Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 5 - Sep. / Oct. of 2014
Vol. 47 nº 5 - Sep. / Oct. of 2014
|
CASE REPORT
|
|
Acute tracheobronchitis caused by Aspergillus: case report and imaging findings |
|
|
Autho(rs): Katia Hidemi Nishiyama1; Esther de Alencar Aripe Falcão2; Fernando Uliana Kay3; Gustavo Borges Silva Teles3; Fabiola Del Carlo Bernardi4; Marcelo Buarque de Gusmão Funari5 |
|
|
Keywords: Aspergillosis; Tracheal disease; Immunocompromised host. |
|
|
Abstract: INTRODUCTION
Acute tracheobronchitis caused by Aspergillus sp is a rare manifestation of the invasive form of this fungus. It is also known as pseudomembranous and ulcerative tracheobronchitis and generally occurs in severely immunocompromised patients(1,2), presenting high mortality, reported in more than 70% of cases(3). Up to the present moment, this condition has been poorly described and illustrated in the literature. The authors report a case of tracheobronchial aspergillosis in a patient presenting with febrile neutropenia after undergoing bone marrow transplant, and discuss the main computed tomography (CT) findings. CASE REPORT A 62-year-old man presenting with febrile neutropenia in association with dry cough and dyspnea, at the 16th. day after autologous bone marrow transplant for mantle cell lymphoma. Chest CT was performed to investigate the infectious focus, and demonstrated diffuse tracheobronchial thickening associated with densification of the adjacent mediastinal fat (Figure 1). 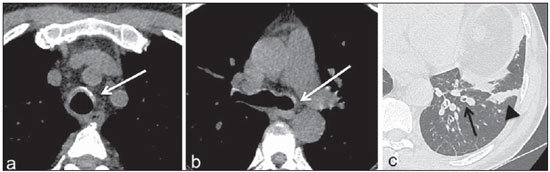 Figure 1. Non contrast-enhanced chest CT, axial sections. a: Mediastinal window - subtle tracheal thickening (arrow) associated with slight densification of the adjacent mediastinal fat. b: Mediastinal window - also, observe the presence of parietal thickening of the main bronchi, most noticeable at left (arrow). c: Lung window - bronchial wall thickening (arrow) associated with laminar atelectasis (arrowhead). The patient was already making use of empirical antibiotic therapy for the febrile condition, as well as coverage for fungal infections with amphotericin B. Follow-up CT did not demonstrate any significant alteration in the course of the condition. However, the patient reported persistence of the cough and hemoptysis. CT performed one month and ten days after demonstrated worsening of the imaging findings, with greater tracheal and bronchial walls thickening and increased densification of the adjacent mediastinal fat (Figure 2). 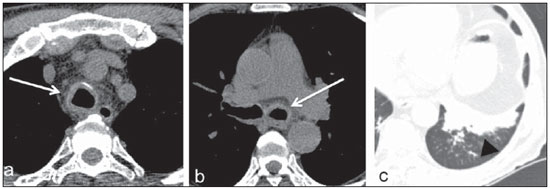 Figure 2. Non contrast-enhanced chest CT, axial sections performed one month and ten days following the first CT scan. a,b: Mediastinal wall - there was increase in the diffuse thickening of the tracheal and bronchial walls (arrows), particularly at left, and greater blurring of the adjacent mediastinal fat. c: Lung window - increase in the bronchial wall thickening and pulmonary atelectasis in the left lower lobe (arrowhead), with development of adjacent centrilobular micronodules. After three weeks, the patient was submitted to laryngotracheobronchoscopy, and attached but detachable whitish plaques with underlying friable mucosa were found on the walls of the trachea and bronchial three. Some of these plaques determined segmental ostial obstruction. Bronchoalveolar lavage was collected in the left lower lobe and endobronchial biopsy was performed. The biopsy revealed the presence of bifurcated hyphae at 45°, stained by the histochemical Grocott method, with characteristics of Aspergillus sp (Figures 3a and 3b), and chest CT performed two days after the laryngotracheobronchoscopy demonstrated progression of the disease (Figure 3c). The bronchoalveolar lavage culture was positive for Aspergillus sp. 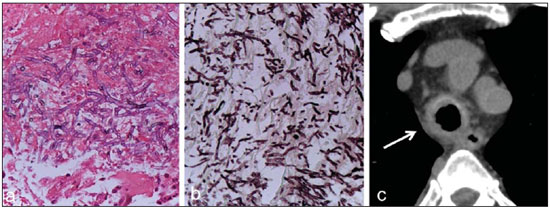 Figure 3. Anatomopathological analysis and chest CT, four weeks after the first CT scan. a,b: Fungal structures with bifurcation at 45°. b: Fungi-specific Grocott staining. c: Non contrast-enhanced chest CT, axial section, four weeks after the first CT scan reveals disease progression with increased tracheobronchial thickening (arrow), as well as increased densification of the mediastinal fat. Considering his clinical stability, the patient was discharged and remained under follow-up on an outpatient basis at the day-hospital, and was prescribed other antifungal drug (oral voriconazol) to increase the antifungal coverage. Two days after, the patient required a new admission for abdominal pain, diarrhea, hypotension and febrile peak, with diagnosis of septic shock from abdominal origin, remaining in the intensive care unit. Despite the clinical support, the patient died in three days. DISCUSSION The spectrum of the involvement of the bronchial three and pulmonary parenchyma by the Aspergillus sp is variable according to the patient's immunity and preexistence of pulmonary disease. It is a potentially lethal, common opportunistic infection that may present in the following forms: bronchopulmonary allergic, saprophytic (aspergilloma), angioinvasive, and chronic necrotizing, besides the tracheobronchial form (invasive of the airways). The latter is an uncommon manifestation of the disease predominantly limited to the airways, generally occurring in severely immunocompromised patients or in those affected by AIDS(1,2,4). Other relevant risk factors described in the literature include lung transplant and corticotherapy(5). The clinical presentation is variable and nonspecific, which masks and delays the diagnosis. Cough, fever and dyspnea are the most frequent symptoms, and hemoptysis is reported in 11.5% to 26.3% of cases(5,6). Recently, the use of serial sampling of galactomannan polysaccharides has been proposed for the diagnosis of invasive pulmonary aspergillosis. However, despite the high specificity of this method (85% to 99%), some studies have demonstrated sensitivity ranging between 29% and 94%(7). In such cases, the typical tomographic findings seem to precede the laboratory tests findings of invasive pulmonary aspergillosis (increased in serum galactomannan levels inclusive) in neutropenic patients(7). At bronchoscopy, tracheobronchial aspergillosis may present either as a diffuse or focal ulcerative form, or even as elevated whitish plaques associated with inflammatory lesions and pseudomembranes(1,2), historically classified into three presentation forms according to such findings, as follows: pseudomembranous, ulcerative, and obstructive(4,5). However, currently some authors propose that such presentations might represent different stages of a single disease and not distinctive entities. A new classification was proposed as follows: type I - superficial infiltrate; type II - deeper involvement, affecting the cartilage and with airways destruction; type III - obstructive (airway occlusion > 50% by pseudomembranes, polypoid granulation tissue or necrotic tissue); type IV - mixed form (coexistence of two or more forms of disease)(6). Type II seems to be more closely related to greater aggressiveness and worse prognosis(6). As regards imaging findings, the literature describes tracheal or bronchial wall thickening as the main finding(1,2). Presence of multifocal, irregular plaques on the tracheal wall, many times with high attenuation due to the Aspergillus sp capacity to fix calcium, is also described(7,8). According to Fernández-Ruiz et al.(5), specific signs are found in just 25% of cases: smooth or nodular tracheobronchial thickening - 14.3%; atelectasis - 8.2%; endobronchial mass - 2.1%. In the present case, besides tracheobronchial thickening, the authors have also observed densification of adjacent mediastinal fat, a finding that might be related to infiltration of adjacent tissue planes. Transbronchial biopsy in association with sample culture presents high diagnostic accuracy, but many times it is contraindicated by the presence of thrombocytopenia or coagulopathy observed in patients affected by malignant hematological diseases. There is no specific recommendation for the management of tracheobronchial aspergillosis. The use of voriconazol has been reported in the literature as the drug of choice, despite the disadvantage of its high cost. Thus, other anti-fungal drugs, either alone or in combination have also been quite utilized in the clinical practice(5). In the study developed by Fernández-Ruiz et al.(5), the tracheobronchial aspergillosis seems to be relatively more benign than other invasive forms of the disease, and neutropenia and acute respiratory failure as initial presentation of the disease constitute the main predictors of mortality. Despite the rarity of this disease, the authors highlight the relevance of the knowledge of acute tracheobronchitis caused by Aspergillus sp, considering that it affects severely immunocompromised patients with high mortality indices, and whose prognosis depends on early appropriate management. In the present case report, the authors emphasized the CT findings which are poorly described and illustrated in the literature and many times may be decisive for the diagnosis of this entity, particularly in patients with contraindication for bronchoscopy with biopsy that is still considered as a diagnostic reference standard. Acknowledgements The authors thank Drs. Hamilton Choji, Danilo Perussi Bianco and Ricardo mazzetti Guerrini, for their support during the preparation of this manuscript. REFERENCES 1. Kang EY. Large airway diseases. J Thorac Imaging. 2011;26:249-62. 2. Franquet T, Müller NL, Oikonomou A, et al. Aspergillus infection of the airways: computed tomography and pathologic findings. J Comput Assist Tomogr. 2004;28:10-6. 3. Krenke R, Grabczak EM. Tracheobronchial manifestations of Aspergillus infections. ScientificWorldJournal. 2011;11:2310-29. 4. McGuinness G, Gruden JF, Bhalla M, et al. AIDS-related airway disease. AJR Am J Roentgenol. 1997;168:67-77. 5. Fernández-Ruiz M, Silva JT, San-Juan R, et al. Aspergillus tracheobronchitis: report of 8 cases and review of the literature. Medicine (Baltimore). 2012;91:261-73. 6. Wu N, Huang Y, Li Q, et al. Isolated invasive Aspergillus tracheobronchitis: a clinical study of 19 cases. Clin Microbiol Infect. 2010;16:689-95. 7. Weisser M, Rausch C, Droll A, et al. Galactomannan does not precede major signs on a pulmonary computerized tomographic scan suggestive of invasive aspergillosis in patients with hematological malignancies. Clin Infect Dis. 2005;41:1143-9. 8. Gotway MB, Dawn SK, Caoili EM, et al. The radiologic spectrum of pulmonary Aspergillus infections. J Comput Assist Tomogr. 2002;26:159-73. 1. MD, Researcher, Radiology Department - Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil 2. MD, Resident, Radiology Department - Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil 3. MDs, Physician Assistants, Radiology Department - Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil 4. PhD, Physicians Assistant, Department of Pathology - Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil 5. PhD, MD, Radiologist, Head of Unit of Thoracic Radiology, Radiology Department - Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil Mailing Address: Dra. Katia Hidemi Nishiyama Rua Tamandaré, 776, ap.132, Liberdade São Paulo, SP, Brazil, 01525-000 E-mail: katianishiyama@yahoo.com.br Received July 3, 2013. Accepted after revision October 22, 2013. Study developed at Radiology Department - Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554