Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Adriana Dias Barranhas1; Monica Silva Costa Janson Ney2; Marcelo Alves3; Alair Augusto Sarmet Moreira Damas dos Santos4; Marcelo Souto Nacif4 |
|
|
A male, 40-year-old patient entered the emergency department complaining of macroscopic hematuria. Previous history of repeated nephrolithiasis and computed tomography (CT) performed in other institution, demonstrating the presence of calculi without other specific findings.
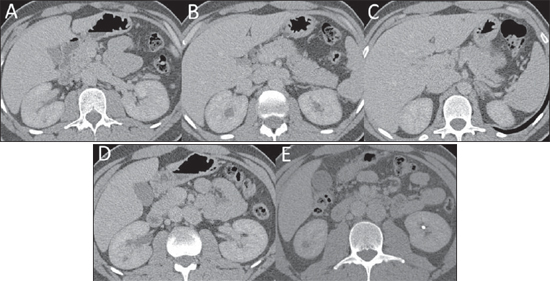
The patient was referred to undergo a new CT scan which demonstrated bilateral nephrolithiasis and mild dilatation of the calyceal system (Figure 1). Images description Figure 1. Computed tomography image acquired after intravenous contrast injection. A: Inferior vena cava at left, receiving the left renal vein. B: Inferior vena cava positioned from the left to the right anteriorly to the aorta. C: Inferior vena cava at right, after receiving the right renal vein. D: Right gonadal vein ectasia. E: Nephrolithiasis at left. Diagnosis: Left inferior vena cava with mild compression of the ureter, causing stasis and development of calculi. COMMENTS Abnormalities of the inferior vena cava (IVC) and its tributaries are known by anatomists since 1793(1). Location of the inferior vena cava at left has a prevalence of 0.2% to 0.5%, which may be underestimated, considering that such abnormality is frequently asymptomatic(2). It is a common imaging finding, but its clinical significance is taken into consideration in cases of confusion with para-aortic lymph nodes enlargement or with the left renal vein, which has occurred principally because the increasing utilization of minimally invasive diagnostic procedures. Non-invasive imaging methods are extremely important for the pre-procedural diagnosis, considering that iatrogenic hemorrhage may result from some clinical and therapeutic situations, particularly those involving laparoscopic manipulation or procedures performed without previous knowledge on such anatomical variant. Other important clinical situation occurs in transjugular insertion of IVC filter that may be very difficult to be performed in the presence of such a variant(4). The infrahepatic segment of the IVC develops between the sixth and eighth weeks of embryonic life, as a structure formed by anastomosis and partial, non simultaneous, resorption of three paired embryonic veins(5). The location of the IVC at left results from the regression of the right supracardinal vein with persistence of the left supracardinal vein. Characteristically, like in the present case, the left renal vein drains into the IVC at left which crosses the aorta anteriorly, joining the right renal vein to form the suprarenal segment of the IVC at right(5). Ultrasonography, CT or magnetic resonance imaging (MRI) can be utilized to evaluate the IVC, according to the method availability or contraindications for each patient. The ideal study phase for evaluating the IVC is at approximately 40-60 seconds after intravenous contrast injection, depending on the patient's clinical conditions. A possible imaging finding in cases of IVC location at left is higher attenuation of the right renal vein as compared with the left renal vein, as a function of the lower dilution of the venous return in lower limbs relatively without contrast agent(5). However, it is extremely important that an active search for such variants is undertaken, event at non-contrast enhanced CT scans performed for different abdominal causes, considering that probably such imaging scan will be the only method capable of making a diagnosis and preventing any type of iatrogenic condition in a future procedure. Some authors believe that IVC malformations by themselves are associated with deep venous thrombosis (DVT)(6), but the occurrence of malformations which remain asymptomatic over a lifetime is suggestive of a multifactorial cause for thrombotic disease in these patients. The incidence of IVC abnormalities in patients with DVT ranges between 5% and 7%, and is higher among young individuals and in cases of bilateral DVT(6). Anatomic variants of the IVC might not be visible at phlebography or at color echo Doppler, methods of first choice during an episode of DVT(6). In cases of DVT involving the iliac or femoral region, it is important that the vascular investigation is made by means of CT or MRI, particularly in young patients (@), to allow a more appropriate therapeutic definition. In the present case, the anatomical variant caused compression of the ureter, resulting in stasis and development of calculi (Figure 2). 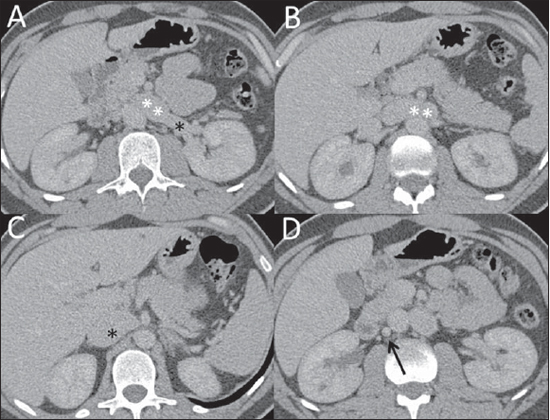 Figure 2. Computed tomography image acquired after intravenous contrast injection. A: Inferior vena cava located at left (white asterisks) receiving the left renal artery (black asterisk). B: Inferior vena cava positioned from the left to the right anteriorly to the aorta (asterisks). C: Inferior vena cava located at right, after receiving the right renal vein (asterisk). D: Ectatic right gonadal vein (arrow). FINAL CONSIDERATIONS The familiarity with this anatomical variant of IVC is important to avoid diagnostic errors resulting from confusion with masses or retroperitoneal lymph nodes enlargement. Even at non-contrast enhanced scans, the diagnosis is essential to avoid any iatrogenic condition or mistakes in interpretation, or even delayed diagnosis in the presence of vascular compression. Considering the greater association of such variant with DVT, vascular investigation with CT and MRI becomes imprescindible in cases of thrombosis in the iliac or femoral region. REFERENCES 1. Abernethy J. Account of two instances of uncommon formation in the viscera of the human body. Phil Trans R Soc Lond. 1793;83:59-66. 2. Onzi RR, Costa LF, Angnes RF, et al. Malformação de veia cava inferior e trombose venosa profunda: fator de risco de trombose venosa em jovens. J Vasc Bras. 2007;6:186-9. 3. Bass JE, Redwine MD, Kramer LA, et al. Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics. 2000;20:639-52. 4. Obernosterer A, Aschauer M, Schnedl W, et al. Anomalies of the inferior vena cava in patients with iliac venous thrombosis. Ann Intern Med. 2002; 136:37-41. 5. Kandpal H, Sharma R, Gamangatti S, et al. Imaging the inferior vena cava: a road less traveled. Radiographics. 2008;28:669-89. 6. Tiesenhausen K, Amann W, Thalhammer M, et al. Aplasia of the vena cava inferior as a cause for recurring thrombosis of the lower extremities and pelvic veins. Vasa. 1999;28:289-92. 1. Master, Universidade Federal do Rio de Janeiro (UFRJ), MD, Radiologist, Hospital de Clínicas de Niterói, Niterói, RJ, Brazil. 2. Head of the Service of Radiodiagnosis, Hospital Naval Marcílio Dias (HNMD), Rio de Janeiro, RJ, Brazil. 3. Head of the Department of Radiology, Hospital Naval Marcílio Dias (HNMD), Rio de Janeiro, RJ, Brazil. 4. PhDs, Professors, Department of Radiology, School of Medicine, Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil. Mailing Address: Dra. Adriana Dias Barranhas Travessa Olavo Bastos, 62, ap. 301, São Francisco Niterói, RJ, 24360-240, Brazi E-mail: diasbarranhas@gmail.com Study developed at Hospital Naval Marcílio Dias (HNMD), Rio de Janeiro, RJ, and at Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554