Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013
|
ORIGINAL ARTICLE
|
|
Morbidity of transrectal ultrasound guided prostate biopsy |
|
|
Autho(rs): Raphael Sandes Solha1; Sérgio Ajzen2; Harley De Nicola3; David Carlos Shigueoka4; Hugo Alexandre Sócrates de Castro5 |
|
|
Keywords: Prostate; Biopsy; Morbidity; Ultrasonography; Complications. |
|
|
Abstract: INTRODUCTION
Prostate cancer is the most common neoplasia among men in America, and the second cause of cancer death in this population group(1). Also in Brazil, prostate cancer is the most common type of cancer among men, and according to Instituto Nacional de Câncer, 52,350 new cases were estimated in 2010(2). In most of cases, the disease affects individuals above the age of 50, and it is a heterogeneous entity whose features vary from asymptomatic presentations to fast-growing disease(3). Its mortality rate is relatively low, especially cases with early diagnosis. Such mortality rate has decreased over the recent years, with five-year survival rates reaching 99% because of screening programs, early detection and changes in life style(4). In spite of developments in different imaging diagnosis methods applied to evaluate pelvic diseases, the confirmation of prostate cancer diagnosis is still achieved by means of histological evaluation of specimens obtained by transrectal biopsy(5,6), a procedure that is generally safe and well tolerated by patients. However, some studies have reported complication rates of up to 73%, as immediate and spontaneous resolution events are included(7). In the Unit of Nonvascular Intervention, Department of Imaging Diagnosis of Escola Paulista de Medicina - Universidade Federal de São Paulo (DDI/EPM-Unifesp), a reference center for a great part of the population from the Southern region of the city of São Paulo, approximately 80 prostate biopsies are performed every month, comprising 36% of the total number of procedures performed in that unit. Normally, complications following transrectal biopsy of the prostate are mild and self-limited, including hematuria, hematospermia or transient rectal bleeding. Sometimes, more severe complications such as urinary retention, infectious events and important rectal bleeding may occur, requiring further treatment(8). The present study was aimed at evaluating the incidence of post-procedural complications in patients submitted to transrectal US-guided biopsy of the prostate in the Unit of Intervention of DDI/EPM-Unifesp. MATERIALS AND METHODS In the period from April to July 2011, 132 patients with clinical and laboratory suspicion of prostate cancer were referred to the authors' institution referred to the authors´ sector for clinical or laboratorial prostate cancer suspect were sequentially submitted to transrectal prostate biopsies and were sequentially evaluated. All the patients were submitted to the same transrectal ultrasound guided prostate biopsy protocol utilized in the unit, after prophylactic antibiotic therapy with ciprofloxacin. After positioning the patient in left lateral decubitus with flexed thighs, an endocavitary transducer coupled with a specific biopsy probe was inserted, and the transrectal sonographic evaluation of the prostate was performed. Then, periprostatic block anesthesia was performed with 5 ml of 2% lidocaine diluted in 5 ml of saline solution, utilizing an 18-gauge needle. After anesthesia, the biopsy was performed with collection 12 representative gland specimens utilizing an 18-gauge needle, following the sextant pattern recommended by Colégio Brasileiro de Radiologia e Diagnóstico por Imagem and by Sociedade Brasileira de Urologia. Upon sonographic findings (focal lesions in the peripheral zone) or upon medical request (palpation findings or saturation re-biopsy - 18 specimens) additional specimens were collected. The patients were discharged after first urination with no evidence of significant hematuria and after being properly instructed on a possible onset of late complications. By means of telephone interviews, questionnaires were filled out on febrile or hemorrhagic adverse events occurring within 14 days after prostate biopsy. In such a questionnaire, the events were reported as hematuria, hematospermia or hematochezia, measured febrile event, chills, dysuria or urinary retention and respective progression and/or treatments. Among the 132 patients who underwent biopsy in the period, 29 were excluded because of contact impossibilities after three attempts at different days and times, four for having undergone the procedure during hospital stay, and one for death by unrelated cause (cardiovascular event) and one for having been submitted to the procedure under a different protocol from that established by the institution (under sedation). For evaluation purposes, the complications were divided into two groups: major complications and minor complications. Major complications were those which led the patients to seek emergency medical assistance after being discharged. All the other complications were considered as being minor, self-limited and inherent to the risks associated with an invasive procedure. RESULTS The 97 selected patients were aged between 43 and 83, with a mean age of 66.2 years. Among the patients, 38 (39.2%) did not present with any adverse event after prostate biopsy. On the other hand, 51 patients (52.6%) reported at least one minor complication, most of them (76.5%) with only an isolated symptom or sign. In this group, macroscopic hematuria was the most prevalent complication, reported by 39 patients. The hematuria lasted from one to ten days (men 3.2 days), with 62.5% of such cases presenting spontaneous resolution within the first three days and 5% of the cases persisting for more than one week. Hematospermia was the second most frequent reported sign, present in 23.7% of the patients after biopsy. Most of such patients (82.6%) presented spontaneous remission of the hematospermia, while the symptom persisted in four patients at the time of the telephone interview. None of such patients reported the need to seek medical assistance for such a reason. Two patients (2%) reported hematochezia, both cases with spontaneous resolution, one within one day and the other after 7 days. As regards major complications, eight patients (8.2%) required emergency medical evaluation. Among them, seven (87.5%) sought medical assistance for urinary retention, requiring urinary catheter insertion, with three of the patients requiring associated home antibiotic therapy. Three patients (3.1%) reported fever, in two cases associated with dysuria, requiring urinary catheter insertion and home antibiotic therapy. One of the patients with measured fever reported spontaneous resolution, with no need of further specific treatment. Only one patient reported persistent hematuria in association with dysuria, leading him to seek medical assistance at the hospital where he was admitted for treatment with antibiotics. However such patient reported concomitant respiratory symptoms, which has impaired the direct correlation between such an event and the procedure itself. Other five patients also reported dysuria, although with spontaneous resolution, without the need for additional medical evaluation. Chills were the symptoms with the lowest prevalence, being reported by only one patient, in association with fever and urinary retention. Table 1 shows the complications reported by the patients. 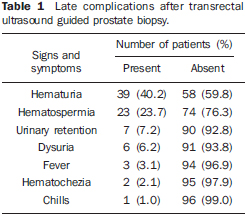 DISCUSSION Early detection of prostate cancer is critical for a favorable prognosis, with consequential reduction in morbidity in patients presenting with the disease. With the increase in prostate cancer screening, both in private and public services, the number of transrectal ultrasound guided biopsies tends to increase, so the knowledge on the inherent complications of the method(9) becomes indispensable for both the interventional radiologist and the requesting physician. In the present study, 59 patients (60.8%) reported at least one late complication after prostate biopsy. Some other studies, such as that developed by Miller et al., have found less significant complication rates, achieving 9.6%, however the authors have not taken minor and self-limited complications into consideration(10). In the absence of an effective standardization of the post-procedural complications, the authors of the present study have opted for considering the need for further medical evaluation as a definition of major complication, because of its greater socioeconomic impact. Thus a prevalence of 8.2% for major complications and 52.6% for minor complications were observed. Such rates are equivalent to those reported by other studies in the international literature, such as the one developed by Rodriguez et al., who have found similar prevalence (63.6%) of post-procedural complications, also with hematuria being the main symptom found by those authors (47.1%)(11). Post-biopsy macroscopic hematuria is generally a self-limited and very common event, reported by 40.2% of the patients included in the present study. In a study undertaken in Rotterdam, Holland, Rietbergen et al. have evaluated 1,687 patients submitted to prostate biopsies, and found a similar prevalence (45.3%)(12). For being a very common symptom, some authors, such as Raaijmakers et al., have considered as being complications only those cases where hematuria persisted for more than three days(13), obtaining a prevalence of 22.6%. In the present study, only eight (8.2%) patients met that criterion. Hematospermia was the second most commonly found sign, present in 23.7% of the patients included in the present study, with none being considered as a major complication. In the literature, a great variation - from 9.1% to 78.3% - is observed with respect to the prevalence of hematospermia following prostate biopsy(11,14). The highest prevalence (78.3%) was reported by Peyromaure et al., who have considered only the relationship between hematospermia and patients who reported sexual activity in the evaluated period(14). As related to the total number of patients, a prevalence of 54.9% was found, a rate that is much higher than the prevalence observed in the present study. Generally associated with urinary tract infections (UTI), dysuria, fever or chills were reported by ten patients included in the present study, but, among those patients, only three (3.1%) were characterized as major events. Urinary tract infection is considered as being the second most frequent complication of prostate biopsy, only after hemorrhagic complications. In spite of being a simple event, UTI occurs with a certain frequency after prostate biopsies, and febrile UTIs are not uncommon after the procedure(15,16). Sepsis is one of the most severe complications, albeit rare, being found in less than 2% of cases(12). In the authors' institution, since 2007, only one patient required admission to intensive care unit because of sepias following prostate biopsy, and was released after 14 days of treatment. Studies have evidenced the presence of asymptomatic bacteriuria and transient bacteremia in 16% to 100% of cases after the procedure(17,18), hence the current consensus on the importance of prophylactic antibiotic therapy in the preparation of the patient before performance of the biopsy, with the purpose of maintaining the low rates of complications caused by such procedure(19,20). However, many studies have pointed out the lack of a standard algorithm to be followed in such preparation(21). In spite of the fact that in the present study the rate of major complications (8.2%) was comparable to those in most services performing such studies utilizing similar criteria(22), a high incidence of urinary retention was observed as compared with similar studies in the literature (Table 2). Among the risk factors for urinary retention in the general population, several such factors are present in the patients submitted to biopsy: previous history of obstruction caused by increased prostate volume or by potential obstruction due to presence of hematuria, concomitant infection - particularly prostatitis -, and use of drugs with anticholinergic properties (tricyclic antidepressants, alpha adrenergic blockers and non-steroidal anti-inflammatory drugs). Some postoperative conditions are similar to those observed after biopsy, for example occurrence of pain or anesthetic procedure(23). In the authors' experience, the patients discharge only after the first clear urination should suffice to prevent such complication. Besides highlighting such patients discharge criterion, such finding demonstrates the need for further studies to investigate its possible causes, indicating new criteria or additional measures aimed at further reducing the incidence of such complications. 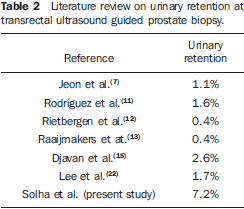 CONCLUSION The authors conclude that, in spite of the rate of urinary retention reported by patients in the present study being higher than average in the cited studies, the prevalence of major and minor complications in their institution is comparable to that in other services dedicated to this procedures, corroborating their safety and the low incidence of major late complications. REFERENCES 1. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71-96. 2. Ministério da Saúde. Instituto Nacional de Câncer. Câncer de próstata. In: Estimativa 2010. Incidência de câncer no Brasil. Rio de Janeiro, RJ: INCA; 2009. 3. Kelloff GJ, Choyke P, Coffey DS; Prostate Cancer Imaging Working Group. Challenges in clinical prostate cancer: role of imaging. AJR Am J Roentgenol. 2009;192:1455-70. 4. Kundra V, Silverman PM, Matin SF, et al. Imaging in oncology from the University of Texas M. D. Anderson Cancer Center: diagnosis, staging, and surveillance of prostate cancer. AJR Am J Roentgenol. 2007;189:830-44. 5. Goldman SM. Ressonância magnética da próstata. Radiol Bras. 2009;42(3):vii-viii. 6. Santos VCT, Milito MA, Marchiori E. O papel atual da ultra-sonografia transretal da próstata na detecção precoce do câncer prostático. Radiol Bras. 2006;39:185-92. 7. Jeon SS, Woo SH, Hyun JH, et al. Bisacodyl rectal preparation can decrease infectious complications of transrectal ultrasound-guided prostate biopsy. Urology. 2003;62:461-6. 8. Berger AP, Gozzi C, Steiner H, et al. Complication rate of transrectal ultrasound guided prostate biopsy: a comparison among 3 protocols with 6, 10 and 15 cores. J Urol. 2004;171:1478-80. 9. Castro HAS, Iared W, Shigueoka DC, et al. Contribuição da densidade do PSA para predizer o câncer da próstata em pacientes com valores de PSA entre 2,6 e 10,0 ng/ml. Radiol Bras. 2011;44:205-9. 10. Miller J, Perumalla C, Heap G. Complications of transrectal versus transperineal prostate biopsy. ANZ J Surg. 2005;75:48-50. 11. Rodríguez LV, Terris MK. Risks and complications of transrectal ultrasound guided prostate needle biopsy: a prospective study and review of the literature. J Urol. 1998;160(6 Pt 1):2115-20. 12. Rietbergen JB, Kruger AE, Kranse R, et al. Complications of transrectal ultrasound-guided systematic sextant biopsies of the prostate: evaluation of complication rates and risk factors within a population-based screening program. Urology. 1997;49:875-80. 13. Raaijmakers R, Kirkels WJ, Roobol MJ, et al. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology. 2002;60:826-30. 14. Peyromaure M, Ravery V, Messas A, et al. Pain and morbidity of an extensive prostate 10-biopsy protocol: a prospective study in 289 patients. J Urol. 2002;167:218-21. 15. Djavan B, Waldert M, Zlotta A, et al. Safety and morbidity of first and repeat transrectal ultra-sound guided prostate needle biopsies: results of a prospective European prostate cancer detection study. J Urol. 2001;166:856-60. 16. Aus G, Ahlgren G, Bergdahl S, et al. Infection after transrectal core biopsies of the prostate - risk factors and antibiotic prophylaxis. Br J Urol. 1996;77:851-5. 17. Crawford ED, Haynes AL Jr, Story MW, et al. Prevention of urinary tract infection and sepsis following transrectal prostatic biopsy. J Urol. 1982;127:449-51. 18. Lindert KA, Kabalin JN, Terris MK. Bacteremia and bacteriuria after transrectal ultrasound guided prostate biopsy. J Urol. 2000;164:76-80. 19. Aron M, Rajeev TP, Gupta NP. Antibiotic prophylaxis for transrectal needle biopsy of the prostate: a randomized controlled study. BJU Int. 2000;85:682-5. 20. Kapoor DA, Klimberg IW, Malek GH, et al. Single-dose oral ciprofloxacin versus placebo for prophylaxis during transrectal prostate biopsy. Urology. 1998;52:552-8. 21. Davis M, Sofer M, Kim SS, et al. The procedure of transrectal ultrasound guided biopsy of the prostate: a survey of patient preparation and biopsy technique. J Urol. 2002;167(2 Pt 1):566-70. 22. Lee SH, Chen SM, Ho CR, et al. Risk factors associated with transrectal ultrasound guided prostate needle biopsy in patients with prostate cancer. Chang Gung Med J. 2009;32:623-7. 23. Selius BA, Subedi R. Urinary retention in adults: diagnosis and initial management. Am Fam Physician. 2008;77:643-50. 1. MD, Resident, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 2. Full Professor, Head of Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 3. PhD, Collaborating Physician, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 4. Adjunct Professor, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 5. MSc, Chief of Coordination, Unit of Nonvascular Intervention, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. Mailing Address: Dr. Raphael Sandes Solha Rua Barão do Triunfo, 1220, ap. 14, Brooklin Paulista São Paulo, SP, Brazil, 04602-916 E-mail: r_solha@hotmail.com Received May 17, 2012. Accepted after revision December 21, 2012. 8 Study developed at Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554