Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 5 - Sep. / Oct. of 2013
Vol. 46 nº 5 - Sep. / Oct. of 2013
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Amanda Nogueira de Sá Gonçalves Ligabô1; João Maurício Canavezi Indiani2; Marcelo Fontalvo Martin2; Rodrigo Ciotola Bruno3; Paulo Maurício Chagas Bruno4; Marcelo Souto Nacif5 |
|
|
A female, 67-year-old patient complaining of rectal and vaginal discomfort mainly during defecation, reported the feeling of a "lump" in the vagina during straining from coughing and evacuation. Symptoms persisted for five years until the patient sought evaluation by a proctologist. The patient reported one normal delivery following prolonged labor, 30 years ago. The patient was submitted to defecography for diagnosis. (Figures 1 and 2).
 Figure 1. Defecography at rest, during contraction and during Valsalva.  Figure 2. Defecography during evacuation, during forced evacuation and after evacuation. DESCRIPTION OF THE IMAGES Figure 1. Presence of anterior rectocele measuring 5.1 cm, posterior rectocele with 3.7 cm and enterocele at rest. The patient presented with subtle rectoperineal descent at rest. The contraction was efficient, causing satisfactory rectal angulation. The findings characterize flaccidity of the puborectal muscle. Figure 2. A: Observe that, during evacuation, there is a significant worsening of the anterior rectocele, measuring 11.6 cm, protruding towards the vagina, in association with internal rectal prolapse (intussusception) and worsening of the enterocele, which now causes compression of the rectum (grade II). The rectoperineal descent is clear. B: During forced evacuation there is a worsening of the anterior rectocele, which reaches 11.6 cm, leading to external rectovaginal prolapse, intussusception and enterocele with rectoperineal descent. C: In the post evacuation stage, there is no active return of the structures to the anatomical position, requiring manual readaptation. Diagnosis: Genital dystopia characterized by rectovaginal prolapse, enterocele and intussusception diagnosed at defecography. COMMENTS Defecography is a radiological method for the study of defecation, providing images of morphofunctional changes of the pelvis and of the anorectal segment. It is a valuable method for the study of the physiology of the pelvic dynamics and colorectal disorders(1). Physical examination is many times difficult and inaccurate, underestimating the prolapse of pelvic organs in approximately 45% to 90% of cases. Additionally, the physical examination may not diagnose associated prolapses. Dysfunction of multiple compartments is commonly found, and the preoperative diagnosis is extremely important as it modifies the surgical approach. The inability in diagnosing such condition may cause therapeutic failure and symptoms recurrence(2). Genital prolapse is defined as caudal displacement of pelvic viscera towards the genital hiatus. It is secondary to imbalance between the forces which maintain the pelvic organs in their normal position and the forces which tend to impel them to the outside of the pelvis(3). As there are several organs suspended in the pelvic cavity, it is possible to identify different types of genital prolapse, which many times occur concomitantly. Genital prolapse can also be called colpocele. In cases of anterior colpocele, or cystocele, the bladder presses the anterior vaginal septum, forming a prominence in the interior of the vaginal canal. In case of posterior colpocele, or rectocele, the rectum presses the posterior vaginal septum, forming a procidentia inside the vaginal canal. The same occurs in enterocele, where the prolapse affects the upper part of the posterior vaginal septum, leading to the development of a herniation constituted by a portion of the bowel(4). Rectoceles may be asymptomatic or cause intestinal symptoms such as difficulty or discomfort in evacuation, flatus or fecal incontinence and local symptoms such as sense of fullness in the vagina, pressure, pain or dyspareunia(5). According to the volume and descent of the cystocele, of the uterine prolapse or of the rectocele, they may be classified as follows: a) grade 1: when there is some degree of descent of the vaginal wall and adjacent organ (bladder, uterus or rectum) during straining, without reaching the vaginal introitus; b) grade 2: when greater descent of the vaginal wall and adjacent organ occurs, reaching the vaginal introitus, without overcoming it completely. Grade 2 perineal tear is a partial tear at the level of the perineal body, with laceration of the pelvic diaphragm, reaching the anus; c) grade 3: protrusion of the vaginal wall and the adjacent organ toward or through the opening of the vagina. A grade 3 uterine prolapse occurs as the third degree prolapse when the entire uterine body protrudes entirely outside the vagina. In cases of grade 3 perineal tear, there is a complete separation of the perineal body and anal sphincter, with apposition of the vaginal mucosa to the rectal mucosa(6). In cases of complications, there is a risk to the patients, for example in cases of cystocele, uterine prolapse or grade 3 rectocele, where keratinization of a dry and constantly exposed vaginal epithelium may occur. Even ulceration of the prolapsed segment may be observed because of local ischemia. In more extreme cases, there may be incarceration of the prolapsed segment (generally the uterus), due to important edema and/or infection of the exposed region, precluding the return of the organ to the interior of the vagina. Rarely, cancer may develop in the vagina or in the prolapsed uterine cervix(6). In the present case, defecography (Figure 3) was fundamental for a deeper understanding of the physiopathology of evacuation and the impact on the patient's quality of life. The measurement of the anorectal angle demonstrated satisfactory contraction and evacuation, causing the expected rectal angulation, which becomes more acute during contraction and obtuse during evacuation. The measurement of the puborectal muscle remained the same in all phases (26 cm), characterizing the non relaxation of such muscle during evacuation. It was also possible to characterize the presence of anterior and posterior rectocele, enterocele, perineal descent, rectal intussusception and rectovaginal prolapse. 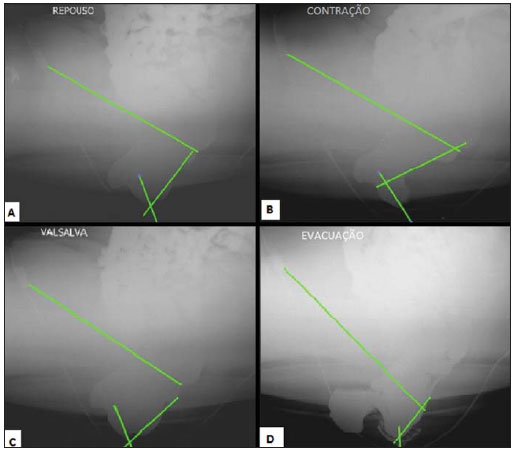 Figure 3. Defecography in the four phases of the study: rest, contraction, Valsalva and evacuation, demonstrating the measurement of the anorectal angle and measurement of the puborectal muscle. FINAL CONSIDERATIONS Vaginal prolapse directly interferes in the quality of life of the patient and for that reason it should be diagnosed the earliest possible to allow a swift and appropriate management. Defecography presents a good sensitivity for early detection of external and internal prolapsed of pelvic organs through the vagina and rectum. In the present case, the patient was submitted to surgery for correction of anterior and posterior rectocele, enterocele and recto-vaginal protrusion by means of vaginal (posterior colporrhaphy) and abdominal approach. Cystocele repair was performed at the same surgical time. Three months after the surgery, the patient had favorably evolved, with no pelvic complaints. REFERENCES 1. Sobrado CW, Pires CEF, Amaro S, et al. Videodefecografia: aspectos técnicos atuais. Radiol Bras. 2004;37;283-5. 2. Karasick S, Karasick D, Karasick SR. Functional disorders of the anus and rectum: findings on defecography. AJR Am J Roentegenol. 1993;160:777-82. 3. Mezwa DG, Feczko PJ, Bosanko C. Radiologic evaluation of constipation and anorectal disorders. Radiol Clin North Am. 1993;31:1375-93. 4. Ganeshan A, Anderson EM, Upponi S, et al. Imaging of obstructed defecation. Clin Radiol. 2008;63:18-26. 5. Castro EB, Palma PCR, Herrmann V, et al. Defeitos do compartimento vaginal posterior: fisiopatologia e tratamento da retocele. Femina. 2007;35:363-7. 6. Salvatore CA. Tratamento cirúrgico do prolapso uterino. São Paulo: Livraria Roca; 1982. 1. MD, Trainee (1st year), Unidade de Radiologia Clínica, São José dos Campos, SP, Brazil 2. MD, Radiologists, Unidade de Radiologia Clínica, São José dos Campos, SP, Brazil 3. Master, MD, General Surgeon and Coloproctologist, Hospital Vivalle, São José dos Campos, SP, Brazil 4. MD, General Surgeon and Coloproctologist, Hospital Vivalle, São José dos Campos, SP, Brazil 5. Associate Professor, Department of Radiology, School of Medicine, Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil Mailing address: Dr. Marcelo Souto Nacif Rua Barão de Cocais, 324, Bosque Imperial São José dos Campos, SP, Brazil, 12242-042 msnacif@gmail.com / www.msnacif.med.br Study developed at Unidade de Radiologia Clínica (URC) and Hospital Vivalle, São José dos Campos, SP, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554