Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013
|
ORIGINAL ARTICLE
|
|
Temporal bone trauma and complications: computed tomography findings |
|
|
Autho(rs): Ana Maria Doffémond Costa1; Juliana Oggioni Gaiotti1; Caroline Laurita Batista Couto1; Renata Lopes Furletti Caldeira Diniz2; Emília Guerra Pinto Coelho Motta2; Natália Delage Gomes1 |
|
|
Keywords: Temporal bone trauma; Ossicular injuries; Ossicular trauma. |
|
|
Abstract: INTRODUCTION
Cranioencephalic trauma (CET) is one of the leading morbimortality causes in Brazil and in the world, most commonly occurring in the young adult age group(1). Most temporal bone fractures result from high-energy blunt head trauma, many times related to other skull fractures or to polytrauma. For such a reason, a multidisciplinary evaluation is generally required, including otolaryngology, radiology and neurosurgery(2-4). Multidetector computed tomography plays a fundamental role in the assessment of such patients. According to a study published by Morgado et al.(5), in spite of most CET cases (82.4%) being classified as mild, tomographic changes were observed in approximately 80% of their patients. Such data highlight the importance of skull computed tomography as the method of choice in the initial assessment of such patients(1), in addition to the Glasgow Coma Scale and information regarding the accident(5). Multiplanar reconstructions allow detailed evaluation of the base of the skull, temporal anatomy as well as the extent of injuries involving specific structures(3,4,6). Currently, in addition to representing the imaging study of choice for the diagnosis and prognosis in cases of CET, computed tomography also plays an important role in the follow-up of injuries(5). The relationship between types of injuries demonstrated by computed tomography, types of CET (severity of the injury) and prognosis has been described by several authors in the literature, all of them demonstrating approximately the same relationship: the more severe the CET, the more numerous and more severe are the findings at computed tomography(5). Fractures and displacements of the ossicular chain in the middle ear represent one of the main complications of temporal bone injuries, the latter being frequently observed in cases of severe CET, and for that reason, are more deeply approached in the present study(2,6-8). The radiologist must be familiar with the possible trauma mechanisms and with the temporal anatomy, allowing the proper classification of fracture types in order to predict possible associated complications and to guide the appropriate treatment. CLASSIFICATION OF TEMPORAL FRACTURES AND TRAUMA MECHANISMS The classification of temporal bone fractures is useful in the prediction of complications associated with the trauma, thus providing guidance for the management and treatment of the patient(2,4,6). It is very important that the radiologist accurately describes the affected anatomic structures, particularly in cases where the injury may cause functional compromising. The traditional classification indicates the relationship between the fracture line and the longer axis of the petrous portion of the temporal bone(3,4). Oblique fractures, also called mixed or complex fractures, are the most common types, followed by longitudinal and transverse fractures(4). As regards trauma mechanisms and main complications of each type of temporal fracture, they may be summarized as follows: a) longitudinal fractures generally occur in cases of temporoparietal trauma, commonly affecting the extra labyrinthine segment, and presenting as main complications ossicular lesion and hemotympanum(3); b) on the other hand, transverse fractures generally occur in cases of frontal/occipital traumas, with translabyrinthine involvement, whose main complication is facial nerve weakness(3). Longitudinal fractures Such fractures are characterized by a line of force running lateral to medial. In such cases, temporoparietal trauma is most frequently observed(3,4,7,9). At axial computed tomography, a radiolucent line parallel to the longest axis of the petrous pyramid is observed (Figure 1).  Figure 1. Longitudinal fracture. Axial computed tomography image showing temporal bone longitudinal fracture identified as a radiolucent line parallel to the largest axis of the petrous pyramid. The most common complications of longitudinal fractures include ossicular injuries, tympanic membrane rupture and hemotympanum, with conductive hearing loss. Less commonly, the facial nerve may be affected(3). Transverse fractures Such fractures typically result from trauma either in the frontal or occipital regions, as well as in the craniocervical junction, with a line of force running anterior to posterior(3,4). The fracture line is perpendicular to the longest axis of the petrous pyramid (Figure 2). 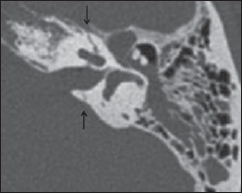 Figure 2. Transverse fracture. Axial computed tomography image demonstrating temporal bone transverse, translabyrinthine fracture, seen as a radiolucent line perpendicular to the largest axis of the petrous pyramid. The sensorineural hearing loss is more common in patients with transverse fracture, sometimes secondarily to transection of the cochlear nerve, injuries to labyrinthine structures or to the stapes footplate, which results in labyrinthine fistula(10,11). Facial nerve paralysis is also more frequently observed in this type of fracture. Oblique fractures Such fractures include both elements, longitudinal and transverse (Figure 3), with frequent involvement of the otic capsule, which causes sensorineural hearing loss(3,4,9). In the event of ossicular injury, it may also cause conductive hearing loss. 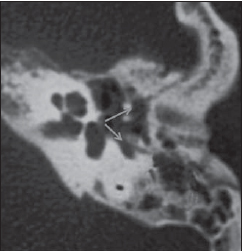 Figure 3. Oblique fracture. Axial computed tomography image demonstrating longitudinal and transverse elements of the oblique fracture. IDENTIFICATION OF THE AFFECTED STRUCTURES: INJURIES TO THE OSSICULAR CHAIN Ossicular injuries represent a frequent complication from temporal trauma, possibly leading to interruption of different segments of the ossicular chain. In cases of patients who suffered temporal trauma, conductive hearing loss is the most common consequence of this type of injury, with dislocations being more frequently observed than ossicular fractures(3,7,10,12). There are five types of dislocations as follows: incudostapedial joint dislocation; malleoincudal joint dislocation; dislocation of the incus; dislocation of the malleoincudal complex; stapediovestibular dislocation(7,8,12,13). Fractures of the malleus, incus and stapes are uncommonly observed. High resolution computed tomography is the method of choice to evaluate ossicular trauma. Axial images allow a better evaluation of ossicular continuity. Coronal and oblique reconstructions may be used in the evaluation of the long process of the incus as well as its relationship with the malleus, as it can be seen below(3). Incudostapedial joint dislocation Incudostapedial dislocation is the most common post-traumatic abnormality of the ossicular chain, on account of the tenuous suspension of the incus between the firmly attached malleus and the stapes(3,8,12). On axial or oblique reconstructions, the interruption of such joint is seen as an enlarged space between the head of the stapes and the long process of the incus (Figure 4). 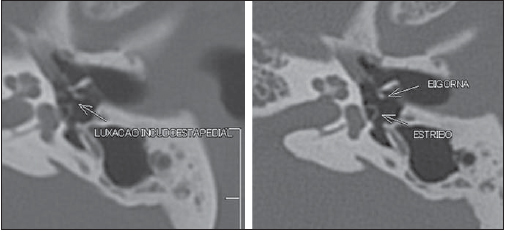 Figure 4. Incudostapedial dislocation. Axial computed tomography image of the incudostapedial joint reveals separation between the incus lenticular process and the stapes head. Malleoincudal joint dislocation The malleoincudal joint is protected by the epitympanic recess. The malleus is the most firmly attached ossicle, and such an attachment is guaranteed by the tympanic membrane, by the anterior and lateral ligaments of the malleus and by the tensor muscle and tendon of the tympanic membrane. Usually, in cases of trauma, the malleus remains at its position or moves slightly. On the other hand, the incus, the heaviest ossicle, is not attached to any muscle structure and its ligaments are rather weak(3,12,13). The malleoincudal dislocation is clearer seen at axial computed tomography images, which show the dislocation of the malleus head from the body/long process of the incus (Figure 5). 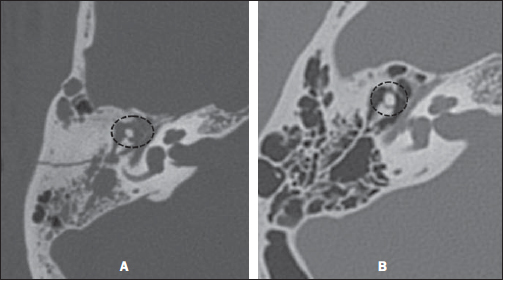 Figure 5. Malleoincudal dislocation. Axial Computed tomography image demonstrates dislocation of the malleoincudal joint (A) in a comparative analysis with a normal joint (B). Reconstructions are important to highlight the position of the ossicles in those cases of significant dislocation. Dislocation of the incus The incus is relatively vulnerable to traumatic dislocations, on account of its weakly anchored position between the firmly attached malleus and stapes(3,12). After severe skull trauma, the incus may suffer dislocation on account of its inertia(14). Penetrating traumas through the external ear canal may also cause dislocation of the incus. The incus may remain in the epitympanic recess, dislocate to the most inferior portion of the tympanic cavity or of the external ear canal, or even be destroyed(13). A thorough evaluation by means of computed tomography in axial and coronal planes of the middle ear and external acoustic meatus is necessary to identify the exact position of the incus in relation to the malleus and the stapes (Figure 6). 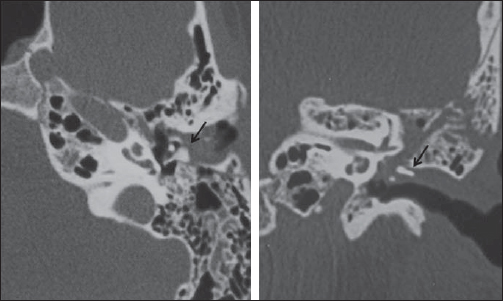 Figure 6. Incus dislocation. Axial and coronal computed tomography images demonstrating incus dislocation with rotation and displacement of the ossicle toward the external ear canal (arrows). Stapediovestibular dislocation The annular stapedial ligament firmly attaches the stapes to the oval window, and for this reason the stapediovestibular dislocation is not common(7,14). Penetrating injuries through the external ear canal (manipulation with cotton swabs) can dislocate the stapes through the oval window into the vestibulum (internal dislocation) (Figure 7). 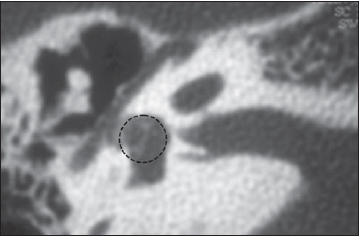 Figure 7. Stapedial dislocation. The stapes has been displaced into the vestibulum. Ossicular fractures Among the ossicular fractures, the most relevant one fracture of the stapes arch, which occurs secondarily to its torsion(8,14). Fracture of the stapes footplate occurs mainly in cases of transverse fractures (translabyrinthine fractures) crossing the oval window. Footplate fracture (either with or without fragments displacement) may cause perilymphatic fistula with pneumolabyrinth(14). OTHER TYPES OF INJURIES Labyrinthine fractures Generally related to transverse fractures with sensorineural hearing loss(11), such fractures are followed by pneumolabyrinth(12,14) and perilymphatic fistulas. Perilymphatic fistulas may also cause vertigo, and occur on account of injury to the otic capsule(9,15) (Figures 8 and 9). 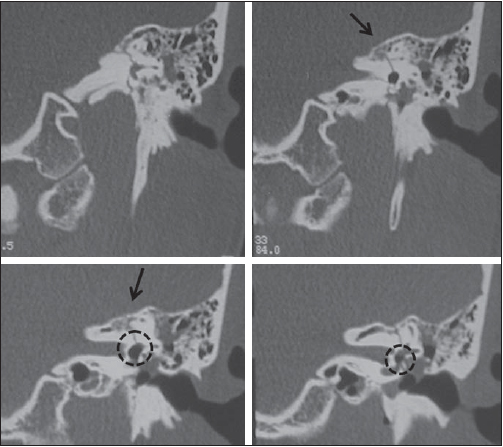 Figure 8. Labyrinthine fractures. Coronal computed tomography image shows transverse fracture extendinginto the osseous labyrinth (arrow) and with pneumovestibule (circle). 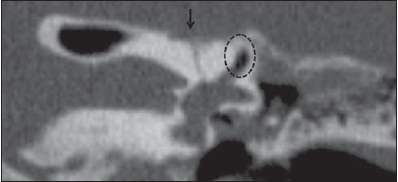 Figure 9. Labyrinthine fractures. Coronal computed tomography reveals translabyrinthine transverse fracture (arrow) Pneumolabyrinth (circle) and fluid inside the middle ear (perilymphatic fistula) are highlighted. Dural fistulas Generally related to injuries of the tegmen tympani or of the sphenoid sinuses walls, dural fistulas evolve with otoliquorrhea or rhinoliquorrhea. Such lesions should not be neglected, because of the risk for meningitis(7,12,15) (Figure 10). 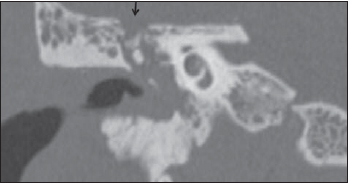 Figure 10. Dural fistulas. Coronal computed tomography image demonstrating tegmen tympani rupture (arrow). Facial paralysis The facial nerve pathway may be evaluated along its entire extent in the axial plane, with oblique reconstructions being of great relevance to analyze the integrity of the mastoid and tympanic segments. The facial nerve is affected in up to 7% of patients with temporal fracture. Most injuries occur in the labyrinthine portion, in the region of the geniculate ganglion, and manifest as nerve contusion, edema and hematoma of the neural sheath and partial or complete nerve transection(7,9,15). Immediate-onset post-traumatic paralysis frequently indicates presence of nerve transection or compression by a bone fragment (Figure 11). 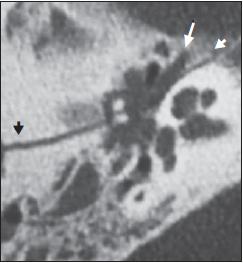 Figure 11. Facial paralysis. Axial computed tomography image showing longitudinal fracture (arrow heads) crossing the tympanic segment of the facial nerve (arrow). Carotid canal The petrous portion of the temporal bone includes the petrous segment of the internal carotid artery, which is located in the carotid canal, medially to the styloid process and anteriorly to the jugular fossa. The carotid canal thoroughly evaluated in the axial plane. Patients with fractures extending to the carotid canal present increased risk for injuries to the internal carotid artery. Associated complications include arterial dissection, pseudoaneurysm, complete transection, occlusion and arteriovenous fistulas(7,15) (Figure 12). 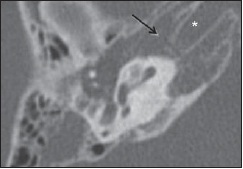 Figure 12. Carotid canal. Axial computed tomography image showing transverse fracture (arrows) crossing the carotid canal (asterisk). CONCLUSION Computed tomography plays a fundamental role in the initial evaluation of polytrauma patients, as it is capable of identifying injuries to important structures which may lead to severe complications such as conductive or sensorineural hearing loss, dizziness and balance disorders, perilymphatic fistulas, facial nerve paralysis, vascular injuries, among others(3). Investigations by means of computed tomography also allow the radiologist to classify temporal fractures and to predict such possible complications, providing guidance for treatment. The temporal bone anatomy is rather complex, with several critical structures associated to each other(3,7,8,11). It is important for the radiologist to be familiar with such anatomy and by team-working with other specialists, such as otolaryngologists and neurosurgeons, allowing the appropriate management of cases of temporal bone trauma, thus reducing the risk for severe sequels in such patients. REFERENCES 1. Gasparetto EL. Tomografia computadorizada no traumatismo cranioencefálico [editorial]. Radiol Bras. 2011;44(2):vii. 2. Dal Secchi MM, Moraes JFS, Castro FB. Fratura de osso temporal em pacientes com traumatismo crânio-encefálico. Arquivos Int Otorrinolaringol. 2012;16:62-6. 3. Little SC, Kesser BW. Radiographic classification of temporal bone fractures: clinical predictability using a new system. Arch Otolaryngol Head Neck Surg. 2006;132:1300-4. 4. Saraiya PV, Aygun N. Temporal bone fractures. Emerg Radiol. 2009;16:255-65. 5. Morgado FL, Rossi LA. Correlação entre a escala de coma de Glasgow e os achados de imagem de tomografia computadorizada em pacientes vítimas de traumatismo cranioencefálico. Radiol Bras. 2011;44:35-41. 6. Lasak JM, Van Ess MJ, Kryzer TC, et al. Penetrating middle ear trauma through the external auditory canal. Otolaryngol Head Neck Surg. 2004;131:P92. 7. Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18:188-97. 8. Hasso AN, Ledington JA. Traumatic injuries of the temporal bone. Otolaryngol Clin North Am. 1988;21:295-316. 9. Dahiya R, Keller JD, Litofsky NS, et al. Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 1999;47:1079-83. 10. Swartz JD, Berger AS, Zwillenberg S, et al. Ossicular erosions in the dry ear: CT diagnosis. Radiology. 1987;163:763-5. 11. Swartz JD, Swartz NG, Korsvik H, et al. Computerized tomographic evaluation of the middle ear and mastoid for posttraumatic hearing loss. Ann Otol Rhinol Laryngol. 1985;94:263-6. 12. Cvorovic L, Jovanovic MB, Markovic M, et al. Management of complication from temporal bone fractures. Eur Arch Otorhinolaryngol. 2012;269:399-403. 13. Lourenco MT, Yeakley JW, Ghorayeb BY. The "Y" sign of lateral dislocation of the incus. Am J Otol. 1995;16:387-92. 14. Mafee MF, Valvassori GE, Kumar A, et al. Pneumolabyrinth: a new radiologic sign for fracture of the stapes footplate. Am J Otol. 1984;5:374-5. 15. Zayas JO, Feliciano YZ, Hadley CR, et al. Temporal bone trauma and the role of multidetector CT in the emergency department. Radiographics. 2011;31:1741-55. 1. MDs, Radiology and Imaging Diagnosis Trainees at Hospital Mater Dei, Belo Horizonte, MG, Brazil. 2. MDs, Radiologists, Preceptors at Unit of Radiology and Imaging Diagnosis, Hospital Mater Dei - Mater Imagem, Belo Horizonte, MG, Brazil. Mailing Address: Dra. Ana Maria Doffémond Costa Rua Platina, 56, ap. 302, Prado Belo Horizonte, MG, Brazil, 30411-092 E-mail: anadoffemond@yahoo.com.br Received June 30, 2012. Accepted after revision October 9, 2012. * Study developed at Unit of Radiology and Imaging Diagnosis, Hospital Mater Dei - Mater Imagem, Belo Horizonte, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554