Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 3 - May / June of 2013
Vol. 46 nº 3 - May / June of 2013
|
ORIGINAL ARTICLE
|
|
Cranial computed tomography findings in patients admitted to the emergency unit of Hospital Universitário Cajuru |
|
|
Autho(rs): Lauro Aparecido Lara Filho1; Samir Sari Omar2; Rodrigo Foletto Biguelini2; Rony Augusto de Oliveira Santos2 |
|
|
Keywords: Computed tomography; Craniocerebral trauma; Imaging diagnosis. |
|
|
Abstract: INTRODUCTION
A number of recent studies published in Brazil have highlighted the relevance of neuroradiology for the diagnosis and treatment of several diseases(1–11). Computed tomography (CT) was developed by the British physicist Godfrey Hounsfield and was first utilized at the Atkinson Morley Hospital, London, in 1972, and quickly became one of the main methods for the evaluation of structural brain disorders(12–14). Currently, the method relies on an X-ray tube that spins 360° and is equipped with photon detectors opposite to the X-ray source. The image will depend upon the thickness of the object and its capability of absorbing the X-rays. The detector transforms the emitted photons into analogical signals (by means of voltage) and then a computer transforms such signals into digital ones(12,15,16). There is a convention utilized to translate the detected voltage values into digital units, the absorption coefficient (attenuation). It is calculated in relation to the linear coefficient of water, for which the numeric value 0 is attributed, in a scale that may range from +1,000 to –1,000 Hounsfield units (HU) and is represented by a gray scale comprising a large spectrum of tones representation between white, gray and black (Table 1)(15,16). 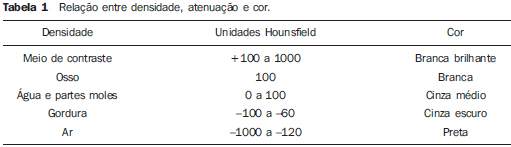 With the advent of magnetic resonance imaging, cranial studies by means of CT became better indicated in acute situations such as those encountered at specialized emergency services. CT is the imaging method of choice in the evaluation of head trauma (HT) as it can demonstrate bone and parenchymal changes, besides hemorrhages. It is a very important method as it is accessible because of its wide availability, lower cost and low acquisition time. Magnetic resonance imaging, on its turn, presents some limitation in patients with implanted materials, such as clips or pacemakers, claustrophobia or obesity, which do not prevail in CT(17–19). At the CT unit of Hospital Universitário Cajuru (HUC), the main indications for cranial CT include: decreased consciousness level without known causes; alcohol or drug intoxication; focal neurological deficit; suspected penetrating injury or skull fracture; consciousness loss during or after trauma; ages < 2 years and > 65 years with a history of HT; unreliable history; reports of post-trauma vomiting; post-trauma amnesia; signs of skull base fracture; polytrauma; severe facial trauma; significant extracranial soft tissue swelling; and suspicion of child abuse. Because of the shortage of local scientific studies (Curitiba metropolitan area) evaluating the prevalence of cranial CT findings and, considering that HUC is a specialized emergency service where such imaging method is required, the present investigation became necessary to evaluate the service, as well as to analyze the prevalence of findings. Thus, the present study was aimed at recognizing and analyzing the prevalence of cranial CT findings in patients admitted to the emergency unit of HUC in Curitiba, PR, Brazil. MATERIALS AND METHODS A cross-sectional study was undertaken with sequential analysis of 200 cranial CT reports of patients admitted to the HUC's emergency unit in the period between January 1st and February 9, 2008. All the patients admitted to the HUC's emergency unit who were submitted to cranial non contrast enhanced CT were included in the present study, regardless of gender and age. Only reports of patients submitted to contrast-enhanced scan were excluded. The scans were performed with the patients in dorsal decubitus, in a Siemens Somaton Spirit apparatus, with the following acquisition parameters: 130 kVp, 100 mAs, axial plane, 3 mm-thick slices for the posterior fossa, and 10 mm-thick slices for the remaining areas of the skull, without intravenous contrast injection. Two report patterns were considered and recorded as being normal: without volume reduction and with volume reduction (normal pattern for elderly patients). Normal pattern without volume reduction – Absence of expansile lesions, extra-axial collections or pathological calcifications in the encephalon; ventricular system with normal morphology, topography and dimensions; anatomical features of the basal cisterns, as well as of the sulci between the cortical gyri in the brain convexities. Diagnostic impression: study within the normality limits. Normal pattern with volume reduction – Absence of expansile lesions, extra-axial collections or pathological calcifications in the encephalon; dilation of the ventricular system (ex-vacuo); prominence of the cerebellar folia, basal cisterns, Sylvian fissure as well as of the sulci between the cortical gyri in the brain convexities. Diagnostic impression: brain and cerebellar volume reduction. All the other CT findings, such as hypodense lesions or collections, microangiopathy, hyperdense lesions or collections, hemorrhages, expansile lesions (tumor, hematoma, hemorrhages), soft-tissue volume increase, calcifications, atheromas, fractures, alterations secondary to surgical procedures (craniotomy, aneurysmal clips, shunt catheter), pneumocephalus, signs of intracranial hypertension (hydrocephalus, edema, hernias, ventricular asymmetries, midline structures displacement and focal obliteration of sulci), sinusal alterations, foreign body, metal fragments and anatomic variations, were considered abnormal and exposed to analysis, establishing a relation between number of findings and total number of scans. RESULTS In the sample of this study, 47 patients (23.5%) presented results within the normality standards. Thus, 153 patients (76.5%) presented alterations detected by CT. The most common finding was intracranial soft-tissue swelling, observed on 44 (22%) of the 200 CT scans. The bone fractures found in 33 patients (16.5%) are shown on Table 2. 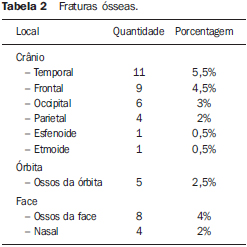 The findings of ectopic air collections included pneumocephalus, observed in 11 patients (5.5%), and intra-orbital emphysema, in one patient (0.5%). Hyperdensities and hypodensities are listed on Tables 3 and 4, respectively. 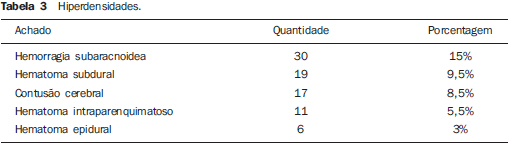 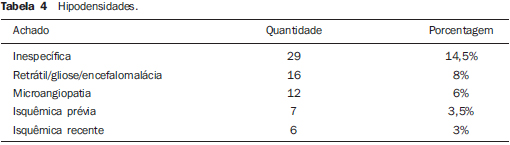 Ventricular alterations and signs of intracranial hypertension are represented on Table 5. 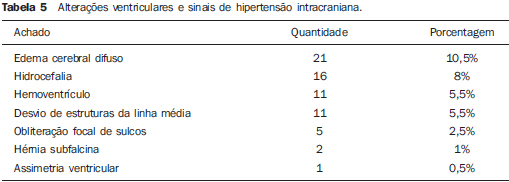 Abnormal findings observed in the nose, nasal cavity and paranasal sinuses were the following: veiling of paranasal sinuses, in 23 patients (11.5%); sinusopathy, in 13 patients (6.5%); and septal deviation in 2 patients (1%). Veiling and sclerosis of the mastoid process was observed in 4 patients (2%). The following types of pathological calcifications were observed: intraparenchymal calcifications, with 15 findings (7.5%); calcified atheromas in the carotid or vertebral system, with 14 (7%) findings; and eyeball calcifications with 2 (1%) findings. As regards expansile lesions, there were 5 (2.5%) findings – 3 (1.5%) hypodense and 2 (1%) heterogeneous –; 2 (1%) parenchymal heterogeneities and one (0.5%) corpus callosum lipoma. Craniotomy was found in 15 (7.5%) patients, one (0.5%) of them with herniation. Ventricular shunt catheters were found in 10 (5%) patients. In addition, motion artifacts were found on 12 scans, impairing their results, 7 (3.5%) metal fragments, 4 (2%) aneurysmal clips and 2 (1%) orotracheal tubes. Cavum vergae, an anatomic variation, was found in 2 (1%) patients. The 10 most prevalent findings are listed on Table 6 and the most relevant images are shown on Figures 1, 2 and 3. 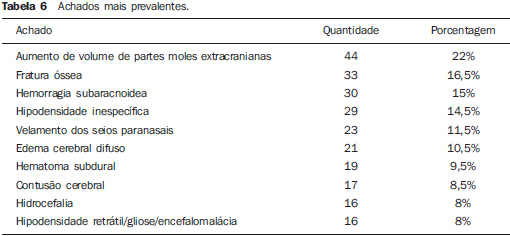 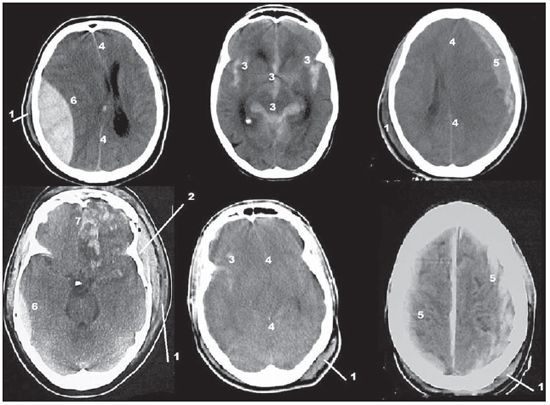 Figure 1. 1, extracranial soft-tissue swelling; 2, depressed bone fracture; 3, subarachnoid hemorrhage; 4, midline structures displacement/diffuse cerebral edema; 5, subdural hematoma; 6, epidural hematoma; 7, cerebral contusion in frontal pole (straight and orbital gyri). 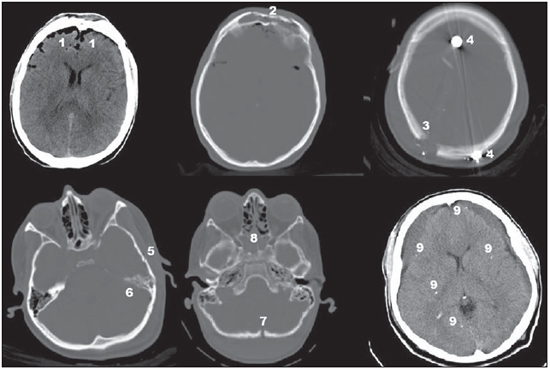 Figure 2. 1, pneumocephalus; 2, frontal bone fracture; 3, right posterior parietal orifice made by meandering bullet entry; 4, metal fragments representing projectile or shrapnel; 5, left temporal bone fracture; 6, veiling of left mastoid cells; 7, occipital bone fracture; 8, veiling of the sphenoidal sinus and some ethmoid cells; 9, pathological intraparenchymal calcifications associated with hypodense subdural collections. 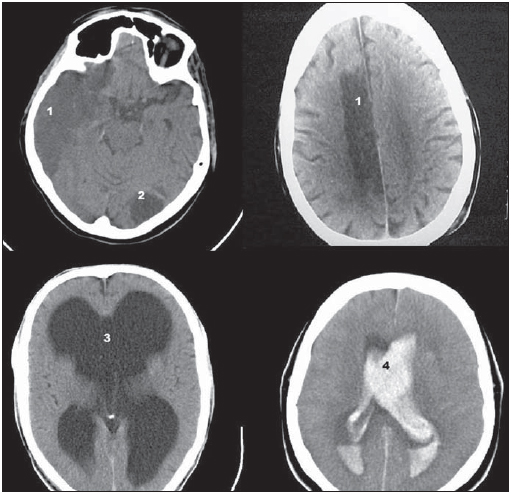 Figure 3. 1, recent ischemic hypodensity; 2, previous ischemic hypodensity; 3, hydrocephalus; 4, ventricular hemorrhage. DISCUSSION In the present study, 23.5% of the scan results were found to be normal. Such result is similar to that obtained by Rocha(20) (25.3%), and is inferior to the results reported by Palheta et al.(21) (46.4%). It is important to highlight that in those two studies, only CT scans with indication for HT investigation were considered, while in the present study all CT scans performed in the emergency unit were considered, regardless of their indication. Palheta et al.(21) have justified the high index of normal results by the fact that, at those authors' institution, cranial CT is routinely performed for mild HT, an indication which is not supported by Conselho Federal de Medicina (Federal Medicine Council)(22) for all patients. In the opinion of the authors of the present study, their findings are within the expected levels for an emergency unit, considering the current indications for cranial CT. The most prevalent finding was extracranial soft-tissue swelling (22%). Such finding was also prevalent in the study developed by Rocha(20), with 57%, by Bordignon et al.(23), with 47%, and by Palheta et al.(21), with 44.3%. Such an alteration is typical in cases of HT, and for such reason its prevalence was higher in those studies. Bone fracture was found in 33 patients (16.5%), and was the second most prevalent finding in the present study. The most common one was temporal bone fracture, with 5.5%, a value that is close to the 4.7% reported by Amin et al.(24). Pneumocephalus is an air collection inside the cranial cavity that may be secondary to surgery or procedures, skull base fracture, congenital defects, tumors causing bone erosion and infection by gas producing bacteria(15,18). Such finding had a prevalence of 5.5% in the present study, while Rocha(20 found 9.3% and Palheta et al.(21) found 7.1%. Hyperdensity may indicate the presence of hemorrhages, hematomas, collections, among other findings(15,16,18). The most common one was subarachnoid hemorrhage, with 15%, and was the third most prevalent finding in the study. Such a finding was observed by Rocha(20) in 22.4% of his patients, a higher prevalence than that reported by Stein et al.(25) and by Palheta et al.(21), with respectively 5.7% and 6.4%. Cerebral contusion was found in 8.5% of the CT scans in the present study. Such a finding was observed by Rocha(20) in 24.4% of his patients, in 12.9% by Bordignon et al.(23) and in 8.6% by Palheta et al.(21). Subdural and epidural hematomas had a prevalence of 9.5% and 3%, respectively, the latter with a lower prevalence than that reported by Palheta et al.(21), of 4.3%, and by Rocha(20), of 8%. Subdural hematoma was found by Rocha(20) in 7.3% of his patients, by Palheta et al.(21) in 10%, and by Servadei et al.(26), in 11% of the patients. Intraparenchymal hematoma was found in 5.5% of patients, while Rocha(20) and Palheta et al.(21) found 6.7% and 11.4%, respectively. Hypodensity may indicate the presence of tumor, abscess, hematoma in resolution, ongoing infarction, chronic hematoma, chronic infarction, encephalomalacia, microangiopathy (microvascular ischemic damage), among others(15,16,18). In the present study, hypodensity of nonspecific type was the most prevalent (14.5%), representing the fourth most prevalent finding in the study. The second most prevalent type of hypodensity was retractile hypo-dense area/gliosis/encephalomalacia, in 8% of the patients. Microangiopathy was the third most prevalent, with 6%. It is important to note that, in the present study, the authors considered as nonspecific findings those that were not described as typical ischemic lesions, microangiopathy or encephalomalacia. Intracranial hypertension may be caused by an expansile process (tumor, hematoma, cysts, abscess, empyema and granuloma), hydrocephalus, cerebral edema, metabolic disorder, and intoxication by prescription drugs or other types of drugs(16,18). Among the findings related to intracranial hypertension and ventricular alterations, the authors of the present study observed diffuse cerebral edema (10.5%); hydrocephalus (8%); intraventricular hemorrhage (5.5%); midline structures displacement (5.5%); and subfalcine herniation (1%). In their study, Palheta et al.(21) have found diffuse edema in 5.7% of their cases, while Rocha(20) has observed such finding in 8.2% and midline structures displacement in 9.1% of his cases. Palheta et al.(21) highlight that midline structures displacement is commonly associated with subfalcine herniation, being such herniation the most common in this case. The present study did not found any other related herniations. Intraventricular hemorrhage was found by Rocha(20) in 2.7% of his cases, and such finding was not observed by Palheta et al.(21). Because of the intimate association with surrounding structures, isolated paranasal sinuses injuries are uncommon. Association between bone injuries, including those in the paranasal sinuses, with intracranial and extracranial soft tissues are more common(27). This explains the fact that veiling of the paranasal sinuses was observed in 11.5% of the cases, the fifth most prevalent finding in the present study, probably associated with other HT injuries. Veiling and sclerosis of the mastoid process were found in 2% of the patients. According to Secchi et al.(28),such finding is present in 25% of temporal bone fractures. In the present study, sinus hemorrhage and changes in the content of the sinuses were not discriminated. Intracranial calcifications represent frequent incidental findings at numerous neurological imaging studies(29). In the present study, calcifications with greater significance were intraparenchymal calcifications (7.5%) and calcified atheromas in the carotid or vertebral system with (7%). Craniotomy, observed in 7.5% of cases, as well as aneurysmal clips, in 1.0%, are due principally to postoperative follow-up. Metal fragments corresponding to projectiles or shrapnel were found in 3.5% of the patients. Rocha(20) has found them in 4.4% of the cases and Palheta et al.(21), in 1.4%. It is important to remind that the main studies utilized in the discussion of the data, such as those published by Rocha(20), Palheta et al.(21) and Bordignon et al.(23), have exclusively evaluated patients with indication of CT for HT. The present study did not discriminate the indication for cranial CT scan, but, considering that the HUC is a reference emergency service, HT was the main indication for the CT scans. As limitations inherent to the present study, the authors highlight that the study period of one month and nine days might give room to possible seasonal variations, and that the evaluation was based only on a report made by a single radiologist and not by consensus between two radiologists. Another limitation was the absence of reports standardization, as many times different radiologists utilize different terms for a single type of finding, a fact which required a revision of the tables and data proposed by the authors. It is also important to mention the difficulty in finding studies describing CT findings in emergency settings, and for such reason it would be appropriate to undertake further studies with the same objective. CONCLUSIONS The authors recognize that the most common non-contrast-enhanced cranial CT findings in emergency settings reported by other studies are similar to those observed in the present study. Such findings include extracranial soft-tissue swelling (22%), bone fracture (16.5%), subarachnoid hemorrhage (15%), nonspecific hypodensity (14.5%), veiling of paranasal sinuses (11.5%), diffuse brain edema (10.5%), subdural hematoma (9.5%), cerebral contusion (8.5%), hydrocephalus (8%), and retractile hypodensity/gliosis/encephalomalacia (8%). Such data are important to enable the professionals in the service to recognize the mains findings to be identified at cranial CT and for a future planning and hospital screening, with the purpose of obtaining efficiency and improvement in the rendered services. REFERENCES 1. Fernandes RCL, Rosso ALZ, Vincent MB, et al. Transcranial sonography findings in Parkinson's disease and essential tremor: cases report. Radiol Bras. 2012;45:356–8. 2. Coeli GNM, Silva GC, Tiengo RR, et al. Cerebelite aguda com herniação tonsilar: relato de caso. Radiol Bras. 2012;45:244–6. 3. Sanches P, Yamashita S, Freitas CCM, et al. Chordoid glioma of the third ventricle: a new case report. Radiol Bras. 2012;45:288–90. 4. Gonçalves FG, Hanagandi PB, Torres CI, et al. Posterior migration of lumbar disc herniation – imaging dilemma due to contrast contraindication: a case report. Radiol Bras. 2012;45:170–2. 5. Barros ML, Fernandes DA, Melo EV, et al. Malformações do sistema nervoso central e malformações associadas diagnosticadas pela ultrassonografia obstétrica. Radiol Bras. 2012;45:309–14. 6. Coeli GNM, Tiengo RR, Silva AC, et al. Neurocisticercose nodular calcificada com sinais de reativação. Radiol Bras. 2012;45:291–3. 7. Nogueira-Barbosa MH, Savarese LG, Herrero CFPS, et al. Raízes nervosas redundantes da cauda equina: revisão da literatura. Radiol Bras. 2012;45:155–9. 8. Jurno ME, Castro MHA, Lage MA, et al. Síndrome de desmielinização osmótica: relato de caso com evolução favorável. Radiol Bras. 2012;45:61–2. 9. Wajnberg E, Rodrigues G, Abud DG. O uso de stents farmacológicos no tratamento da estenose das artérias vertebrais. Radiol Bras. 2011;44:343–8. 10. Gonçalves FG, Barra FR, Matos VL, et al. Sinais em neurorradiologia – Parte 1. Radiol Bras. 2011;44:123–8. 11. Barra FR, Gonçalves FG, Matos VL, et al. Sinais em neurorradiologia – Parte 2. Radiol Bras. 2011;44:129–33. 12. Beckmann EC. CT scanning the early days. Br J Radiol. 2006;79:5–8. 13. Hounsfield GN. Computerized transverse axial scanning (tomography): Part 1. Description of system. Br J Radiol. 1973;46:1016–22. 14. Ambrose J. Computerized transverse axial scanning (tomography): Part 2. Clinical application. Br J Radiol. 1973;46:1023–47. 15. Gunderman R. Fundamentos de radiologia. 2ª ed. Rio de Janeiro, RJ: Guanabara Koogan; 2007. 16. Koch HA. Radiologia e diagnóstico por imagem na formação do médico geral. 2ª ed. Rio de Janeiro, RJ: Revinter; 2012. 17. Haaga JR. Tomografia computadorizada e ressonância magnética do corpo humano. 3ª ed. Rio de Janeiro, RJ: Guanabara Koogan; 1996. 18. Leite CC, Amaro Jr E, Lucato LT. Neuroradiologia – diagnóstico por imagem das alterações encefálicas. Rio de Janeiro, RJ: Guanabara Koogan; 2008. 19. American College of Radiology. ACR Appropriateness Criteria® Head Trauma. Last review date: 2008. [acessado em 20 de maio de 2011]. Disponível em: http://gm.acr.orgSecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonNeurologicImaging/HeadTraumaDoc5.aspx. 20. Rocha CMN. Traumatismo cranioencefálico: correlação entre dados demográficos, escala de Glasgow e tomografia computadorizada de crânio com a mortalidade em curto prazo na cidade na cidade de Maceió, Alagoas [tese]. São Paulo, SP: Faculdade de Medicina – Universidade de São Paulo; 2006. 21. Palheta MS, Nunes RB, Targino MN, et al. Achados tomográficos dos pacientes vítimas de traumatismo cranioencefálico atendidos no Hospital Metropolitano de urgência e emergência. Rev Para Med. 2009;23(2). 22. Andrade AF, Marino Jr R, Miura FK, et al. ABM/CFM Projeto diretrizes. Diagnóstico e conduta no paciente com traumatismo craniencefálico leve. Brasil; 2001. 23. Bordignon KC, Arruda WO. CT scan findings in mild head trauma: a series of 2,000 patients. Arq Neuropsiquiatr. 2002;60:204–10. 24. Amin Z, Sayuti R, Kahairi A, et al. Head injury with temporal bone fracture: one year review of case incidence, causes, clinical features and outcome. Med J Malaysia. 2008;63:373–6. 25. Stein SC, Ross SE. Mild head injury: a plea for routine early CT scanning. J Trauma. 1992;33:11–3. 26. Servadei F, Nasi M, Giuliani G, et al. CT prognostic factors in acute subdural haematomas: the value of the 'worst' CT scan. Br J Neurosurg. 2000;14;110–6. 27. Mathog RH, Arden RL, Marks SC. Trauma of the nose and paranasal sinuses. New York, NY: Thieme Med Publ; 1995. 28. Secchi MMD, Moraes JFS, Castro FB. Fratura de osso temporal em pacientes com traumatismo crânio-encefálico. Arq Int Otorrinolaringol. 2012;16:62–6. 29. Piñol-Ripoll G, Mauri-Llerda JA, de la Puerta Martínez-Miró I, et al. Differential diagnosis of intracranial calcifications. Rev Neurol. 2005;41:151–5. 1. Specialist in Radiology and Imaging Diagnosis, Professor, Course of Medicine, Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba, PR, Brazil. 2. Students, Course of Medicine, Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba, PR, Brazil. * Study developed at Hospital Universitário Cajuru – Pontifícia Universidade Católica do Paraná (PUCPR), Curitiba, PR, Brazil. Mailing Address: Samir Sari Omar Rua Alferes Poli, 464, ap. 1407, Rebouças Curitiba, PR, Brazil, 80220-050 E-mail: samir176@gmail.com Received July 10, 2012. Accepted after revision February 19, 2013. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554