INTRODUCTION
Central nervous system (CNS) lymphoma may present as a primary disease, however, it is more frequently found as a secondary disease. In a survey carried out in the USA between 2004 and 2008, lymphomas represented 2.3% of CNS primary tumors, most commonly found in men (1.38:1) and after the sixth decade of life(1). Typically, primary CNS lymphoma (PCNSL) is a B-cell non-Hodgkin's lymphoma but occasionally it may manifest as T-cell lymphoma, intravascular lymphomatosis or Hodgkin's lymphoma(2,3). On the other hand, in cases where the CNS involvement is not primary, CNS metastasis occurs in 2% to 15% of non-Hodgkin's
The early diagnosis of CNS lymphomas depends upon the understanding by radiologists of their varied presentations at magnetic resonance imaging (MRI). The present study reviews images obtained over the past 13 years in the Radiology Service at Hospital das Clínicas - Universidade Estadual de Campinas (Unicamp). The diagnoses were duly confirmed by histopathology, and the project was approved by Committee for Ethics in Research of the School of Medical Sciences of Unicamp.
RADIOLOGICAL CHARACTERISTICS
As regards the location of lesions, supratentorial region is generally more frequently affected than the infratentorial region. In cases of deep intra-axial lesions, striatocapsular regions and the corpus callosum are affected with a certain frequency. However, lesions may be observed in other sites such as the hypophysis, cavernous sinus, hypothalamus, pineal gland, and posterior fossa. Periventricular or superficial lesions, in contact with the meningeal or ventricular surfaces (intraventricular lesions for example), are commonly found(2-7).
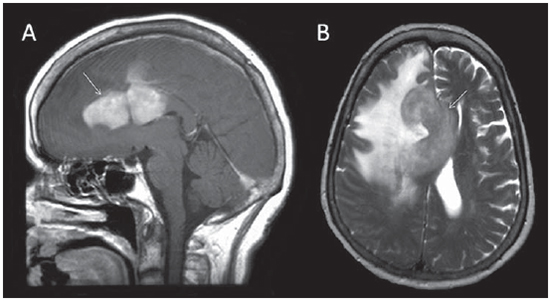
In immunocompetent patients, CNS lymphoma tends to present as a single and solid large mass, with tumor cells which tend to be monoclonal. Often, the patient's age at the disease onset is higher and the survival is longer. Such single lesions, with high cellularity and generally without necrosis, present preponderantly hyposignal (or isosignal) on T2-weighted and isosignal on T1-weighted images, and demonstrate intense enhancement after intravenous injection of paramagnetic contrast agent.
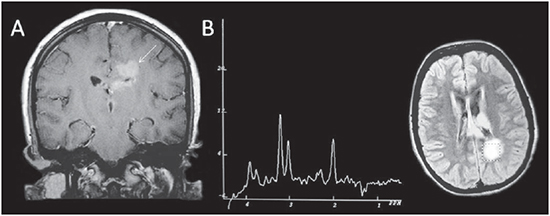
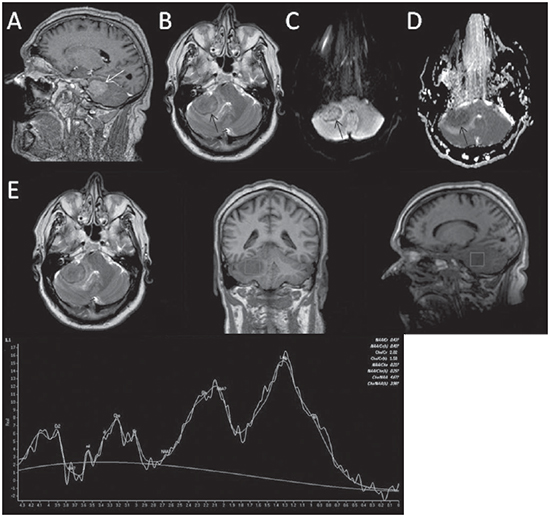
The presence of this kind of lesion involving the corpus callosum is highly suggestive of lymphoma (Figure 1)(5). Additionally, not only the image but also the frequent subependimal dissemination can demonstrate the common perilesional edema which occurs in varied degrees and the mass effect (Figure 2A)(4-7).
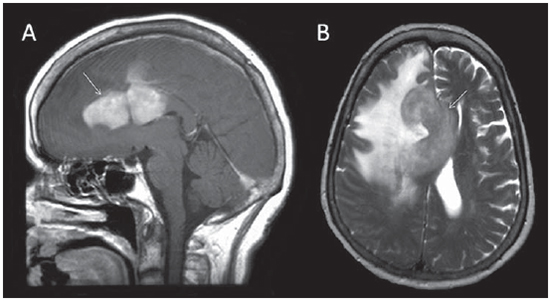
Figure 1. Female, 53-year-old patient. Contrast-enhanced MRI: sagittal T1weighted image (A) and axial T2-weighted image (B) shows a solitary lesion in the corpus callosum and cingulate gyrus, with diffuse and homogeneous contrast-enhancement. On the T2-weighted image, the lesion is hypointense. Marked perilesional edema is observed. The CNS involvement was primary in this case and the anatomopathological analysis indicated the presence of a large B-cell non-Hodgkin's lymphoma (centroblastic).
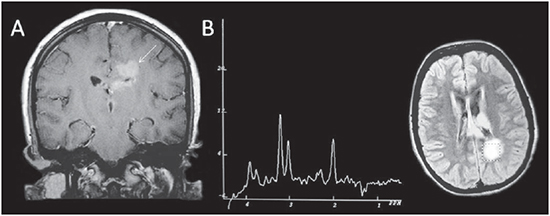
Figure 2. Female, 19-year-old patient. Post-contrast coronal MRI T1-weighted image (A) reveals presence of a left periventricular lesion, with homogeneous contrast uptake. Subependymal dissemination is observed. Spectroscopy with ET of 135 ms (B) demonstrates increased choline levels, decreased NAA levels and inverted lactate peak (double peak of 1.3 ppm). In this case, CNS was the primary site of involvement by lymphoma.
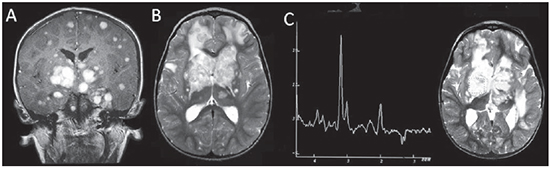
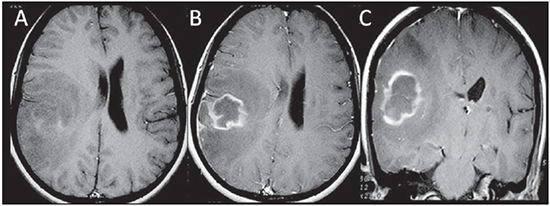
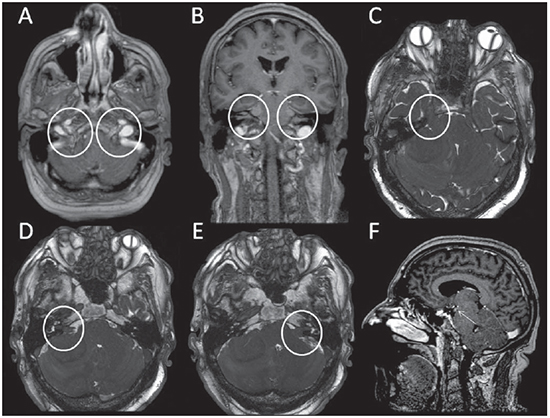
Several significant similarities may be found between patients with acquired immunodeficiency syndrome and patients with other forms of immunosuppression. In such cases, there is a higher probability of PCNSLs presenting as multifocal lesions (Figures 3A and 3B) with necrosis (Figures 4A and 4B) and differentiation between them and toxoplasmosis may be difficult.
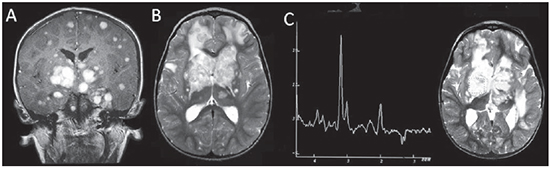
Figure 3. Male, 3-year-old patient. Post-contrast coronal MRI T1-weighted image (A) shows the presence of centroencephalic, cortical and subcortical lesions with nodular homogeneous contrast enhancement. Subependymal dissemination is observed. On the axial T2 weighted image (B) the lesions present isointense signal, some of them with a hyperintense center. Also, moderate perilesional edema is observed. At spectroscopy with ET of 135 ms (C), increased choline, decreased NAA levels and inverted lactate peak are observed.
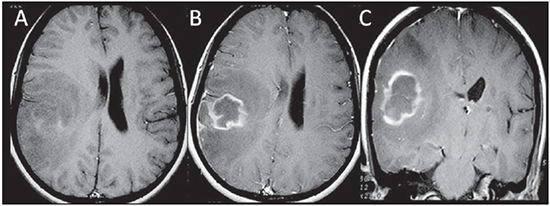
Figure 4. Female, 32-year-old, HIV positive patient. Axial T1-weighted image (A) demonstrates right parietotemporal lesion with high signal components (hemorrhage). B, C: Post-contrast axial and coronal T1weighted images demonstrate peripheral contrast uptake and moderate perilesional vasogenic edema. Central non-enhancing component corresponds to necrosis.
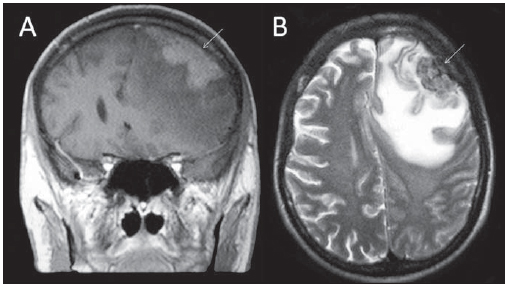
In regard to contrast-enhancement, several series have demonstrated that its absence can be considered as being rare in CNS lymphomas (Figure 5)(5,6).
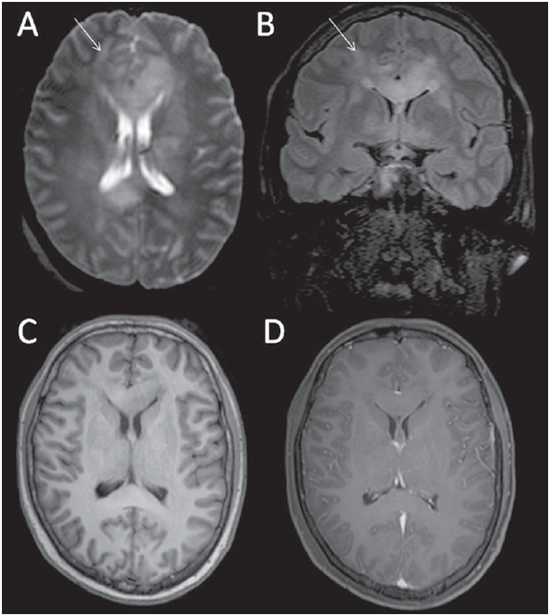
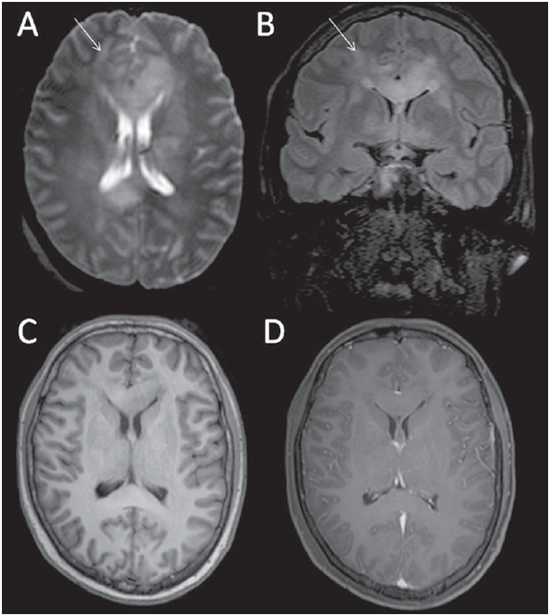
Figure 5. Male, 30-year-old patient. Images demonstrate an infiltrating deep white matter lesion which crosses medline and has variable signal intensity with an hypointense component on T2-weighted image (A,B - arrows), centered in the knee and splenium of the corpus callosum. Coronal FLAIR image (B) demonstrates hypersignal predominance. Axial T1-weighted images before (C) and after gadolinium injection (D) shows no contrast enhancement. Non-Hodgkin's lymphoma with peripheral B cells of high histologic grade and high proliferative index, compatible with diffuse large B cell lymphoma. Secondary CNS lymphoma (primary testicular involvement).
Pachy- or leptomeningeal involvement is more commonly found in secondary lymphomas or in immunocompromised patients. Additionally, appearance of dural/ pachymeningeal lesions may be similar to that of meningiomas (Figures 6 and 7)(4). Secondary CNS involvement by non Hodgkin's lymphoma generally occurs by leptomeningeal infiltration (found in up to two thirds of cases) and infiltration of perivascular spaces resulting in parenchymal lesions (observed in one third of cases - Figures 8 and 9)(2,3). Lesions affecting cranial nerves are relatively rare and may be solitary or multiple (Figure 10)(3,4,8). On the other hand, in Hodgkin's lymphoma, primary CNS involvement is rare and secondary involvement represents a late manifestation of disseminated disease (Figure 11).
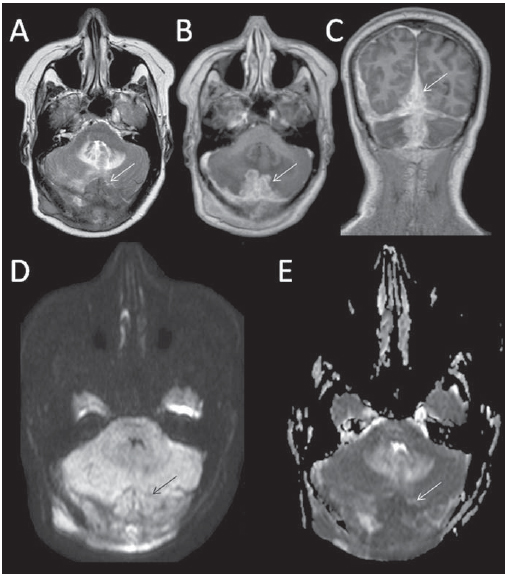
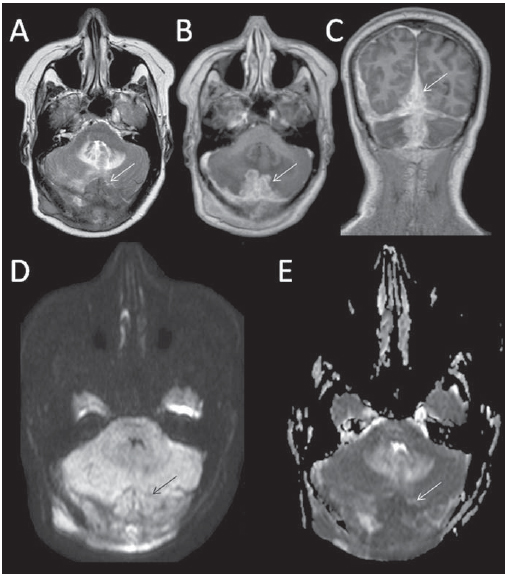
Figure 6. Female, 52-year-old patient. Images show diffuse supra and infratentorial dural (pachymeningeal) thickening at median right region, with hyposignal on T2-weighted image, homogeneous contrast-enhancement (C), hypersignal on diffusion-weighted image (D) and ADC map hyposignal - restricted diffusion (E). High-histologic-grade B immunophenotype non-Hodgkin's lymphoma.
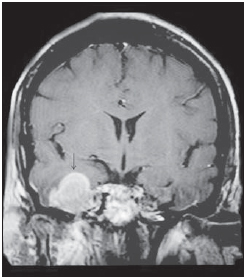
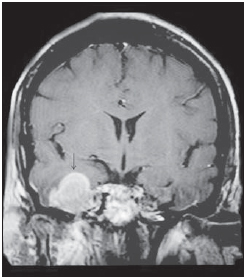
Figure 7. Female, 42-year-old patient. Contrast-enhanced, coronal MRI T1-weighted sequence presents a homogeneously enhanced solitary, extra-axial lesion in the right temporal fossa. Previously to the intracranial involvement, chronic sinusitis was present, whose cause was later identified by means of biopsy of the right maxillary sinus, as diffuse large B-cell non-Hodgkin's lymphoma.
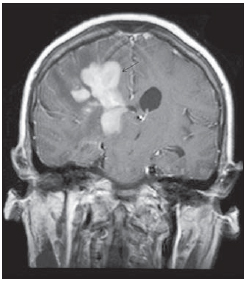
Figure 8. Female, 57-year-old patient. Coronal contrast-enhanced T1-weighted image (A) reveals presence of an intra-axial compact lesion affecting subcortical and deep white matter at right frontal lobe also compromising homolateral centroencephalic structures. The contrast-enhancement is homogeneous. Marked perilesional edema is observed. Primary bronchial involvement. Anatomopathological report of chest biopsy revealed large B-cell non-Hodgkin's lymphoma with Lambda light chains restriction in the bronchial mucosa. Secondary CNS involvement.
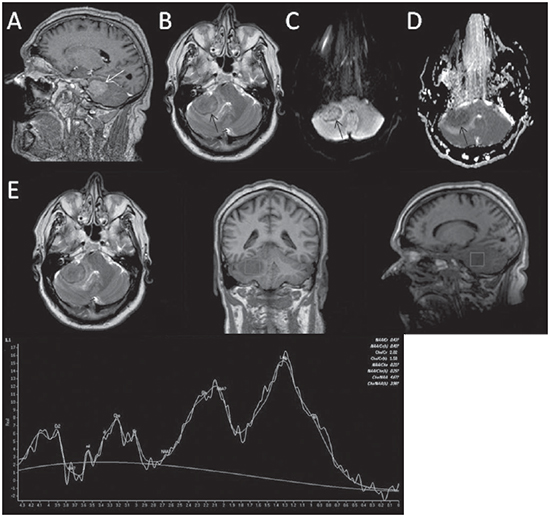
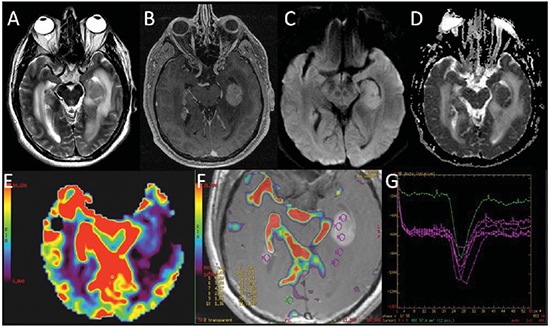
Figure 9. Male, 59-year-old patient. Fine post-gadolinium sagittal T1weighted image (A) demonstrates a right cerebellar hemispheric mass with intense contrast enhancement. On axial T2-weighted image (B) this lesion and homolateral middle cerebellar peduncle are observed with hyposignal. Diffusion-weighted image hypersignal (C) and ADC map hyposignal (D) characterizes restricted diffusion. Proton spectroscopy (E) with (short) ET of 30 ms reveals significant peak at 1.3 ppm (lipids/lactate) and decreased NAA level (2.0 ppm). B-cell Non-Hodgkin's lymphoma, secondary CNS involvement.
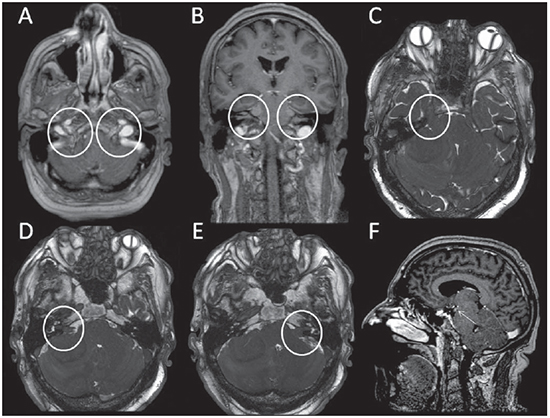
Figure 10. Same case as on Figure 9. Post-contrast axial T1-weighted image (A) demonstrates thickening and enhancement of the cranial nerve XI, bilaterally. Post-contrast coronal T1-weighted image (B) shows bilateral thickening and homogeneous enhancement of the cranial nerves V and VII-VIII are observed. Axial 3D CIS image demonstrates bilateral thickening of the cranial nerves V (C) and VII/VIII (D,E). Post-contrast sagittal T1-weighted image (F) demonstrates enhancement and thickening of the III cranial nerv.
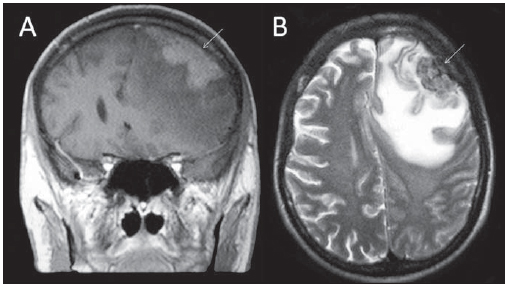
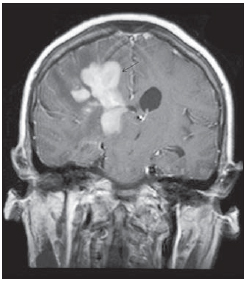
Figure 11. Male, 22-year-old patient. Coronal T1-weighted image (A) demonstrates frontal left extraaxial lesion with diffuse contrast-enhancement. This lesion is hypointense on axial T2-weighted image (B). Marked edema is observed. The extension to CNS was secondary to Hodgkin's disease/ type II nodular sclerosis diagnosed by means of cervical lymph node biopsy.
Proton magnetic resonance spectroscopy provides graphs which allow the analysis of specific tumor tissue metabolites, particularly in cases of parenchymal lesions. With this complementary method, it is possible to evaluate the levels of choline (peak ant 3.2 ppm), which marks cell membranes biosynthesis; N-acetylaspartate (NAA) (2.0 ppm), related to neuronal and axonal number and viability; creatine (3.02 and 4.0 ppm), utilized as a reference for its stability and a marker of oxidative phosphorylation of normal brain metabolism; lactate (1.3 ppm), related to anaerobic metabolism observed in anaerobiosis; lipids (usually between 0.9 and 1.3 ppm), related to necrosis(9). In CNS lymphomas, it is common to observe a pattern of increased choline levels, decreased NAA, increased lipids (moreover in the solid component without necrosis, an information that helps the differential diagnosis with glial lesions, in which such peak is usually observed in the necrotic component) (Figures 2B, 3C, 4C and 9E). It has been suggested that spectroscopy might be useful in differentiation between lymphoma, glioblastoma multiforme and metastases(10). It is important to observe that with echo time of 135144 ms, lactate is characterized by a double peak inverted below baseline. However this peak can be demonstrated at approximately 1.3 ppm above baseline with short echo time (30 or 35 ms) and with very high echo time (270 or 288 ms) lipids are suppressed and lactate is seen as a double peak above the baseline(4,5,9).
DIFFUSION
Diffusion-weighted MR images measure the apparent diffusion coefficient (ADC) which is inversely proportional to cell density, presumably resulting from the tortuosity of the interstitial space and consequential limitation of water movement. Although not always observable, CNS lymphoma tends to present a low ADC value at diffusion-weighted MRI because of its high cellularity, characteristically presenting restriction in those lesions without necrosis (Figures 6D, 6E, 9C and 9D)(2,5,10).
PERFUSION
Perfusion-weighted MRI techniques evaluate the microcirculation allowing the calculation of physical parameters such as cerebral blood volume (CBV), cerebral blood flow, and mean transit time. Typically, lymphomatous lesions present low CBV (Figure 12). The maximum relative CBV measured in the tumor and its relationship with the contralateral parenchyma is low as compared with that of other brain tumors(2).
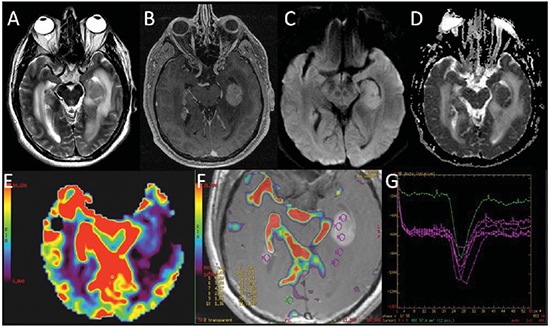
Figure 12. Male, 63-year-old patient. Nodular lesion located at left mesial temporal region, with isosignal on T2-weighted image (A), marked contrast-enhancement (B), hypersignal on DWI (C) and hyposignal on ADC map (D), characterizing diffusion restriction. The CBV map (D) does not demonstrate increased perfusion characterized by the quantitative analysis in form of curves (E,F). B image also demonstrates contrast-enhancement foci on the surface of the ependymal lining of right temporal horn, characterizing cerebrospinal fluid dissemination. (Case kindly assigned by Dr. Cassio Iwakura, from Hospital Vera Cruz, Campinas, SP, Brazil).
CNS lymphomas may present with varied forms, however some findings can contribute to facilitate the differential diagnosis which includes gliomas, metastases, and inflammatory diseases. The finding of an expansile supratentorial solid lesion hypointense on T2-weighted images, with no signs of necrosis, lipids peak in the solid component, low perfusion and diffusion restriction, favors the possibility of such diagnosis.
REFERENCES
1. Central Brain Tumor Registry of the United States. CBTRUS Statistical Report: Primary brain and central nervous system tumors diagnosed in the United States in 2004-2008. Hinsdale, IL: Central Brain Tumor Registry of the United States; 2012.
2. Haldorsen IS, Espeland A, Larsson EM. Central nervous system lymphoma: characteristic findings on traditional and advanced imaging. AJNR Am J Neuroradiol. 2011;32:984-92.
3. Slone HW, Blake JJ, Shah R, et al. CT and MRI findings of intracranial lymphoma. AJR Am J Roentgenol. 2005;184:1679-85.
4. Besada C, Schvartzman P, Paganini L, et al. Neuroimágenes estructurales y funcionales en la caracterización del linfoma del SNC. Rev Argent Radiol. 2010;74:147-53.
5. Küker W, Nägele T, Korfel A, et al. Primary central nervous system lymphomas (PCNSL): MRI features at presentation in 100 patients. J Neurooncol. 2005;72:169-77.
6. Schwingel R, Reis F, Zanardi VA, et al. Central nervous system lymphoma: magnetic resonance imaging features at presentation. Arq Neuropsiquiatr. 2012;70:97-101.
7. Nacif MS, Jauregui GF, Mello RAF, et al. Linfoma adrenal primário bilateral com envolvimento do sistema nervoso central: relato de caso. Radiol Bras. 2005;38:235-8.
8. Garcia MM, Martins JCT. Avaliação por imagem das lesões isoladas do III par craniano. Radiol Bras. 2005;38:219-23.
9. Horská A, Barker PB. Imaging of brain tumors: MR spectroscopy and metabolic imaging. Neuroimaging Clin N Am. 2010;20:293-310.
10. Chawla S, Zhang Y, Wang S, et al. Proton magnetic resonance spectroscopy in differentiating glioblastomas from primary cerebral lymphomas and brain metastases. J Comput Assist Tomogr. 2010;34:836-41.
1. PhD, Teacher responsible for the Sector of Neuroradiology, Professor at Faculdade de Ciências Médicas da Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil.
2. Graduate Student of Medicine (6th year) at Faculdade de Ciências Médicas da Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil.
3. MD, Radiologist, Fellow of Neuroradiology, Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
Mailing Address:
Dr. Fabiano Reis
Faculdade de Ciências Médicas, Universidade Estadual de Campinas, Departamento de Radiologia
Rua Tessália Vieira de Camargo, 126, Cidade Universitária Zeferino Vaz
Caixa Postal: 6111. Campinas, SP, Brazil, 13083-887
E-mail: fabianoreis2@gmail.com
Received July 16, 2012.
Accepted after revision November 5, 2012.
* Study developed at Hospital das Clínicas da Faculdade de Ciências Médicas da Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil. Financial support: Fundação de Amparo à Pesquisa do Estado de São Paulo (Fapesp) - Process No. 2010/01939-0.
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013