acometimento mais comuns são a fossa posterior e a medula espinhal, sendo raro o envolvimento orbitário. O aspecto de imagem dos melanocitomas é de hipersinal nas sequências ponderadas em T1 e T2 na RM, com realce acentuado após injeção do meio de contraste paramagnético. É importante diferenciar as lesões melanocíticas primárias das de origem metastática, pois envolvem diferentes abordagens terapêuticas. A ausência de melanoma maligno conhecido ajuda na diferenciação, sendo importante a investigação completa nestes pacientes em busca do diagnóstico
(5,6).
Neste contexto, as biópsias guiadas por métodos de imagem podem ser úteis na coleta de material adequado para avaliação histológica, com menor morbidade que as biópsias cirúrgicas. Tanto a punção aspirativa por agulha fina (PAAF) como a biópsia por agulha grossa já foram descritas para diagnóstico de lesões orbitárias
(7,8). As vantagens do procedimento orientado pela US em relação à TC são a ausência de radiação ionizante e monitoramento em tempo real da posição da agulha. No entanto, os trabalhos com procedimentos guiados por TC não demonstraram maior número de complicações e o acesso pode ser mais fácil a depender da localização da lesão
(8-11).
Chojniak et al. demonstraram que as biópsias por agulha grossa têm resultados melhores que as PAAFs para coleta de material adequado e definição de diagnósticos específicos, sem aumento do número de complicações
(9). Em levantamento feito por Gupta et al.
(7), em que foram avaliadas 37 PAAFs de tumores de órbita guiadas por US, 22% dos casos tiveram amostra insuficiente para o diagnóstico. No entanto, existem poucos relatos na literatura de core-biópsia guiada por TC para o diagnóstico de lesões orbitárias
(8,10).
Os primeiros relatos na literatura de biópsias por agulha grossa em lesões orbitárias foram da década de 90
(11,12). Apesar de este procedimento ser pouco solicitado, pois na maioria das vezes o diagnóstico é sugerido pelos aspectos de imagem da lesão, nossa pequena experiência demonstra que é factível e bem tolerado. A hemorragia retrobulbar é a complicação mais comum, no entanto, na maioria das vezes é pequena e reabsorvida sem sequelas
(8). Não encontramos relatos na literatura de complicações mais graves, como lesões do globo ocular e nervo óptico, nos procedimentos guiados por métodos de imagem (US ou TC). Estes, quando realizados por radiologistas com experiência em procedimentos percutâneos e biópsias por agulha grossa, não oferecem riscos maiores, visto que o trajeto da agulha pode ser bem controlado pela TC. Algumas técnicas podem ser utilizadas para reduzir o risco de complicações, como utilizar agulhas de menor calibre (p. ex.: 20-
gauge) e disparos de curto alcance (1,5 cm), que também produzem diagnóstico satisfatório na grande maioria dos casos.
Em levantamento feito por Yarovoy et al.
(8), em que foram avaliadas 50 biópsias por agulha grossa de tumores de órbita utilizando agulhas de 18-
gauge e 20-
gauge (11 guiadas por US e as demais sem métodos de imagem), apenas dois pacientes apresentaram hematoma retrobulbar leve, sem comprometimento da acuidade visual, e não houve nenhum caso de lesão do globo ou nervo óptico, alteração da motilidade ocular ou infecção. Nessa casuística, o diagnóstico histopatológico foi estabelecido com sucesso em 94% dos procedimentos
(8).
Em ambos os casos apresentados no presente relato, a decisão de realizar a biópsia percutânea por agulha grossa guiada por TC foi baseada em discussão multidisciplinar com os médicos assistentes, incluindo oncologistas clínicos e cirurgiões. Optamos por realizar biópsia por agulha grossa e não PAAF, pela indisponibilidade de citopatologista na sala durante o procedimento para confirmar a presença de material suficiente para o diagnóstico e pela larga experiência profissional que a equipe de radiologia intervencionista do serviço tem neste procedimento. No caso específico em que houver suspeita de linfoma em uma lesão orbitária, a avaliação histológica é preferida para diagnóstico adequado e classificação do tumor, em razão do grande número de resultados discordantes na PAAF
(13).
Em conclusão, em nossa pequena amostra, a biópsia por agulha grossa guiada por TC foi uma alternativa segura e eficaz na coleta de material para avaliação histológica de lesões orbitárias selecionadas, em que o diagnóstico pré-operatório é importante para o adequado planejamento terapêutico. No entanto, deve-se sempre levar em consideração a relação custo-benefício do procedimento, esgotando-se todas as possibilidades de diagnóstico por métodos não invasivos antes da indicação da biópsia.
REFERÊNCIAS 1. Chojniak R, Pinto PNV, Tyng CJ, et al. Computed tomography-guided transthoracic needle biopsy of pulmonary nodules. Radiol Bras. 2011;44:315-20.
2. Chojniak R, Grigio HR, Bitencourt AGV, et al. Percutaneous computed tomography-guided core needle biopsy of soft tissue tumors: results and correlation with surgical specimen analysis. Radiol Bras. 2012;45:259-62.
3. Kapur R, Mafee MF, Lamba R, et al. Orbital schwannoma and neurofibroma: role of imaging. Neuroimaging Clin N Am. 2005;15:159-74.
4. Rawlings NG, Brownstein S, Robinson JW, et al. Orbital schwannoma: histopathologic correlation with magnetic resonance imaging. Can J Ophthalmol. 2007;42:326-8.
5. Smith AB, Rushing EJ, Smirniotopoulos JG. Pigmented lesions of the central nervous system: radiologic-pathologic correlation. Radiographics. 2009;29:1503-24.
6. Mathai AM, Naik R, Pai MR, et al. Orbital melanocytoma. Orbit. 2008;27:383-7.
7. Gupta S, Sood B, Gulati M, et al. Orbital mass lesions: US-guided fine-needle aspiration biopsy - experience in 37 patients. Radiology. 1999;213:568-72.
8. Yarovoy AA, Bulgakova ES, Shatskikh AV, et al. CORE needle biopsy of orbital tumors. Graefes Arch Clin Exp Ophthalmol. 2013;251:2057-61.
9. Chojniak R, Isberner RK, Viana LM, et al. Computed tomography guided needle biopsy: experience from 1,300 procedures. Sao Paulo Med J. 2006;124:10-4.
10. Ortiz O, Bastug D, Ellis B. CT-guided percutaneous lateral suprazygomatic approach for posterior orbital wall biopsy. Skull Base Surg. 1996;6:249-51.
11. Shields JA, Shields CL. Biopsy techniques for orbital tumors. Int Ophthalmol Clin. 1993;33:175-80.
12. Alter C, Heywang-Köbrunner SH, Beck R. Diagnosis of intraorbital meningioma. Aktuelle Radiol. 1996;6:232-4.
13. Landgren O, Porwit MacDonald A, Tani E, et al. A prospective comparison of fine-needle aspiration cytology and histopathology in the diagnosis and classification of lymphomas. Hematol J. 2004;5:69-76.
1. Mestre, Médico Titular e Responsável pelo Setor de Intervenção Percutânea do Departamento de Imagem do A.C.Camargo Cancer Center, São Paulo, SP, Brasil
2. Mestre, Fellow do Departamento de Imagem do A.C.Camargo Cancer Center, São Paulo, SP, Brasil
3. Doutor, Médico Titular do Departamento de Imagem do A.C.Camargo Cancer Center, São Paulo, SP, Brasil
4. Médica, Fellow no Serviço de Oftalmologia do Hospital do Servidor Público Estadual, São Paulo, SP, Brasil
5. Médico, Fellow do Departamento de Imagem do A.C.Camargo Cancer Center, São Paulo, SP, Brasil
6. Meste, Médica Titular e Responsável pelo Setor de Tomografia Computadorizada do Departamento de Imagem do A.C.Camargo Cancer Center, São Paulo, SP, Brasil
7. Doutor, Médico Titular e Diretor do Departamento de Imagem do A.C.Camargo Cancer Center, São Paulo, SP, Brasil
Endereço para correspondência:
Dr. Almir Galvão Vieira Bitencourt
Rua Antônio Prudente, 211, Liberdade
São Paulo, SP, Brasil, 01509-010
E-mail:
almirgvb@yahoo.com.brRecebido para publicação em 20/8/2013.
Aceito, após revisão, em 17/1/2014.
Trabalho realizado no A.C.Camargo Cancer Center, São Paulo, SP, Brasil.

 |
|