Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 6 - Nov. / Dec. of 2013
Vol. 46 nº 6 - Nov. / Dec. of 2013
|
ICONOGRAPHIC ESSAY
|
|
Typical and atypical presentations of paranasal sinus mucocele at computed tomography |
|
|
Autho(rs): Bruna Vilaça de Carvalho1; Izabella de Campos Carvalho Lopes1; James de Brito Corrêa1; Laura Filgueiras Mourão Ramos2; Emília Guerra Pinto Coelho Motta2; Renata Lopes Furletti Caldeira Diniz2 |
|
|
Keywords: Paranasal sinuses; Mucocele; Presentation; Atypical. |
|
|
Abstract: INTRODUCTION
Paranasal sinuses mucoceles are benign, expansile cystic masses covered by respiratory epithelium, resulting from accumulation and retention of mucus secretion in cases where the sinus drainage is obstructed(1,2). Mucoceles rarely occur in the paranasal sinuses, but such pathology is the most common expansile lesion of these sinuses(2). In spite of being benign, the expansile nature of mucocele may cause paranasal sinuses bone erosion(3) by compression and consequential bone resorption, leading to compromise of adjacent structures. Early diagnosis is of paramount relevance(1). Its incidence is higher between the third and fourth decades of life, but mucoceles may occur at any age range, with no predominance of sex. Such condition is rarely observed in the pediatric population, except for patients with predisponent factors for obstruction such as trauma, surgery, expansile lesion, chronic sinusitis, allergy or cystic fibrosis(1-3). Mucoceles primarily occur in the frontal sinuses (60% to 65%)(2), but may also be found in ethmoid sinuses (20% to 25%), maxillas (10%) and sphenoid sinuses (1% to 2%)(1,3,4). Many times, the primary site of mucoceles cannot be determined because of the progressive osteolysis of the adjacent bone walls, with significant destruction of anatomical parameters, besides veiling of other sinuses caused by obstruction of their drainage ostia(3). The present pictorial essay describes the main characteristics of paranasal sinuses mucoceles, as well as demonstrates and illustrates a series of typical presentations with emphasis on imaging findings. PATHOGENESIS The exact etiology and pathogenesis of mucoceles still remain uncertain. Mucoceles may develop as the communication between the sinuses and the nasal cavity is obstructed(3,5). Usually, mucoceles are post-inflammatory complications (allergy, chronic infection, chronic inflammatory condition, mucociliary dysfunction) but, less usually, may be secondary to neoplastic obstruction (osteoma, juvenile nasoangiofibroma, carcinoma), inflammatory processes (Caldwell-Luc procedure) and post-traumatic processes (iatrogenic accidents), generally with long-term progression(2,4). CLINICAL CONDITION The clinical presentation is variable, according to the affected region, normally with insidious symptoms and slow course, possibly causing facial pain, headache, facial pressure, nasal obstruction, dental pain, ophthalmological alterations and dacryocystitis. As mucocele becomes infected, it is called mucopyocele and may course with sinusitis, orbital cellulitis, erythema, fever and pain. Rarely, intracranial extension may be found in association with meningitis, subdural or cerebral abscess, pneumocephalus or liquoric fistula(2). IMAGING FINDINGS Mucoceles can be diagnosed by means of computed tomography (CT) and magnetic resonance imaging (MRI), and suggested by facial sinuses radiography. CT offers detailed information on the bone structure, and is considered to be the complementary method of choice in the investigation of mucoceles(2,4). Usually, mucoceles is seen as an isodense/mildly hyperdense sinus opacity in relation to the cerebral tissue (Figure 1), but in cases of acute infection, it may appear as a more dense and peripherally enhanced image(3). Thus, considering that mucocele is not enhanced by contrast agents, it is possible to make the differential diagnosis with neoplasms(1). The neighboring bone structure is remodeled with areas of thickening and erosion(3). Additionally, in the areas of greater fragility, one may observe herniation into adjacent structures(4). 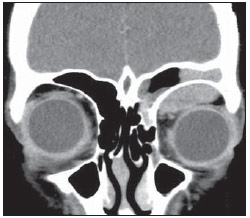 Figure 1. CT with coronal reconstruction showing a slightly hyperdense content as related to the cerebral tissue within the left frontal sinus, with herniation into the orbital cavity. MRI is useful to identify the relation between mucocele, brain tissue, orbit and soft tissues (Figure 2)(5). In spite of not offering detailed images of bones, MRI is useful to rule out the presence of neoplasia in cases of large mucoceles. This imaging method is not routinely utilized, but it is recommended in following situations: CT image showing bone erosion, mucocele extending out from the sinus, and partial loss of vi-sion(1). 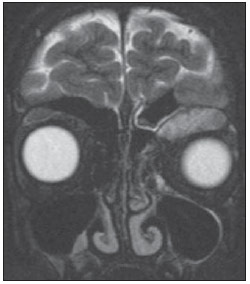 Figure 2. Coronal MRI showing expansile lesion occupying the left frontal sinus with extension towards the orbital cavity. The radiological appearance of mucoceles at MRI varies with the time of evolution of the disease. Initially, the contents will be predominantly aqueous, so the corresponding image will be hypointense on T1-weighted, and hyperintense on T2-weighted sequences. Over time, the protein contents may increase, resulting in hyperintense images both on T1- and T2-weighted sequences. The differential diagnosis for mucocele is made with innumerable inflammatory, congenital, cystic and neoplastic conditions, such as Rathke's cleft cyst, dermoid cyst, cysticercosis, hypophyseal adenoma, craniopharyngioma, optic glioma, besides neoplastic lesions of skull base, facial sinuses and nasopharynx(1). It is important to observe the differentiation between mucoceles and retention cysts: mucoceles develop from sinus ostium obstruction, and the cavity becomes completely filled with mucus involved by the sinusal mucosa; on the other hand, retention cysts do not fill completely the cavity and are formed by the ductal epithelium and by the gland capsule. ATYPICAL PRESENTATIONS Paranasal sinuses mucoceles may be found in atypical locations, such as nasolacrimal duct, intersinus cell, turbinate, in association with osteoma and hematoma, among others. The involvement of the nasolacrimal duct is uncommon and is found principally in the pediatric population, causing nasal obstruction and respiratory discomfort. Nasolacrimal duct mucocele is caused by obstruction of such duct, interrupting the normal flow of tears and resulting in the development of a mass in the medial corner of the orbit (Figures 3 to 6). Typically, patients with nasolacrimal mucoceles present the following triad of imaging findings a) mass in the medial corner of the orbit, representing nasolacrimal duct enlargement; b) nasolacrimal bone duct enlargement secondary to soft tissues which enlarge the nasolacrimal duct; c) intranasal mass representing inferior extension of the mucocele(6).  Figure 3. CT with coronal reconstruction identifying the presence of a mass in the medial corner at left, with erosion of the ipsilateral orbital wall. Also, partial obstruction of the inferior nasal fossa by soft tissue which might represent an inferior extension of the mucocele. 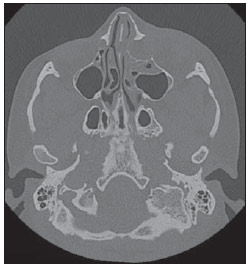 Figure 4. CT with axial section demonstrating the presence of an expansile lesion in the left nasolacrimal duct. 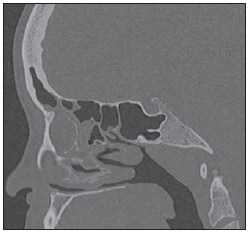 Figure 5. CT with sagittal reconstruction, demonstrating the presence of an expansile lesion in the left nasolacrimal duct. 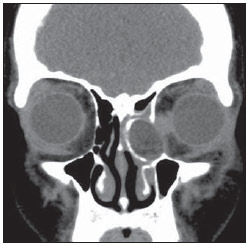 Figure 6. CT with coronal reconstruction demonstrating no significant enhancement of a lesion in the left nasolacrimal duct. Association between mucocele and osteoma is a rarity; only 21 cases with intracranial extension are reported in the literature. In such cases, osteoma is considered as the primary lesion and mucocele, secondary. In most cases, the diagnosis is based on the clinical symptoms associated with intraorbital or intracranial extension of the disease (Figures 7 and 8)(7).  Figure 7. CT with coronal reconstruction for bone structures, demonstrating the presence of an osteoma in the left frontal sinus as well as discontinuity of the superolateral wall of the orbit. 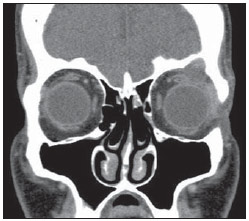 Figure 8. CT with coronal reconstruction for soft tissues. Lesion within the left frontal sinus with extension into the orbital cavity. Mucoceles may also occur after trauma, and their differentiation is important in cases of coexistence with hematoma. In such cases, the higher density of the hematoma can be observed as compared with the density of the mucocele (Figure 9). 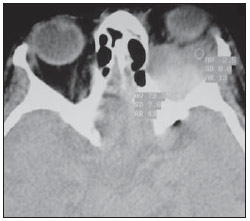 Figure 9. CT with axial section. Higher density is observed on the posterior hematoma as compared with the anterior intraorbital mucocele at left. Intersinus cell is defined as pneumatization at the median line or paramedian bone lamella (septum) between the frontal sinuses. A mucocele may develop within such structure and be either sufficiently large to block unilaterally the frontal sinus ostium, or increase to form a giant mucocele involving both frontal sinuses. Generally, such mucocele erodes the anterior and/or posterior sinuses tables (Figure 10)(8). 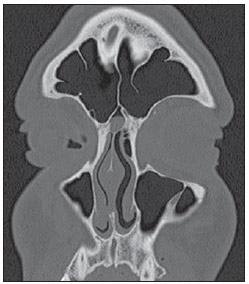 Figure 10. CT with coronal reconstruction. Presence of soft tissue inside the intersinus cell. The pneumatization of the middle turbinate occurs as an extension of the ethmoidal cells, which extends through the superior meatus or through the frontal recess. The interior of the concha bullosa is lined by the respiratory epithelium and generally drains into the middle meatus. In case of obstruction of such drainage, infection may develop progressing to mucocele (Figures 11 to 14)(9).  Figure 11. CT with coronal reconstruction for bone structures. Volumetric increase of the right middle turbinate secondary to the presence of mucocele in the concha pneumatization. 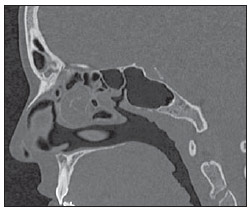 Figure 12. CT with sagittal reconstruction. Volumetric increase of the right middle turbinate secondary to the presence of mucocele in the concha pneumatization. 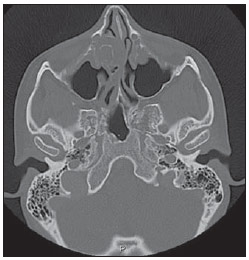 Figura 13. TC com corte axial. Aumento volumétrico da concha nasal média direita secundário à presença de mucocele no interior da pneumatização da concha. 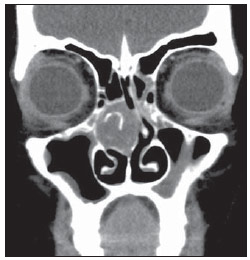 Figura 14. TC com reconstrução coronal para partes moles. Aumento volumétrico da concha nasal média direita secundário à presença de mucocele no interior da pneumatização da concha. MANAGEMENT The management of mucoceles is surgical, aiming at restoring the sinus drainage, and the approach may be either by means of conventional methods (transcranial and transeptal) or by nasal endoscopy(1,2). Currently, the endoscopic surgery is considered the treatment of choice for paranasal sinuses mucoceles(2). The main objective of such method is the complete removal of both the lesion and the sinusal mucosa, thus preventing disease recurrence. CT or MRI may be necessary in the suspicion of recurrence(1). CONCLUSION It is important to know the common findings as well as the atypical presentations of mucoceles for a correct diagnosis and treatment of sinusal and extrasinusal lesions, thus avoiding possible pre- and postoperative clinical complications. REFERENCES 1. Tinoco P, Pereira JC, Lourenço Filho RC, et al. Tratamento nasoendoscópico da mucocele de seio esfenoidal. Arq Int Otorrinolaringol. 2009;13:336-9. 2. Marambaia O, Gomes AM, Marambaia PP, et al. Tratamento endoscópico das mucoceles frontoetmoidais. Rev Bras Otorrinoloaringol. 2008; 74(Supl). 3. Price HI, Batnitzky S, Karlin CA, et al. Computed tomography of benign disease of the paranasal sinuses. Radiographics. 1983;3:107-40. 4. Towbin R, Dunbar JS. The paranasal sinuses in childhood. Radiographics. 1982;2:253-79. 5. Cavazza S, Bocciolini C, Laudadio P, et al. Two anomalous localizations of mucocele: clinical presentation and retrospective review. Acta Otorhinolaryngol Ital. 2007;27:208-11. 6. Koch BL. Case 73: Nasolacrimal duct mucocele. Radiology. 2004;232:370-2. 7. Sakamoto H, Tanaka T, Kato N, et al. Frontal sinus mucocele with intracranial extension associated with osteoma in the anterior cranial fossa. Neurol Med Chir. 2011;51:600-3. 8. Som PM, Lawson W. Interfrontal sinus septal cell: a cause of obstructing inflammation and mucoceles. AJNR Am J Neuroradiol. 2008;29:1369-71. 9. Sala CR, Fuster MA, Molina JV, et al. Mucocele de concha bullosa con afectación orbitaria. Acta Otorrinolaringol Esp. 2002;53:46-9. 1.MDs, Residents, Department of Radiology and Imaging Diagnosis, Hospital Mater Dei, Belo Horizonte, MG, Brazil 2.MDs, Radiologists, Hospital Mater Dei, Belo Horizonte, MG, Brazil Mailing Address: Dra. Bruna Vilaça de Carvalho Rua Pernambuco, 753, Savassi Belo Horizonte, MG, Brazil, 30130-151 E-mail: brunavilaca@gmail.com Received November 23, 2012. Accepted after revision April 5, 2013. Study developed at Instituto de Pesquisa e Pós-Graduação da Faculdade de Ciências Médicas de Minas Gerais / Hospital Mater Dei, Belo Horizonte, MG, Brazil |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554