Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 47 nº 3 - May / June of 2014
Vol. 47 nº 3 - May / June of 2014
|
ORIGINAL ARTICLE
|
|
Current situation of high-dose-rate brachytherapy for cervical cancer in Brazil |
|
|
Autho(rs): Rogério Matias Vidal da Silva1; Juliana Castro Dourado Pinezi2; Luiz Eduardo Andrade Macedo3; Divanízia do Nascimento Souza4 |
|
|
Keywords: Brachytherapy; Cancer; Cervix; Uterus; Research; Brazil. |
|
|
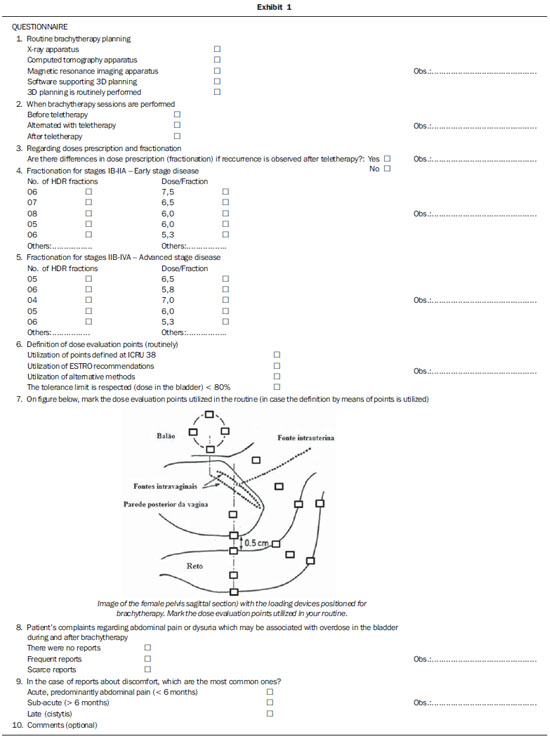
Abstract: INTRODUCTION
High-dose-rate (HDR) afterloading brachytherapy has been utilized in the treatment of uterine cervix cancer since the decade of 1960, but it was introduced in Brazil in the 1990s(1,2). This type of therapy has undergone significant evolution in terms of treatment methods and planning systems(3-6). Currently, the utilization of loading devices compatible with imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) allow for the acquisition of three-dimensional images of the entire pelvis with the loaders duly positioned for treatment. Such images associated with modern planning softwares allow for outlining the target volume and evaluating the radiation dose behavior on healthy structures with a high degree of fidelity, thus allowing for the optimization of the points and dwell time of the source(6). Studies developed by Wang et al.(6) and Zwahlen et al.(7) have related the plannings developed with basis on CT and MRI, respectively, with the two-dimensional plannings based on conventional radiographic images, demonstrating better tumor coverage and lower toxicity on healthy tissues as such modern imaging techniques are utilized for the planning. Considering such developments, the present study presents the results of a research developed with hospitals and clinics in Brazil in order to obtain data on the current situation of uterine cervix brachytherapy in the country. Data on the number of apparatuses and their distribution throughout the country were obtained. The present study also describes the methods utilized by the Brazilian radiotherapists to prescribe and evaluate brachytherapy doses in their clinical routines. Preliminarily, post-treatment complications that may be related to overdoses to the bladder were also investigated. MATERIALS AND METHODS In March 2012, 220 hospitals which operate radiotherapy services were identified at the website of Comissão Nacional de Energia Nuclear (National Commission of Nuclear Energy). Such institutions were contacted by phone in order to confirm the existence of active HDR brachytherapy equipment in their premises. Of the contacted institutions, 89 hospitals and clinics confirmed the existence of HDR brachytherapy facilities. Presentation letters with a questionnaire (Exhibit 1) addressed to the radiotherapists of the institution were mailed. In the first part of the questionnaire, the respondents answered questions on the planning routine and on the characteristics of imaging and therapy apparatuses available at their institutions. On the second part, the questionnaire was focused on data about the moment of treatment when the brachytherapy sessions are performed and on whether there are differences in the prescription in cases where the lesion persists after teletherapy, in addition to adopted fractionation schedule types. The third part of the questionnaire approached questions on the methods to evaluate the dose to risk organs. In this part, a figure similar to that included in the ICRU-38 was presented, representing a lateral view of the whole pelvis at a session of intracavitary brachytherapy for cervical cancer(4). Several checkboxes were inserted into such a figure, some of them in locations defined by the ICRU-38 and others at random spots, in order for the respondents to identify at which points they routinely evaluate the radiation dose delivered by HDR brachytherapy. Considering that investigating the occurrence of all possible side effects resulting from this type of treatment would considerably increase the number of propositions, the fourth and last part of the questionnaire was restricted to the implications of HDR brachytherapy effects on the urinary tract, more specifically, on the bladder. Such an organ was also selected on account of its reference point dose apparently having little relevance in the estimation of the actual dose absorbed by this organ during this type of brachytherapy(8-10). In this questionnaire part, a blank space was left for the professionals to freely express their suggestions, criticism and opinions on aspects related to the questionnaire. RESULTS Out of the 89 radiotherapy services which confirmed the existence of HDR brachytherapy equipment in operation, 61 sent back filled-out questionnaires, corresponding to a total of 68% of the brachytherapy services. Figure 1 presents a comparative chart of the number of institutions equipped with HDR brachytherapy in the five geographic regions of the country in the years 2001 and 2013, with basis on the comparison of data obtained by the present investigation and those reported by Esteves et al.(3) in 2001. 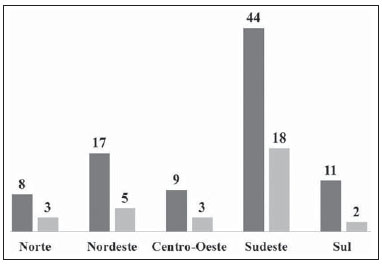 Figure 1. Number of HDR brachytherapy apparatuses by region in 2013 and 2001. Number of apparatuses in 2013 (dark gray columns) and number of apparatuses in 2001 (light gray columns). On Figure 2 one can observe the ratio between estimates of new cases of uterine cervix cancer and the number of available HDR brachytherapy apparatuses per region in 2013, considering the national estimates provided by Instituto Nacional de Câncer(11). 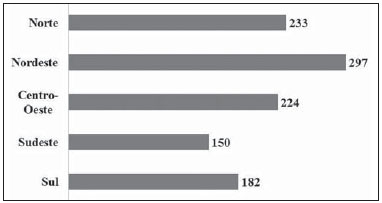 Figure 2. Ratio between estimates of new uterine cervical cancer cases and number of HDR brachytherapy apparatuses by region in 2013. By comparing the number of apparatuses installed in 2001 (31) and in 2013 (89), a global increase of approximately 300% is observed. All the regions presented a significant increase in the number of services; however the Southern region had the highest increase with 550%. The Southeastern region has the highest number of apparatuses, while it also presents with the highest estimates of new uterine cervix cancer cases. The percent distribution of operational apparatuses in the Brazilian regions in 2013 is shown on Figure 3. 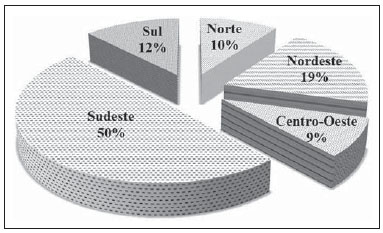 Figure 3. Percentage distribution of HDR apparatuses in operation by Brazilian regions in 2013. The Southeastern region concentrates one half of all HDR brachytherapy apparatuses in the country, followed by the Northeastern region with 19%. The Midwestern region with has the lower number of apparatuses, with only 9% of the total number of apparatuses in the country. The authors observed that 91% of the centers are equipped with three-dimensional planning softwares; however, conventional radiography was mentioned by 92% of the respondents as the main imaging tool after insertion of the loading device in their routines, while 23% informed that CT was sporadically utilized for the planning, and only 8% informed that exclusively CT was utilized. None of the respondents reported the utilization of MRI in the HDR brachytherapy planning routine. The present investigation showed that in approximately 35% of the institutions brachytherapy is performed only after teletherapy is concluded. Most institutions opt for four sessions, with doses ranging between 6.5 and 7.5 Gy per fraction. Table 1 presents the percentages of institutions according to fractionation schedule and doses per session in the routine. 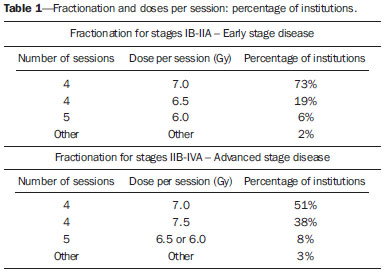 As the respondents were asked about which points or methods are utilized to prescribe and evaluate the planning in the routine, 75% of them indicated the utilization of only the points defined by the ICRU-38, while 22% indicated the utilization of alternative methods such as other points on the vesical probe surface to estimate the dose delivered to the bladder. The professionals were asked to mark the points which they use to evaluate the dose during planning on a figure of a sagittal section of the pelvis identical to the one included in the ICRU-38. The utilization of such an image after the question related to the methods habitually utilized for monitoring was intentional, with the purpose of identifying falsepositives in the answer to the previous question. Even when informing that they utilized the points recommended by the ICRU-38, 6% of the respondents marked points different from those recommended by such a document. The highest number of mistakes in the identification of such points were related to the point of the rectum. The dose evaluation point in the sigmoid colon, also proposed by the ICRU-38, was not represented on the figure; but 65% of the respondents pointed it out graphically. When asked whether they hear reports of abdominal pain which might be associated with overdoses to the bladder, 32% of the respondents answered that patient complains regarding some type of discomfort are frequent, while 61% responded that they rarely hear some type of report and 7%, that they never heard any reports. As regards the most frequent complaints, 86% of the respondents informed that those were related to acute side effects of the therapy, which are predominantly abdominal pain during the first six months after the treatment. Other respondents (14%) pointed out late effects, such as occurrence of cystitis. DISCUSSION Equipment distribution Without considering the differences in the assistance at public and private services, and the utilization of brachytherapy equipment for treating other types of cancer, the Southeastern region generally presents the lowest number of new cases per installed apparatus (150 new cases per HDR brachytherapy apparatus). On the other hand, the Northeastern region, in spite of having experienced an increase of 340% in the number of apparatuses, presents the highest number of new cases per installed HDR brachytherapy apparatus (297). Currently, in the Northern region, the States of Roraima and Amapá do not have any HDR brachytherapy service, although those states present estimated 120 new cases of cervical cancer for 2013. Characteristics of the planning routine in Brazil In the literature, MRI has been described as one of the most appropriate techniques for staging patients with cervical cancer(12). Such a method is also described as being the best tool for the acquisition of images during the routine three-dimensional planning, overcoming conventional radiography and the images obtained by means of CT(12-15). On the other hand, a recent study developed by Viswanathan et al.(16), involving institutions in Asia, North America, Europe and Oceania, demonstrated that obtaining CT images after the insertion of the loading device is the most common approach. An important characteristic in this type of planning that also must be observed is that the systematic description of the disease extent, i.e., the follow-up of changes in the gross tumor volume as the treatment progresses, particularly after teletherapy, requires time for planning and costs associated with images acquisition. The fact that a high number of institutions have softwares for three-dimensional plannings while only a small part of them actually utilize such softwares can be justified by the inappropriateness of the values paid by Sistema Único de Saúde. Specifically, one observes that the cost associated with CT and MRI required for such procedures are not covered by the regulations from the Health Ministry about procedures and values associated with radiotherapy(17,18). Several studies demonstrate that extending the total treatment time may negatively influence the local management and the patient survival(19-21). In Brazil, most interviewed institutions alternate HDR brachytherapy sessions with teletherapy sessions. However, as reported by some radiotherapists, a high number of radiotherapy services in the country are not equipped with brachytherapy apparatuses, a fact that leads to many patients being referred to other institutions in order to complete their treatment, which in some situations increases the treatment time. In spite of the lack of consensus about fractionation schedules and doses per session that should be utilized for a given clinical staging, generally the relative doses prescribed for teletherapy and brachytherapy must depend upon the initial volume of the disease, the geometric variations of the bladder and rectum, the degree of tumor regression during pelvic irradiation and also upon the therapeutic protocol followed by the institution(16,22-24). As regards fractionation and doses per session practiced by the investigated institutions, few differences were identified among them. A small number of institutions reported that it was possible to change the number of sessions and doses per session in particular situations, according to the disease extent and response to radiation. In the Brazilian context, such a small variation regarding the number of HDR brachytherapy sessions performed by the institutions may be directly associated with the guidelines imposed by Sistema Único de Saúde, which only supports the cost of four sessions for the hospital institution, regardless of the clinical staging of the patient(17,18). Dose monitoring points In HDR brachytherapy, special attention must be placed on the definition of dose monitoring points in the bladder and in the rectum, as proposed by ICRU-38. The originally defined dose evaluation point in the bladder has demonstrated to be of little representativeness(8-10). With the purpose of improving the estimation of the dose received by this organ, another point located 1.5 cm above the current one has recently been suggested as being most appropriate for the monitoring(23). As regards the point in the rectum, the literature also reports moderate representativeness for evaluating the dose received by this organ during a HDR brachytherapy session. In the present study, 98% (59) of the respondents utilize the points recommended by ICRU-38, while only 3% (2) informed that they utilize the doses in volume recommended by the GEC-ESTRO guidelines for cervical cancer brachytherapy(25). Observation of side effects possibly related to the Brazilian clinical practice During the treatment of uterine cervical cancer, the region of the lower abdomen is weakened due to factors such as the previous extent of the disease, the injury caused by radiation itself, besides the trauma caused by the insertion of loading devices and probes for brachytherapy. Considering the wide range of factors leading to temporary fragility in this region of the body, relating the causes with injuries caused by inappropriate insertions and unsuccessful plannings associated with the clinical practice would be a complex task. However, relying on the clinical experience of the respondents, the authors have preliminarily sought to investigate the efficiency of the performed brachytherapy. In spite of some studies pointing towards the lack of representativeness of the dose monitoring point in the bladder proposed by ICRU-38, in the present study most of the respondents informed that patients reports about abdominal pain which might be associated with overdose to this organ were scarce or non-existent. CONCLUSIONS The present study confirms that over the past decade there was a significant increase in the number and distribution of services offering HDR brachytherapy for uterine cervical cancer in Brazil. The Southeastern region is still ahead of the other regions as regards number of services in operation. Despite the prevalent use of CT for planning of HDR afterloading brachytherapy in several countries, in Brazil the HDR brachytherapy planning in most centers is done by means of orthogonal radiography utilizing the traditional points recommended by ICRU-38 for the definition of dose prescriptions and limits for organs at risk. The authors observed that there are still difficulties for routine access to adjuvant imaging tools such as CT and MRI, which makes routine three-dimensional planning unfeasible. As regards the usual fractionation and doses per session, little differences were observed among the Brazilian regions, with the schedule of four 7 Gy insertions being most frequently utilized. Despite some studies reporting lack of representativeness of the dose monitoring point in the bladder as proposed by ICRU-38, most of the respondents informed that patients reports about abdominal pain which might be associated with overdose to this organ were scarce or non-existent. The performance of HDR brachytherapy only after teletherapy is completed and the practice of referring the patients to undergo the procedure in other institutions, as reported by some of the respondents, may induce an increase in uterine cervical cancer recurrence and decrease in patients' survival. Acknowledgements To Medical Physicist Homero Lavieri Martins, for all suggestions and guidance for the present study, and to Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes) and Fundação de Apoio à Pesquisa e Inovação Tecnológica do Estado de Sergipe (Fapitec-SE), for the financial support. REFERENCES 1. Fu KK, Philips TL. High-dose-rate versus low-dose-rate intracavitary brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 1990;19:791-6. 2. Ferrigno R, Nishimoto IN, Novaes PE, et al. Comparison of low and high dose rate brachytherapy in the treatment of uterine cervix cancer. Retrospective analysis of two sequential series. Int J Radiat Oncol Biol Phys. 2005;62:1108-16. 3. Esteves SCB, Oliveira ACZ, Feijó LFA. Braquiterapia de alta taxa de dose no Brasil. Radiol Bras. 2004;37:337-41. 4. International Commission on Radiation Units and Measurements. Dose and volume specification for reporting intracavitary therapy in gynecology (Report 38). Bethesda, MD: ICRU; 1985. 5. Fellner C, Pötter R, Knocke TH, et al. Comparison of radiography- and computed tomography-based treatment planning in cervix cancer in brachytherapy with specific attention to some quality assurance aspects. Radiother Oncol. 2001;58:53-62. 6. Wang B, Kwon A, Zhu Y, et al. Image-guided intracavitary high-dose-rate brachytherapy for cervix cancer: a single institutional experience with three-dimensional CT-based planning. Brachytherapy. 2009;8:240-7. 7. Zwahlen D, Jezioranski J, Chan P, et al. Magnetic resonance imaging-guided intracavitary brachytherapy for cancer of the cervix. Int J Radiat Oncol Biol Phys. 2009;74:1157-64. 8. Pelloski CE, Palmer M, Chronowski GM, et al. Comparison between CT-based volumetric calculations and ICRU reference-point estimates of radiation doses delivered to bladder and rectum during intracavitary radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2005;62:131-7. 9. Wilkinson JM, Harris MA, Davidson SE, et al. A retrospective study of bladder morbidity in patients receiving intracavitary brachytherapy as all or part of their treatment for cervix cancer. Br J Radiol. 2003;76:897-903. 10. Yoshimura R, Hayashi K, Ayukawa F, et al. Radiotherapy doses at special reference points correlate with the outcome of cervical cancer therapy. Brachytherapy. 2008;7:260-6. 11. Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde. Instituto Nacional de Câncer. Incidência do câncer no Brasil: estimativa 2012. Rio de Janeiro, RJ: INCA; 2012. 12. Camisão CC, Brenna SMF, Lombardelli KVP, et al. Ressonância magnética no estadiamento dos tumores de colo uterino. Radiol Bras. 2007;40:207-15. 13. Justino PB, Carvalho HA, Baroni RH, et al. Valor da ressonância magnética no planejamento radioterápico dos tumores de colo de útero: resultados preliminares. Radiol Bras. 2005;38:399-402. 14. Haie-Meder C, Pötter R, Van Limbergen E, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group* (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74:235-45. 15. Hellebust TP, Tanderup K, Lervag C, et al. Dosimetric impact of interobserver variability in MRI-based delineation for cervical cancer brachytherapy. Radiother Oncol. 2013;107:13-9. 16. Viswanathan AN, Creutzberg CL, Craighead P, et al. International brachytherapy practice patterns: a survey of the Gynecologic Cancer Intergroup (GCIG). Int J Radiat Oncol Biol Phys. 2012;82:250-5. 17. Brasil. Ministério da Saúde. Portaria Nº 346, de 23 de junho de 2008. [acessado em 20 de maio de 2013]. Disponível em: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2008/PT-346.htm. 18. Brasil. Ministério da Saúde. Portaria Nº 1.095/GM, de 5 de julho de 2005. [acessado em 20 de maio de 2013]. Disponível em: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2005/GM/GM-1095.htm. 19. Girinsky T, Rey A, Roche B, et al. Overall treatment time in advanced cervical carcinomas: a critical parameter in treatment outcome. Int J Radiat Oncol Biol Phys. 1993;27:1051-6. 20. Perez CA, Grigsby PW, Castro-Vita H, et al. Carcinoma of the uterine cervix. I. Impact of prolongation of overall treatment time and timing of brachytherapy on outcome of radiation therapy. Int J Radiat Oncol Biol Phys. 1995;32:1275-88. 21. Petereit DG, Sarkaria JN, Chappell R, et al. Adverse effect of treatment prolongation in cervical carcinoma. Int J Radiat Oncol Biol Phys. 1995;32:1301-7. 22. Petereit DG, Pearcey R. Literature analysis of high dose rate brachytherapy fractionation schedules in the treatment of cervical cancer: is there an optimal fractionation schedule? Int J Radiat Oncol Biol Phys. 1999;43:359-66. 23. Viswanathan AN, Thomadsen B; American Brachytherapy Society Cervical Cancer Recommendations Committee. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: general principles. Brachytherapy. 2012;11:33-46. 24. Quinn MA, Benedet JL, Odicino F, et al. Carcinoma of the cervix uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet. 2006;95 Suppl 1:S43-103. 25. Pötter R, Haie-Meder C, Van Limbergen E, et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78:67-77. 1. Master, Fellow PhD degree in Physics, Universidade Federal de Sergipe (UFS), São Cristóvão, SE, Brazil 2. Master, Professor, Pontifícia Universidade Católica de Goiás (PUC Goiás), Goiânia, GO, Brazil 3. Specialist in Medical Physics, Physicist at Hospital Chama, Arapiraca, AL, Brazil 4. PhD, Professor, Universidade Federal de Sergipe (UFS), São Cristóvão, SE, Brazil Mailing Address: Rogério Matias Vidal da Silva Departamento de Física - Universidade Federal de Sergipe Avenida Marechal Rondon, s/nº, Jardim Rosa Elze São Cristóvão, SE, Brazil, 49100-000 E-mail: rmv.fisica@gmail.com Received July 9, 2013. Accepted after revision January 22, 2014. Study developed at Department of Physics, Universidade Federal de Sergipe (UFS), São Cristóvão, SE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554