RESUMO
As lesões renais císticas são diagnósticos frequentes na prática do médico radiologista, sendo sua caracterização fundamental na determinação da conduta e prognóstico. A classificação de Bosniak permitiu, por meio de tomografia computadorizada, uniformizar e categorizar tais lesões em ordem crescente de malignidade (I, II, IIF, III e IV), sendo esta avaliação realizada de maneira simples e precisa. Este ensaio iconográfico realizado com tomografia computadorizada multidetectores, de casos selecionados dos arquivos do nosso serviço, tem como objetivo demonstrar achados de imagem que possam auxiliar no reconhecimento dos principais aspectos diagnósticos dos cistos renais.
Palavras-chave:
Classificação de Bosniak; Cistos renais; Tomografia computadorizada multidetectores.
ABSTRACT
Renal cystic lesions are usually diagnosed in the radiologists' practice and therefore their characterization is crucial to determine the clinical approach to be adopted and prognosis. The Bosniak classification based on computed tomography findings has allowed for standardization and categorization of lesions in increasing order of malignancy (I, II, IIF, III and IV) in a simple and accurate way. The present iconographic essay developed with multidetector computed tomography images of selected cases from the archives of the authors' institution, is aimed at describing imaging findings that can help in the diagnosis of renal cysts.
Keywords:
Bosniak classification; Renal cysts; Multidetector computed tomography.
INTRODUÇÃO
As lesões renais são, geralmente, diagnósticos incidentais aos exames de imagem e de necropsia, devido ao seu comportamento assintomático ou como quadro inespecífico das repercussões clínicas(1-3). De acordo com a literatura, as lesões císticas consistem nos achados mais comuns durante a prática diária do radiologista(2,4) e acredita-se que estas sejam lesões adquiridas, pois suas características de incidência e prevalência estão relacionadas a fatores de risco, como o envelhecimento, o sexo masculino, a nefrolitíase, o tabagismo, a hipertensão e a disfunção renal(5,6).
Os cistos renais são de fácil identificação diagnóstica pelos métodos de imagem, não necessitando, muitas vezes, de recursos histopatológicos(4). Entretanto, cistos renais complexos ou com componentes sólidos podem ser evidenciados, necessitando de maior detalhamento em sua caracterização para permitir a determinação de diagnósticos diferenciais, e, consequentemente, da conduta terapêutica e avaliação prognóstica correspondentes(1,7-9).
Em razão desta necessidade, Bosniak, em 1986(4), desenvolveu um esquema de classificação baseado nos critérios de imagem fornecidos pela tomografia computadorizada (TC) que permite analisar os aspectos pertinentes ao contorno e conteúdo do cisto renal, presença de septações e/ou calcificações, e avaliação do realce após a administração intravenosa do meio de contraste.
Por intermédio desta classificação, podemos categorizar as lesões renais císticas em ordem crescente para a probabilidade de malignidade(1,4,9): simples (I), minimamente complicadas (II), minimamente complicadas que requerem seguimento (IIF), indeterminadas (III) ou neoplasias císticas (IV).
O objetivo deste artigo é demonstrar, utilizando a tomografia computadorizada multidetectores (TCMD), os principais aspectos de imagem dos cistos renais de acordo com a classificação de Bosniak.
CATEGORIA I
Os cistos renais simples representam a maioria das lesões renais detectadas por métodos de imagem. São evidenciados por seu conteúdo homogêneo com atenuação de líquido (0-20 UH), contorno regular e nítida interface entre este e o parênquima renal. Não há septações, calcificações ou realce após a administração intravenosa do meio de contraste(8,9) (Figura 1). São de fácil identificação pela ultrassonografia (US), sendo caracterizados por lesões de conteúdo anecoico e parede fina(10).
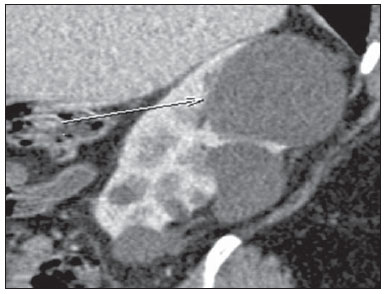
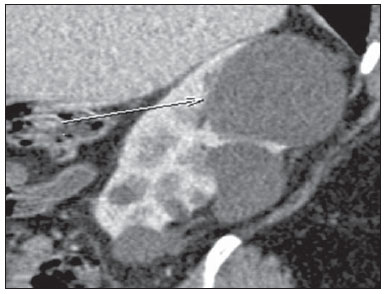
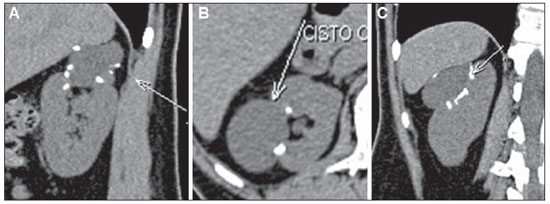
Figura 1.
Categoria I de Bosniak. Imagem de TCMD, reconstrução sagital mostrando lesões císticas com atenuação de líquido, homogêneas, sem calcificações, septações ou realce pós-administração de meio de contraste venoso. Cisto simples. Notar a maior lesão (seta) no polo renal superior.
Quando caracterizados por técnica adequada, lesões com essas características são sempre benignas, com nenhuma chance de malignidade, não havendo necessidade de prosseguir a investigação
(8-10).
CATEGORIA IIAssim como na categoria I, as lesões císticas classificadas na categoria II também são consideradas benignas, porém de aspecto minimamente complicado. Podem apresentar finas septações com espessura inferior a 1 mm (Figura 2), além de pequenas calcificações (1-2 mm) lineares parietais ou septais
(9-15).
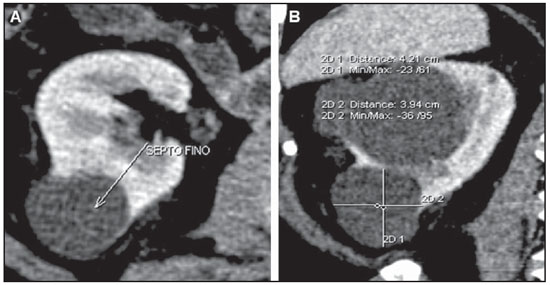
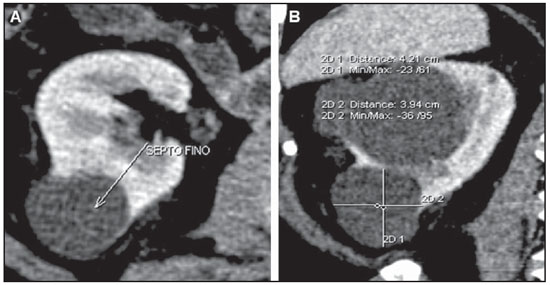
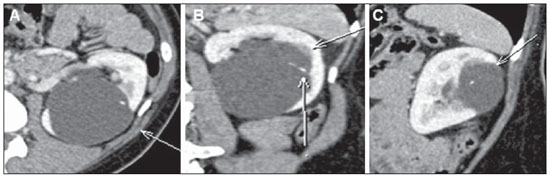
Figura 2.
Categoria II de Bosniak. Imagens de TCMD, reconstruções axial (A) e coronal (B) demonstrando lesão cística com septo fino no seu interior (seta em A). Cisto minimamente complicado.
Nesta categoria também são observados os cistos hiperatenuantes (coeficiente de atenuação superior a 20 UH) que, originalmente, foram descritos como cistos com coeficiente de atenuação maior que o parênquima renal (tipicamente 40-90 UH) na ausência da administração de meio de contraste, e que não apresentam realce quando este for administrado
(1,4,9,16). Um cisto hiperdenso é categorizado como II se seu diâmetro for inferior a 3 cm e parcialmente exofítico, permitindo melhor avaliação da espessura da parede
(9,14) (Figura 3).
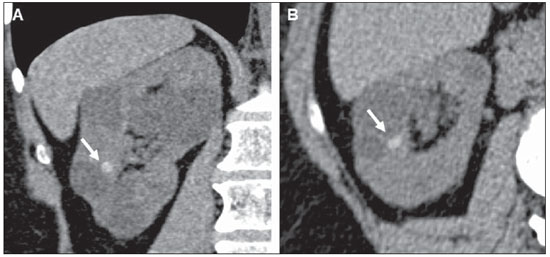
Figura 3.
Categoria II de Bosniak. Imagens de TCMD, reconstruções coronal (A) e axial (B) identificando lesão arredondada hiperatenuante (64 UH de densidade) e medindo cerca de 1,0 cm, podendo corresponder a cisto hemorrágico ou de elevado conteúdo proteico (setas). Cisto minimamente complicado. Notar ainda a presença de cistos simples, categoria I de Bosniak.
Apesar de serem consideradas lesões benignas
(10,12), há relatos na literatura de lesões renais raras, classificadas como categoria II, que foram identificadas como malignas ou potencialmente malignas segundo avaliação anatomopatológica. Nesses casos, é possível que as características das lesões não tenham sido totalmente descritas, interferindo na adequada categorização da lesão. Somam-se também a este contexto outras lesões extremamente raras de carcinoma de células renais nas paredes dos cistos benignos
(9,17-20).
Deste modo, diferenciar lesões mais complexas daquelas classificadas na categoria II (não cirúrgica) causa maior dificuldade diagnóstica, com maior variação entre observadores, embora sejam de extrema importância, pois o prognóstico e a conduta a ser adotada são diferentes
(1,10,11,14,21).
CATEGORIA IIFEm 1993, Bosniak revisou sua classificação original para incluir a categoria IIF
(8,21,22), com base em um grupo de cistos minimamente complicados que não têm características suficientes para serem incluídos na categoria III, porém são mais complexos que os incluídos na categoria II. Sua distinção é subjetiva e difícil, notando-se grande variação entre os observadores, porém é essencial, uma vez que são submetidos a diferentes condutas terapêuticas
(1,8,9,11-13,22-24).
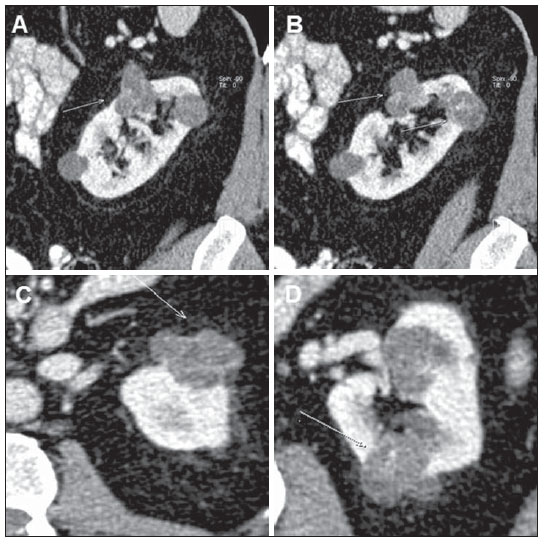
Podem apresentar múltiplos septos finos (Figuras 4 e 5) ou levemente espessados, paredes minimamente espessadas e contorno regular. Podem apresentar realce pós-contraste venoso, porém sem realce do conteúdo cístico
(9,11-13,22,23,25). Cistos hiperdensos completamente intrarrenais, maiores do que 3 cm, com paredes regulares, também são classificados nesta categoria
(9,13,22,25).
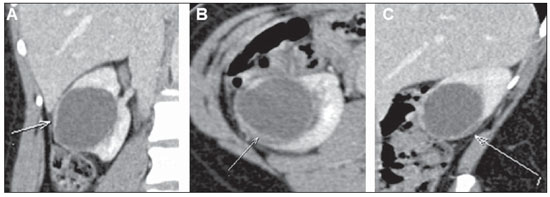
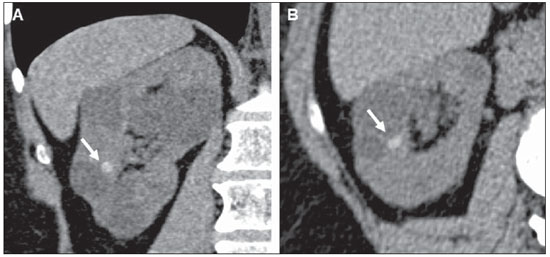
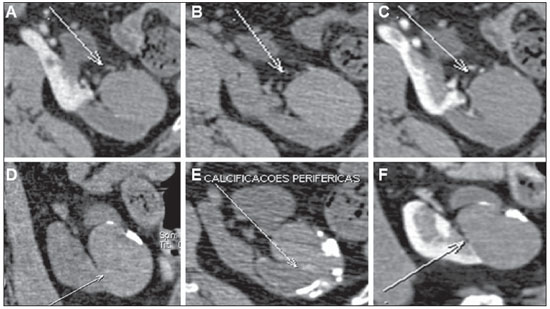
Figura 4.
Categoria IIF de Bosniak. Imagens de TCMD, reconstruções coronal (A), axial (B) e sagital (C) mostrando lesão cística renal direita com espessamento parietal (seta em B) e fino septo (seta em C). Cisto minimamente complicado que requer seguimento.
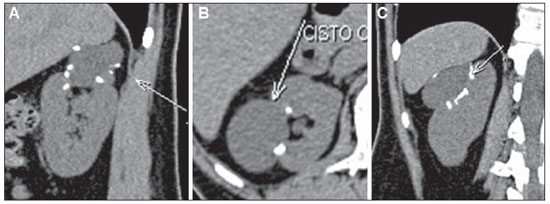
Figura 5.
Categoria IIF de Bosniak. Imagens de TCMD, reconstruções sagital (A), axial (B) e coronal (C) mostrando lesão cística no rim direito com calcificações parietais nodulares. Cisto minimamente complicado que requer seguimento.
Podem conter calcificações nodulares (Figura 5), espessas e com contornos irregulares, e aumentar de volume com o tempo, sem indicar malignidade
(12,13,22,23,25). Israel et al.
(12) demonstraram que todas as lesões classificadas na categoria IIF tinham calcificações, assim como possuíam as maiores concentrações de calcificações. Por causa do elevado número destas calcificações, em algumas lesões poderá ser difícil a visualização do realce pós-contraste, sugerindo-se utilizar a subtração de imagens para distinguir a categoria IIF da III
(12). E, infelizmente, não é possível quantificar as septações ou espessamento da parede para elevar um cisto da categoria II para a categoria IIF
(22).
As lesões na categoria IIF são prioritariamente benignas, mas sua complexidade requer um seguimento seriado ("F" para
follow-up) para afastar, ou não, malignidade
(9,22-25). O tempo adequado de seguimento para determinar se uma lesão é realmente benigna ainda não foi estabelecido
(9,22,23) e varia na literatura. Alguns autores afirmam o início do seguimento 6 meses após o exame inicial, associado a rotina anual por um mínimo de 5 anos
(9,22), ao passo que outros defendem o seguimento em 3, 6 e 12 meses após exame inicial, associado a rotina anual
(26). Esta observação radiológica tem-se mostrado segura, evitando intervenções cirúrgicas em 95% dos casos
(9,10,23).
Uma combinação de US e ressonância magnética (RM) deve ser considerada no seguimento desses pacientes, principalmente nos com menos de 50 anos, pois reduziria a radiação a que o paciente seria submetido ao longo de anos
(23). Uma categoria IIF que não apresenta crescimento ou alterações morfológicas é provavelmente benigna, apesar da velocidade de crescimento não ser uma característica da classificação de Bosniak, devendo o radiologista avaliar, principalmente, as alterações morfológicas
(9).
CATEGORIA IIIEstas lesões compreendem achados renais realmente indeterminados, com ampla variedade de aspectos nos quais os métodos de imagem não podem ser utilizados para diferenciá-las com confiança entre benignas e malignas. Estas lesões possuem espessamento parietal e septações espessas e irregulares realçadas pelo meio de contraste intravenoso, com ou sem calcificações
(9,13) (Figuras 6 e 7). Podem ser evidenciadas como cistos multiloculares (nos quais as paredes têm fibrose linear), cistos hemorrágicos ou infectados, nefroma cístico multilocular (contendo células do blastema), ou carcinoma cístico de células renais. Portanto, têm risco significativo de serem malignas
(1,9,11,12,23).
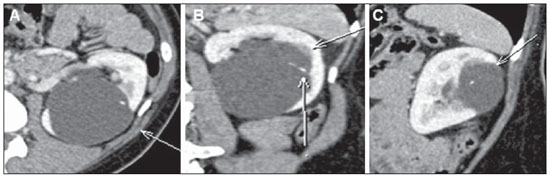
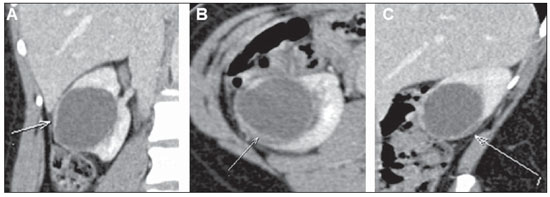
Figura 6.
Categoria III de Bosniak. Imagens de TCMD, reconstruções axial (A), coronal (B) e sagital (C) identificando lesão cística no rim esquerdo com septo fino e calcificações no septo (setas em B). Cisto indeterminado.
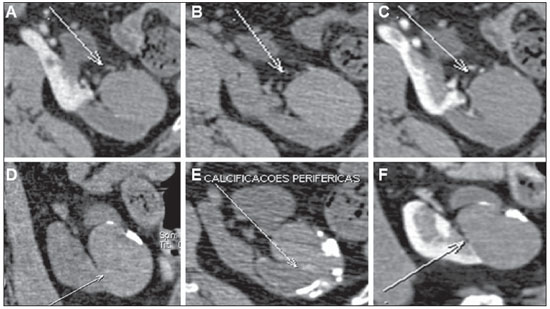
Figura 7.
Categoria III de Bosniak. Imagens de TCMD, reconstruções axiais (A,B,C,E) e coronal (D,B) demonstrando formação hiperatenuante no rim esquerdo com calcificações grosseiras periféricas (seta em E). Cisto indeterminado.
A introdução da categoria IIF englobando lesões benignas antes pertencentes à categoria III resulta que uma maior porcentagem de lesões III seja maligna, pois as lesões provavelmente benignas que eram previamente consideradas III são agora classificadas como categoria IIF e feito o devido seguimento
(9). Quando houver dúvida classificatória, a lesão deve ser considerada na categoria III, permitindo, deste modo, que neoplasias malignas não sejam subdiagnosticadas.
A prevalência de malignidade entre lesões ressecadas da categoria III varia de 31% a 100%
(9,24), mas outros estudos relatam percentual de malignidade entre 40% e 60%
(10). Essas variações devem-se ao modo com que o radiologista estabelece a categoria, à filosofia e à prática de preferência do urologista que trata o paciente com lesões indeterminadas
(9).
Atualmente é possível realizar com segurança o acompanhamento seriado destas lesões, desde que componentes de partes moles não estejam presentes. Se o septo ou parede se tornar espessado ou irregular sem sinal de aumento do componente de partes moles ou sendo este simulado pelo septo, a lesão deve ser considerada III (ou IV) e abordada cirurgicamente
(9,11,12,22,26).
A opção de avaliação por punção percutânea ainda é vista com ceticismo
(26). Em pacientes que apresentem um cisto renal complexo com parede de realce espesso e irregular, frente a uma história ou achados sugestivos de infecção (mesmo remotamente) ou trauma por uma punção prévia, por exemplo, a punção por agulha será indicada
(1).
CATEGORIA IVAs lesões classificadas nesta categoria são neoplasias císticas que podem apresentar características de imagem semelhantes às da categoria III (espessamento parietal ou septal grosseiro e nodular), porém ainda se evidenciam componentes sólidos, que apresentam realce pós-contraste, adjacentes à parede da lesão ou dos septos
(1,9) (Figuras 8 e 9). São consideradas câncer de células renais até que se prove o contrário e possuem indicação eminentemente cirúrgica, pois são malignas em 95-100% dos casos
(9,10).
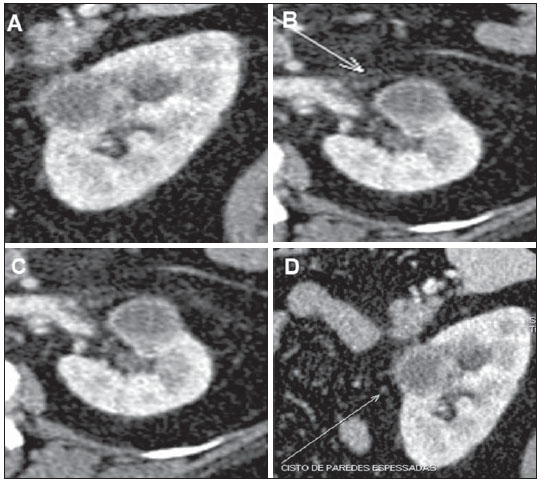
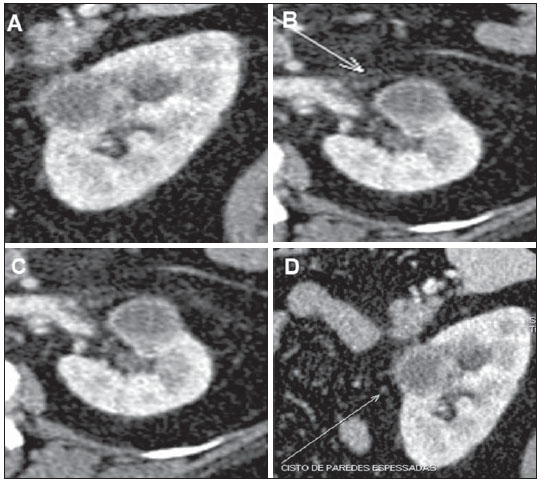
Figura 8.
Categoria IV de Bosniak. Imagens de TCMD, reconstruções sagitais (A,D) e axiais (B,C) demonstrando lesão cística com espessamento parietal grosseiro e nodular.
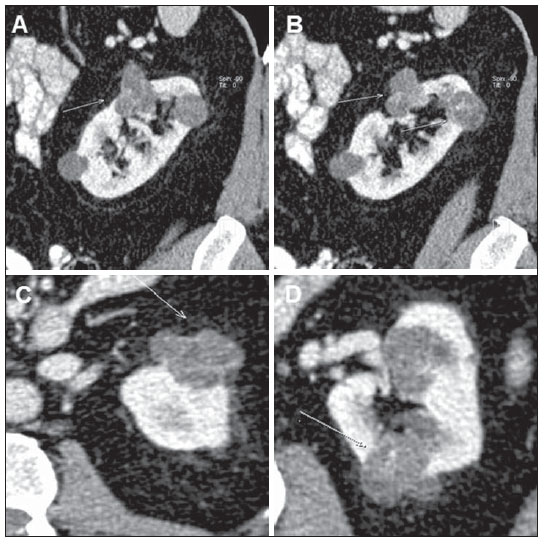
Figura 9.
Categoria IV de Bosniak. Imagens de TCMD, reconstruções sagitais (A,B) e axiais (C,D) identificando lesões císticas lobuladas com septos espessos e realce dos septos pós-administração de meio de contraste.
A diferenciação entre lesões das categorias III e IV pode causar dificuldades ocasionalmente, mas não é essencial, pois ambas necessitam de cirurgia, apesar de diferente abordagem operatória
(10,13).
CONCLUSÃOA classificação de Bosniak torna-se um método prático e acurado para avaliação de lesões císticas renais, limitando, inclusive, o número de diagnósticos de lesões complexas que exigem cirurgia indevidamente. Em razão da sua alta prevalência, os médicos radiologistas e urologistas devem estar familiarizados com sua existência e as características dos métodos de imagem, visando identificá-las e categorizá-las durante a prática diária, além de estabelecer possíveis complicações associadas e auxiliar na conduta terapêutica.
Apesar de a TC ser o método de imagem utilizado para esta classificação, a mesma abordagem pode ser obtida pela RM, que poderá identificar características não visualizadas pela TC, porém estas avaliações por diferentes métodos podem não ser claramente correlacionadas. A RM não evidencia as calcificações, todavia, pode demonstrar alguns espessamentos parietais ou septais não visíveis na TC, resultando em uma reclassificação para um maior grau de malignidade
(1,13).
A US é outro método de imagem bastante utilizado para avaliação inicial de lesões renais, pois consiste num método de baixo custo, fácil acessibilidade, ausência de radiação e do meio de contraste intravenoso
(27). Sua principal característica consiste na identificação de lesões parenquimatosas focais, classificando-as em: cisto simples, nódulo sólido ou indeterminado (cística, porém não simples)
(10,27). Sua falta de precisão diagnóstica, para a classificação de Bosniak, é principalmente decorrente da ausência de material de contraste, uma vez que o reforço dos componentes sólidos de um cisto representa um fator crucial
(25). Porém, trabalhos científicos evidenciam a utilização da US harmônica com meios de contraste de segunda geração, com identificação diagnóstica semelhante à TCMD, assim como se sugere a sua utilização para os que necessitam de seguimento com menor utilização de radiação
(25).
REFERÊNCIAS1. Israel GM, Bosniak MA. How I do it: evaluating renal masses. Radiology. 2005;236:441-50.
2. D'Ippolito G, Torres LR, Ribeiro ACR, et al. Alcoolização percutânea de cistos renais: revisão da literatura e apresentação de resultados. Radiol Bras. 2009;42:225-30.
3. Lee J, Darcy M. Renal cysts and urinomas. Semin Intervent Radiol. 2011;28:380-91.
4. Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1-10.
5. Chang CC, Kuo JY, Chan WL, et al. Prevalence and clinical characteristics of simple renal cyst. J Chin Med Assoc. 2007;70:486-91.
6. Terada N, Arai Y, Kinukawa N, et al. Risk factors for renal cysts. BJU Int. 2004;93:1300-2.
7. Bosniak MA. Dif?culties in classifying cystic lesions of the kidney. Urol Radiol. 1991;13:91-3.
8. Bosniak MA. Diagnosis and management of patients with complicated cystic lesions of the kidney. AJR Am J Roentgenol. 1997;169:819-21.
9. Silverman SG, Israel GM, Herts BR, et al. Management of the incidental renal mass. Radiology. 2008;249:16-31.
10. Sociedade Brasileira de Urologia. Câncer renal: diagnóstico e estadiamento. Projeto Diretrizes. Associação Médica Brasileira e Conselho Federal de Medicina; 2006. [acessado em 20 de fevereiro de 2013]. Disponível em:
www.projetodiretrizes.org.br/6_volume/09-cancerrenaldiagnestad.pdf.
11. Bertolotto M, Zappetti R, Cavallaro M, et al. Characterization of atypical cystic renal masses with MDCT: comparison of 5-mm axial images and thin multiplanar reconstructed images. AJR Am J Roentgenol. 2010;195:693-700.
12. Israel GM, Bosniak MA. Calcification in cystic renal masses: is it important in diagnosis? Radiology. 2003;226:47-52.
13. Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging by using the Bosniak classification system. Radiology. 2004;231:365-71.
14. O'Connor SD, Pickhardt PJ, Kim DH, et al. Incidental finding of renal masses at unenhanced CT: prevalence and analysis of features for guiding management. AJR Am J Roentgenol. 2011;197:139-45.
15. Israel GM, Bosniak MA. An update of the Bosniak renal cyst classification system. Urology. 2005;66:484-8.
16. Bosniak MA. The small (less than or equal to 3.0 cm) renal parenchymal tumor: detection, diagnosis, and controversies. Radiology. 1991;179:307-17.
17. Hartman DS, Weatherby E 3rd, Laskin WB, et al. Cystic renal cell carcinoma: CT findings simulating a benign hyperdense cyst. AJR Am J Roentgenol. 1992;159:1235-7.
18. Chung EP, Herts BR, Linnell G, et al. Analysis of changes in attenuation of proven renal cysts on different scanning phases of triphasic MDCT. AJR Am J Roentgenol. 2004;182:405-10.
19. Siegel CL, McFarland EG, Brink JA, et al. CT of cystic renal masses: analysis of diagnostic performance and interobserver variation. AJR Am J Roentgenol. 1997;169:813-8.
20. Spaliviero M, Herts BR, Magi-Galluzzi C, et al. Laparoscopic partial nephrectomy for cystic masses. J Urol. 2005;174:614-9.
21. Israel GM, Bosniak MA. Follow-up CT of moderately complex cystic lesions of the kidney (Bosniak category IIF). AJR Am J Roentgenol. 2003;181:627-33.
22. Bosniak MA. Problems in the radiologic diagnosis of renal parenchymal tumors. Urol Clin North Am. 1993;20:217-30.
23. Whelan TF. Guidelines on the management of renal cyst disease. Can Urol Assoc J .2010;4:98-9.
24. Smith AD, Remer EM, Cox KL, et al. Bosniak category IIF and III cystic renal lesions: outcomes and associations. Radiology. 2012;262:152-60.
25. Ascenti G, Mazziotti S, Zimbaro G, et al. Complex cystic renal masses: characterization with contrast-enhanced US. Radiology. 2007;243:158-65.
26. Eknoyan G. A clinical view of simple and complex renal cysts. J Am Soc Nephrol. 2009;20:1874-6.
27. Weber TM. Sonography of benign renal cystic disease. Ultrasound Clinics. 2006;1:15-24.
1. Doutora, Membro Titular do Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Coordenadora dos Setores de Tomografia Computadorizada, Ressonância Magnética e Médica Radiologista do Setor de PET-CT da Clínica de Medicina Nuclear e Radiologia de Maceió (MedRadiUS), Professora de Radiologia e Diagnóstico por Imagem da Universidade Federal de Alagoas (UFAL), Maceió, AL, Brasil
2. Membro Titular do Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Médica Radiologista dos Setores de Tomografia Computadorizada e Ressonância Magnética da Clínica de Medicina Nuclear e Radiologia de Maceió (MedRadiUS), Maceió, AL, Brasil
3. Médica Radiologista dos Setores de Tomografia Computadorizada, Ressonância Magnética e PET-CT da Clínica de Medicina Nuclear e Radiologia de Maceió (MedRadiUS), Maceió, AL, Brasil
Estudantes do 6º ano da Faculdade de Medicina da Universidade Federal de Alagoas (UFAL), Maceió, AL, Brasil
Endereço para correspondência:
Dra. Christiana Maia Nobre Rocha de Miranda
Rua Hugo Corrêa Paes, 104, Farol
Maceió, AL, Brasil, 57050-730
E-mail:
maiachristiana@globo.comRecebido para publicação em 21/3/2013.
Aceito, após revisão, em 12/8/2013.
* Trabalho realizado na Clínica de Medicina Nuclear e Radiologia de Maceió (MedRadiUS), Maceió, AL, Brasil.

 |
|