Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 3 - May / June of 2013
Vol. 46 nº 3 - May / June of 2013
|
REVIEW ARTICLE
|
|
Cochlear implant: what the radiologist should know |
|
|
Autho(rs): Natália Delage Gomes1; Caroline Laurita Batista Couto1; Juliana Oggioni Gaiotti1; Ana Maria Doffémond Costa1; Marcelo Almeida Ribeiro2; Renata Lopes Furletti Caldeira Diniz2 |
|
|
Keywords: Cochlear aplasia; Labyrinthine aplasia; Sensorineural hypoacusis; Cochlear implant; Computed tomography. |
|
|
Abstract: INTRODUCTION
Cochlear implant is the method of choice in the treatment of deep sensorineural hypoacusis, notably in those patients for whom conventional amplification devices do not provide noticeable clinical improvement. Imaging findings are decision making factors in the indication or contraindication for such surgical procedure and the radiologist must be familiar with such alterations. Thus, multislice computed tomography (CT) (64 detectors) and high-field thin section magnetic resonance imaging (MRI) with three-dimensional reconstructions are essential to provide data that previously could not be revealed by other imaging methods. Furthermore, the increase in number of cochlear implants increased the demand for investigation with such imaging methods. Based on a recent literature review, the present study was aimed at highlighting the importance of the radiologist in the evaluation of patients eligible for cochlear implant, particularly in the definition of factors which might contraindicate surgery or hinder a successful outcome of the procedure, by means of a comprehensive clinical and imaging evaluation of such factors. DISCUSSION Cochlear implant consists in the subcutaneous implantation of a receptor behind the ear and a cochlear electrode passing through the mastoid cavity, which directly stimulates the acoustic nerve. The receptor sends a signal to the electrode implanted at the basal coil of the cochlea. Such signal is transformed into an electrical stimulation which propagates throughout the remaining auditory pathways until reaching the auditory cortex of the temporal lobe (Figure 1). Thanks to such a process, a great part of sensorineural hypoacusis cases can be reversed by means of the cochlear implant, as the sounds are received by a microphone, in the form of codes which are decoded, and directly stimulate the cochlea (implant), being converted into electrical signals. In those cases of cochlear nerve aplasia, where the implant is contraindicated, there is the possibility of stimulating the ganglion at the brain stem(1–4).  Figure 1. Illustrative drawing depicting a cochlear implant comprising an external receptor and the cochlear electrode. The procedure consists in a small incision behind the auricle, followed by mastoidectomy and opening of the facial recess in order to reach the basal coil of the cochlea, next to the round window, and insertion of the cochlear electrode(1–3). Postoperative imaging studies also contribute to define the window created by the surgeon, confirm the location of the electrodes, detect the presence of labyrinthitis ossificans in the basal coil of the cochlea, next to the round window, demonstrate fluid collections suggestive of cerebrospinal fluid fistula or abscess, and even visualize the facial nerve to rule out postoperative complications in that structure (many times it is necessary to compare postoperative with preoperative images)(1,5). Absolute contraindications A detailed radiological study is indicated to evaluate criteria which are still considered as absolute contraindications for the implant, such as cochlear nerve aplasia (evidenced by MRI), cochlear and/or labyrinthine aplasia, in spite of reports questioning the two latter contraindications(2,6–10). Labyrinthine aplasia is determined by the complete absence of the internal ear, including the cochlea, the vestibulum and semicircular canals. The symptoms consist of congenital sensorineural deafness, sometimes associated with Klippel-Feil syndrome and exposure to thalidomide. The CT findings in the milder cases demonstrate the petrous bone involving labyrinth structures, petrous apex hypoplasia, narrow internal auditory canal and normal middle ear. On the other hand, in severe cases, absence of the internal auditory canal and of the petrous apex bone, absence or fusion of the ossicles may be observed. The facial nerve canal is prominent and the geniculate ganglion is more posterior than normal. On MRI T2-weighted sequences, the high signal intensity from the fluid contained in the membranous labyrinth is not observed, with absence of the vestibulocochlear complex. In cases of unilateral labyrinthine aplasia, the implantation is contralaterally performed, and, if bilateral, (deep deafness), the cochlear implant is contraindicated, and the remaining option is the utilization of a hearing aid device(2,9). In cases of cochlear aplasia, only the cochlea is absent while the other components of the internal ear are present in various forms (dysmorphic). It is also congenital sensorineural deafness, usually bilateral. CT demonstrates absence of the cochlea, and the vestibulum, semicircular canals and the internal auditory tube may be normal, hypoplastic or dilated (Figure 2). The cochlear promontory is flat, and the labyrinth, geniculate ganglion and tympanic portion of the facial nerve occupy the space of the cochlea(3). Cochlear aplasia may be associated with cochlear nerve aplasia, which is only visualized at MRI (Figures 3 and 4)(2). 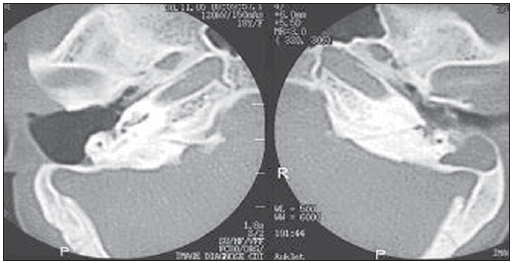 Figure 2. Comparative axial CT sections. Absence of cochlear coils at left, compatible with cochlear aplasia. 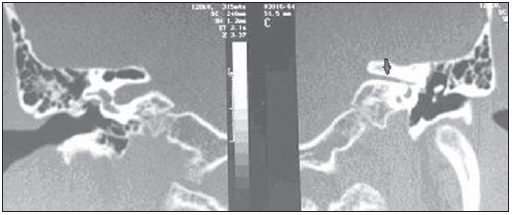 Figure 3. Comparative coronal CT sections. Narrowing of the left internal auditory canal, an indirect sign of cochlear nerve aplasia (arrow). 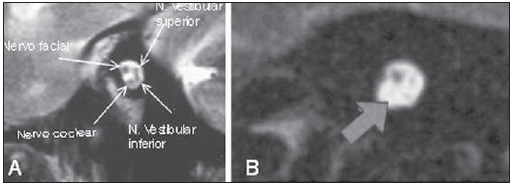 Figure 4. Sagittal MRI T2-weighted images. A: Anatomical distribution of the nerves inside the internal auditory canal. B: Absence of the cochlear nerve (arrow). Relative contraindications Relative contraindications for cochlear implantation include cochlear dysplasias, particularly labyrinthitis ossificans, which may be secondary to infection, inflammation, trauma or previous surgery of the internal ear. Labyrinthitis ossificans affects the fluid-filled spaces of the membranous labyrinth, sometimes with ossification in the form of focal or diffuse plates, with consequential sensorineural deafness and vertigo. CT demonstrates high density bone deposition in the membranous labyrinth. On the other hand, MRI is superior to demonstrate the focus that is not yet calcified. Such cochlear calcification does not contraindicate the implantation, but its imaging documentation is required, since such condition could make cochleostomy more difficult to be performed (Figure 5)(6,9). 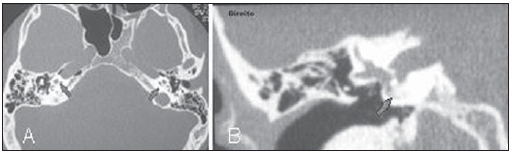 Figure 5. Computed tomography – axial (A) and coronal (B) sections. Increased density within the basal coils of the cochleae, compatible with calcifications (arrows). Complicating factors Hypoplastic mastoid process is included in the range of complicating factors: when unilateral, such a finding favors the contralateral placement of the implant, in the spared side (Figure 6).  Figure 6. Axial CT section. Bilateral decreased mastoid cells aeration. Enlargement of the ducts and endolymphatic sacs is the most common amongst congenital internal ear abnormalities detectable at imaging studies. Such condition is generally bilateral, associated with cochlear dysplasia and abnormalities of the vestibular system semicircular canals. It is more commonly found in children under the age of ten. Sensorineural deafness deepens after one year, or fluctuations in the level of such deafness may be observed after a potentializing trauma event. CT demonstrates the enlargement of the vestibular aqueduct and MRI demonstrates the enlarged endolymphatic sac on the posterior wall of the temporal bone (Figure 7)(6). 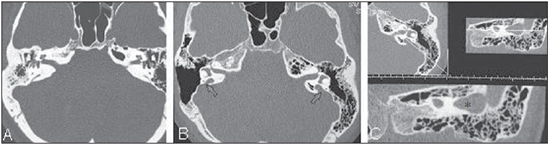 Figure 7. Axial CT sections (A,B) and oblique multiplanar reconstruction (C). Normal appearing vestibular aqueducts (A) and bilateral dilation of vestibular aqueducts (B,C – arrows and asterisk). Mastoiditis and/or otitis media present as opacification of the middle ear and mastoid cells, sometimes complicating with mastoid septa erosion (coalescent otomastoiditis), abscess, meningitis, thrombophlebitis, sigmoid sinus thrombosis, among other factors (Figure 8)(6,9). 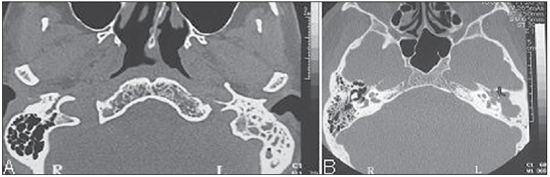 Figure 8. Axial CT sections. A: Total opacification of mastoid cells at left in association with bony septa sclerosis. B: Chronic cholesteatomatous otomastoiditis at left, with important opacification of the tympanic antrum and membrane in association with ossicular chain erosion (arrow). Otosclerosis, a primary disorder of the endochondral layer of the labyrinthine bone, evolves with focal lytic plates progressing to calcification in some cases. Fenestral otosclerosis is most frequently associated with conductive hearing loss, while cochlear otosclerosis may induce sensorineural deafness due to involvement of the basilar membrane. The condition is bilateral and symmetrical in 95% of the cases, and its causes are still to be established. Cochlear otosclerosis is generally followed by fenestral otosclerosis. CT is the method of choice, and gadolinium-enhanced MRI demonstrates focal contrast uptake in the active phase. The most common focus is anteriorly located in relation to the oval window, but it may involve any bone of the medial of the middle ear wall (Figure 9)(6). 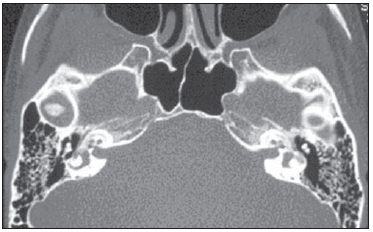 Figure 9. Axial CT section. Bilateral pericochlear bone demyelination (retrofenestral otosclerosis). The preoperative detection of aberrant or dehiscent facial nerve may prevent possible facial palsy secondary to the procedure, as the nerve would be out of its pathway and the surgeon would be aware of this abnormality prior to the procedure (Figure 10)(2,9).  Figure 10. A: Curve reconstruction along the entire normal osseous neural canal of the facial nerve, demonstrating that it is caudally located in relation to the lateral semicircular canal (CAI, internal auditory canal) B: Oblique reconstruction demonstrating part of the aberrant facial nerve (minor arrows) superiorly located in relation to the lateral semicircular canal (major arrow). C: Coronal CT reconstruction showing tympanic segment of the enlarged right facial nerve, positioned anteriorly to the oval window (arrow). Aberrant internal carotid artery results from a congenital vascular abnormality where a small segment of the internal carotid artery is inside the middle ear. CT demonstrates a tubular vascular structure surrounding the cochlear promontory, associated with enlargement of the inferior tympanic canaliculus and absence of the carotid foramen and of the vertical segment of the carotid artery (Figure 11)(6,9). 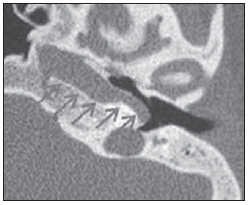 Figure 11. Axial CT image. Aberrant carotid artery at left inside the middle ear. Persistence of stapedial artery represents another congenital abnormality, usually asymptomatic, whose diagnosis is made intraoperatively or at imaging studies demonstrating enlargement of the anterior tympanic segment of the facial nerve canal and absence of the spinous foramen. Association with aberrant internal carotid artery may be observed (Figure 12)(3). 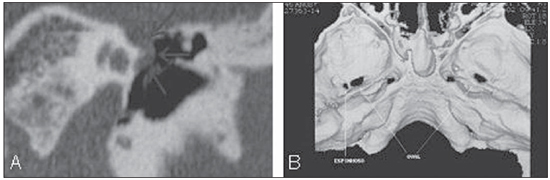 Figure 12. A: Coronal CT reconstruction demonstrating persistent stapedial artery at left: enlargement of the facial nerve canal, with projection of the artery towards the middle year (arrows). B: 3D CT reconstruction showing normal appearing spinous foramen at right and absence at left. Jugular bulb dehiscence is a usually asymptomatic anatomical variant, with superior and lateral extension of the jugular bulb into to the middle ear, through the dehiscent sigmoid plate (Figure 13)(6). 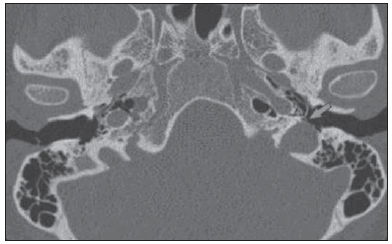 Figure 13. Axial CT section. Absence of the bone septum between the jugular bulb at left and the hypotympanum, with minimum protrusion into the hypotympanum (arrow). CONCLUSIONS The correct classification of cochlear conditions and a clear description of such abnormalities by means of multislice CT and high-field MRI are determining factors in the surgical planning developed by the cochlear implantation team, with direct impact on the success of the surgical intervention. Thus the radiologist experienced in the evaluation of the temporal bone plays a major role in the course of this disorder. REFERENCES 1. Powitzky ES, Hayman LA, Chau J, et al. High-resolution computed tomography of temporal bone: Part IV: Coronal postoperative anatomy. J Comput Assist Tomogr. 2006;30:548–54. 2. Witte RJ, Lane JI, Driscoll CL, et al. Pediatric and adult cochlear implantation. Radiographics. 2003;23:1185–200. 3. Lammers MJ, van der Heijden GJ, Grolman W. Cochlear implants in children and adolescents. Arch Pediatr Adolesc Med. 2012;166:677. 4. Mackeith S, Joy R, Robinson P, et al. Pre-operative imaging for cochlear implantation: magnetic resonance imaging, computed tomography, or both? Cochlear Implants Int. 2012;13:133–6. 5. Bouccara D, Mosnier I, Bernardeschi D, et al. Cochlear implant in adults. Rev Med Interne. 2012;33:143–9. 6. Harnsberger HR, Wiggins RH, Hudgins PA, et al. Diagnostic imaging: head and neck. 1st ed. Salt Lake City, UT: Amirsys; 2004. 7. Lima Júnior LR, Rocha MD, Walsh PV, et al. Evaluation by imaging methods of cochlear implant candidates: radiological and surgical correlation. Braz J Otorhinolaryngol. 2008;74:395–400. 8. Chaturvedi A, Mohan C, Mahajan SB, et al. Imaging of cochlear implants. Indian J Radiol Imaging. 2006;16:385–92. 9. Swartz JD, Harnsberger HR. Imaging of the temporal bone. 3rd ed. New York, NY: Thieme Med Publ; 1998. 10. Fishman AJ. Imaging and anatomy for cochlear implants. Otolaryngol Clin North Am. 2012;45:1–24. 1. MDs., Trainees in Radiology and Imaging Diagnosis at Hospital Mater Dei – Mater Imagem, Belo Horizonte, MG, Brazil. 2. MDs, Radiologists, Preceptors, Unit of Radiology and Imaging Diagnosis, Hospital Mater Dei – Mater Imagem, Belo Horizonte, MG, Brazil. * Study developed in the Unit of Radiology and Imaging Diagnosis, Hospital Mater Dei, Belo Horizonte, MG, Brazil. Mailing Address: Dra. Natália Delage Gomes Rua Padre Marinho, 480, ap. 302, Santa Efigênia Belo Horizonte, MG, Brazil, 30140-140 E-mail: nataliadelagegomes@gmail.com Received June 16, 2012. Accepted after revision October 19, 2012. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554