Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 3 - May / June of 2014
Vol. 47 nº 3 - May / June of 2014
|
ORIGINAL ARTICLE
|
|
The learning of resources of the unified health system in the radiology residency program |
|
|
Autho(rs): Aparecido Ferreira de Oliveira1; Henrique Manoel Lederman2; Nildo Alves Batista2 |
|
|
Keywords: Medical education; Medical residency; Unified health system; Private health institutions; Radiology; Imaging diagnosis. |
|
|
Abstract: INTRODUCTION
The National Curricular Guidelines (DCN)(1) for education in medicine advocate the development of general competencies, including decision making, communication and administration of work force, physical, material and information resources. According to Chiesa et al.(2), "DCN reiterate the need and the duty of Higher Education Institutions (IES) to educate health professionals with a focus on the Unified Health System (SUS) with the purpose of adjusting the education to meet the health needs of the Brazilian population". For those authors, "curricula focused on the development of competencies required to work in health within SUS must provide pedagogical opportunities to ensure that students apply the theoretical knowledge and develop not only technical skills, but also political and relational skills." Guimarães(3) reinforces the relevance of the education for the public sector: "Despite the SUS policies towards integral attention to users, many of the professionals currently acting within the system do not have this basic training, i.e., educating professionals capable of working in interdisciplinary environments and to meet the demands of the Brazilian health system, according to its principles and guidelines...". At the public health services, one of the challenges is the efficient utilization of scarce resources, many times connected with political decisions and projects, legal and regulatory restrictions and impositions, which may lead to delays and squandering, impairing the decision making on the effective utilization of human, financial and technological resources by the managers. Frequently, after completing the medical residency, the radiologist continues to work at public hospitals which maintain most of the programs recognized by the National Medical Residency Committee, in environments connected with the Brazilian Unified Health System (SUS), whose regulations establish their funding and operationalization. According to Natalini(4), "SUS is a system that comprises institutions at the three governmental levels (Federal, State and Municipal), and is supplemented by the private sector under contracts or agreements. The private sector, as contracted by SUS, operates under the same standards that apply to the public sector." Silva et al.(5) have commented on the interfaces established between the private and the public sectors in Portugal: "It is a fact that the State, upon establishing contracts or agreements with the private sector and upon reducing the investments in the public sector, starts "purchasing" health services from private suppliers, which implies the creation of new private health service units and service providers." Valença et al.(6) have comment that with a view on the social demands for more comprehensive and complex services in a context of scarce financial resources and lacking managers with a deep knowledge on SUS, it is necessary to include such learning in residency programs, being important for the resident to learn that "...SUS is one of the social responses to health problems and needs of the Brazilian population, acknowledging that in addition to SUS itself, economic, social and environmental policies are essential for the promotion of health and for the reduction of risks and harm." Almeida(7) comments that "good management practices (...) are important not only for the proper development of academic and administrative activities, but also and especially to achieve success in the initiatives towards change in the education of physicians and other health professionals. Such experiences, their challenges and dilemmas have led to studies on the intersection of the administrative areas and medical education." Boechat et al.(8), specifically referring to radiologists' education, comment that "The medical resident, at the end of his training, must be capable of critically utilizing all resources that will allow him to improve his skills along his professional life." With a view on this scenario, one should ask: How does the program of medical residency in radiology at Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp) prepare the residents in relation to the management of SUS resources required for the radiological practice? What are the positive points and limits for such learning? The present study was aimed at investigating, among residents, faculty and radiology preceptors, the learning on the management of SUS resources in medical residency in radiology at EPM-Unifesp, with the purpose of identifying opportunities for improvements in the education of radiologists. MATERIALS AND METHODS The analyzed program occurs at a public hospital over a three-year period, for 12 students in the first year (R1), 12 in the second year (R-2), and 12 in the third year (R-3), with a supervising teacher, a teaching and research coordinator, two chief preceptors and 11 sector preceptors, distributed among abdomen, head and neck, musculoskeletal system, breast, fetal medicine, emergency, interventional radiology and neurology. Also, the entire staff of the department, comprising faculty, five collaborating physicians, administrative education technicians and the participants of the professional updating program participate in the residents' education. The authors have opted for an exploratory investigation, with quantitative and qualitative approach, carried out with the residents, preceptors and faculty staff acting in the program during 2011. The study population comprised five members of the faculty staff (55.5% of the category), 14 preceptors and 27 residents (10 R1, seven R2 and ten R3). The project was approved by the Committee for Ethics in Research of Unifesp. The present study became a part of a Master dissertation presented and approved at Unifesp. At the first phase of data collection, 46 individuals (75.4% of the 61 comprising the study population) responded to a Likert attitudinal scale comprising 11 items, two of them related to the theme of the present study. Such a scale is an instrument aimed at objectively evaluating the intensity of opinions and attitudes, by measuring the degree of acceptance or rejection towards a determined statement, which led the authors to its choice(9). Amaro et al.(10) have commented that the scale presents a series of five propositions of which the respondent should select one, namely, totally agree, agree, no opinion on the subject, disagree, totally disagree - as regards statements related to the investigated object. The obtained data were tabulated and translated into charts, indicating agreement or disagreement trends of the respondents in relation to the proposed themes, representing an initial approach to the object under study, which is the base for further data collection carried out by means of semi-structured interviews. In this phase, interviews with a seven-question script, lasting approximately 10 minutes, were carried out with a number of participants as per the criteria of a qualitative investigation, i.e., relevance and recurrence of data and data saturation. This occurred after the 18th interview. After a full transcript, the data were submitted to a thematic analysis (meaning units), one of the techniques for analysis of contents, as recommended by Minayo(11): data ordination after reading the obtained material, identification and establishment of context units (of which the data was a part), identification of the recording units (word, phrase or sentence) regarding the analyzed object and grouping of such units into analysis categories. RESULTS When challenged with the proposition "In radiology, the resident has the opportunity of learning on the management of resources of the Unified Health System - SUS" most respondents disagreed with the proposition (only 24% of agreement) (Figure 1). 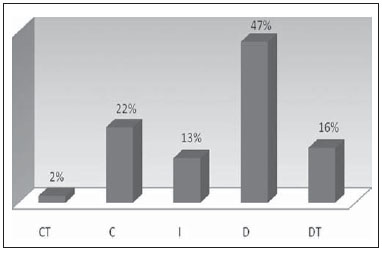 Figure 1. Rate of agreement/disagreement about the opportunity to learning about the management of the resources from the Brazilian Unified Health System (SUS). In the phase of deepening interviews, the respondents reinforced such a disagreement. The thematic analysis revealed three categories, as follows: the lack of emphasis on subjects related to management of resources from SUS; the lack of time for such supplementary learning and non existence of theoretical support related to the theme: "we do not have the opportunity to learn about such management of resources from SUS" - E03; "this again reflects the short time we have to provide a more complete education to our residents" - E18; "we do not learn anything about it, on actually managing the resources, we do not have a theoretical knowledge on this subject" - E11. The comprehensiveness, complexity and depth of the theme are also highlighted as limitations for such learning: "most do not have the opportunity of learning, SUS is a very complex system" - E14; "the resident in radiology is basically in contact with SUS on his daily activities, then what he sees is how the flow of the patient is and the difficulty in scheduling an exam; however the knowledge on resources management is something deeper, and I do not think the resident ever really gets to know it" - E13. It is interesting to observe that for one of the respondents, in spite of being aware of the non existence of such an opportunity ("at no time during residency we have any contact with this type of guidance") such teaching should be done at a different phase of medical education ("this is a subject for the graduation course. It is no subject for medical residency" - E-07). When exposed to the second question, seeking to learn on the opportunities for learning on management of resources for the practice of radiology in the interfaces of school hospitals with private institutions, most of the faculty, preceptors and residents (76%) also answered that it does not occur during residency (Figure 2). 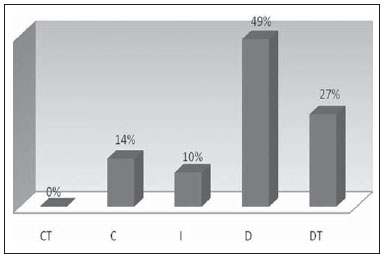 Figure 2. Rate of agreement/disagreement about the opportunity to learn about the management of the resources at private institutions in the interface with the Unified Health System (SUS). The respondents reinforced that only eventually such a learning might occur, but by means of activities parallel to the program (with friends or family members), in congresses or by means of contacts with private managers: "only by acquaintances and friendship with people belonging to them (private institutions) and by means of comments in journeys and congresses" - E08. Another learning possibility may occur by means of the work done by such institutions during residency: "a good portion of the residents work at such private institutions, but nobody explains on how it is managed" - E06; "there is eventually the opportunity of acting at the private service in the last year of residency" - E01. According to most respondents, the main limitations for such learning during residency are seen at the very specificities of a program inserted into a public service: "during residency, we really do not have contact with private institutions; I think that actually, no contact at all during residency" - E12; "we do not have a way to learn about the management, really I do not have any knowledge on that"- E10. DISCUSSION Despite the complexity and comprehensiveness of SUS, it became clear that the residents, preceptors and faculty recognize the absence of discussions on this subject in the programs, as an important component in the residents' education. Several reasons seem to explain such an absence in the contents of the programs. The respondents reinforce the findings of the questionnaire, disagreeing that SUS should be taught even at its most basic features; their sole experience is the daily routine with an excessive number of patients with a full agenda, and many times with an inappropriate infrastructure. Chiesa et al.(2), reflecting on the education of the health professionals, point out that "In order to face the challenges posed by the world of work, such paradigm change involving the concepts of health and education must be experienced during education, widening the possibilities of horizontalization and democratization of the knowledge." Lima(12) adds that all education should consider a new professional profile, as those already listed at the DCNs, with a view on the actual conditions of the labor market: "In Brazil, new demands regarding health professional education are reflected in the National Curricular Guidelines of the Graduation Courses for various careers, including Medicine, and propose a new professional profile based on the development and on the competence of those professionals graduated at such programs." Moimaz et al.(13), discussing on the relevance of professional education oriented towards health needs, comment that "the vertiginous transformations in the field of healthcare make the training of human resources a real challenge." The SUS is the main investor and driver of education and professional training, as well as of investment and costing of premises, equipment and processes of hospital services provision. In that sense, Motta et al.(14) highlight: "Since the early origins of the Unified Health System (SUS) one envisioned the difficulties for the construction of a new healthcare model. Among them, the issues respecting human resources and, in particular, the development component with clear demands for qualification and requalification of the workforce." For Bouyer et al.(15), "...a good education should offer a theorization which allows conceptual acquisition and the perception of the real difficulties of implementation of own theory itself in practical situations." The programs of medical residency in radiology must commit with the education on SUS and its relationship with the private sector promoting the discussion about its relevance in the radiology routines. This becomes even more relevant with the introduction of the public-private partnerships, which, in the health sector, has widened the current concept at Social Organizations (OSs - Law No. 9637/98) and Civil Organizations of Public Interest (OSCIPs - Law No. 9790/99 and Decree 3100/99) which function under the fundamentals of concessions, in an attempt to improve health services for the population(16). Residency faces the huge challenge in the education of professionals focused both on the demands and contexts of public health as well as complementary health. The authors consider it important that residents understand the relevance and the impact of SUS on public health in Brazil and how the processes of resources obtainment, distribution and application develop. CONCLUSIONS The present investigation has demonstrated that most of the respondents do not agree that there are opportunities to learn about the management of SUS's resources for the practice of radiology, attributing this fact to the lack of structure, time and theoretical support of the residency program. The comprehensiveness, depth and complexity of SUS are pointed out as limitations for the better learning on the management of such resources. The non existence of opportunities for learning about the management of private resources was also pointed out by 76% of the respondents, and such learning only occurs by means of parallel activities (friends or family bonds), congresses and journeys, working at such services, or eventually training in the last year of residency. The medical residency programs must teach on how the resources originated from SUS are obtained and utilized in investments and costing of activities in the medical specialties. In the practice of radiology and imaging diagnosis, such factors take on relevant dimensions. In this context, at medical residency programs in radiology, where the physicians acquire competence for their practice, it is expected that the resident to further develop competences to act in the context of the specialty both at public and private sector, assimilating peculiarities and overcoming the normally faced difficulties. The authors understand that lectures, case reports and debates on relevant features of SUS and its impact on the daily practice of radiology, followed by the inclusion of elective disciplines, would minimize the limitations, leading to increased interest and understanding on the relevance of the System. Such aspects deserve and need to be further discussed in debates and in further investigations, widening the discussion and development of alternatives for a better education of radiologists in Brazil. REFERENCES 1. Brasil. Ministério da Educação. Conselho Nacional de Educação. Câmara de Educação Superior. Resolução CNE/CES nº 4, de 7 de novembro de 2001. Institui Diretrizes Curriculares Nacionais do Curso de Graduação em Medicina. [acessado em 11 de dezembro de 2012]. Disponível em: http://portal.mec.gov.br/cne/arquivos/pdf/CES04.pdf. 2. Chiesa AM, Nascimento DDG, Braccialli LAD, et al. A formação de profissionais da saúde: aprendizagem significativa à luz da promoção da saúde. Cogitare Enferm. 2007;12:236-40. 3. Guimarães TG. Papel do preceptor na residência multiprofissional: experiência da nutrição. Porto Alegre: Universidade Federal do Rio Grande do Sul; 2010. [acessado em 13 de dezembro de 2011]. Disponível em: http://hdl.handle.net/10183/32964. 4. Natalini G. Princípios básicos do SUS. In: SUS - O que você precisa saber sobre o Sistema Único de Saúde. São Paulo: Associação Paulista de Medicina; 2001. 5. Silva CRRG, Rodrigues VMCP. O que dizem os pacientes dos serviços privados de radiologia, Portugal. Saúde Soc. São Paulo. 2011;20:425-35. 6. Valença CN, Germano RM. O que é SUS [Resenha]. Cad Saúde Pública. 2010;26:1262-3. 7. Almeida MJ. Gestão da escola médica: crítica e autocrítica. Rev Bras Educ Med. 2008;32:202-9. 8. Boéchat AL, Sousa EG, Moreira FA, et al. Proposta de um programa básico para a formação do médico residente em radiologia e diagnóstico por imagem. Radiol Bras. 2007;40:33-7. 9. Chizzott A. Pesquisa em ciências humanas e sociais. São Paulo: Cortez Editora; 2008. 10. Amaro A, Póvoa A, Macedo LA. A arte de fazer questionários. Porto, Portugal: Faculdade de Ciência da Universidade do Porto; 2004/2005. [acessado em 14 de abril de 2010]. Disponível em: http://nautilus.fis.uc.pt/cec/esjf/wp-content/uploads/2009/11/elab_quest_quimica_up.pdf. 11. Minayo MCS. O desafio do conhecimento. Pesquisa qualitativa em saúde. São Paulo: Hucitec; 1999. 12. Lima VV. Competência: distintas abordagens e implicações na formação de profissionais de saúde. Interface - Comunic Saúde Educ. 2005;9:369-79. 13. Moimaz SAS. Saliba NA, Zina LG, et al. Práticas de ensino-aprendizagem com base em cenários reais. Interface - Comunic Saúde Educ. 2010;14:69-79. 14. Motta JIJ, Buss P, Nunes TCM. Novos desafios educacionais para a formação de recursos humanos em saúde. [acessado em 7 de maio de 2014]. Disponível em: http://www.ccs.uel.br/olhomagico/v8n3/enfoque.htm. 15. Bouyer GC, Sznelwar L, Costa MJB. Aprendizagem estratégica e aquisição conceitual no ensino de gestão de operações. In: XXV Encontro Nacional de Engenharia de Produção. Porto Alegre, RS, Brasil, 29 outubro a 1º novembro de 2005. [acessado em 18 de abril de 2010]. Disponível em: http://www.abepro.org.br/biblioteca/ENEGEP2005_Enegep1101_1587.pdf. 16. Ferreira AS. As organizações sociais e as organizações da sociedade civil de interesse público: considerações sobre seu regime jurídico. [acessado em 10 de maio de 2013]. Disponível em: http://www.gespublica.gov.br/projetos-acoes/pasta.2009-07-15.5584002076/copy_of_pasta.2010-10-22.6887744790/OS%20E%20OSCIP%20-%20SERGIO%20ANDREA.pdf. 1. Master, Fellow PhD degree, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil 2. Docents, Full Professors, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil Mailing Address: Aparecido Ferreira de Oliveira Centro de Desenvolvimento do Ensino Superior em Saúde - Universidade Federal de São Paulo (Cedess-Unifesp) Rua Pedro de Toledo, 859, Vila Clementino São Paulo, SP, Brazil, 04039-032 E-mail: aparecidoliveira@ig.com.br Received January 24, 2013. Accepted after revision December 11, 2013. Study developed at Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554