Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 2 - Mar. / Apr. of 2013
Vol. 46 nº 2 - Mar. / Apr. of 2013
|
CASE REPORT
|
|
Post-traumatic pulmonary pseudocyst in a soccer player: a case report |
|
|
Autho(rs): Andre Nathan Costa1; Karina de Souza Giassi2; Guilherme Hipolito Bachion3; Andre Apanavicius4; Rafael Silva Musolino4; Ronaldo Adib Kairalla5 |
|
|
Keywords: Pulmonary pseudocyst; Post-traumatic pseudocyst; Post-traumatic pneumatoceles. |
|
|
Abstract: INTRODUCTION
Post-traumatic pseudocysts are cavitary lesions that develop in the lung parenchyma as a consequence of blunt thoracic trauma. In general, such lesions occur after traffic collision or fall from height, and usually develop in areas of pulmonary contusion ipsilateral to the trauma site. The present report describes a case of post-traumatic pulmonary pseudocyst contralateral to the trauma site in a young man after falling during a soccer match. CASE REPORT Male, 31-year-old former smoker, with no comorbidity. During a soccer match, the man suffered left thoracic trauma after own-height fall, presenting intense local pain, with partial symptoms relief after use of analgesics. Six hours following the trauma, the patient progressed to hemoptysis, with no other associated symptoms. The patient attended the emergency department, and clinical examination found ecchymosis at the lateral aspect of the left hemithorax. Chest and costal arches radiographic images were normal. The patient received symptomatic medications and persisted with episodes of hemoptysis for two days, returning for medical assistance. His condition remained unaltered at clinical examination. The patient underwent chest computed tomography which demonstrated a solitary cystic lesion measuring 2.5 cm and small air-fluid level located in the lower lobe of the right lung in association with subtle perilesional ground glass opacity (Figures 1 and 2).  Figure 1. Juxtadiaphragmatic cavitary lesion with small air-fluid level and subtle ground-glass opacities in the right lower lobe. 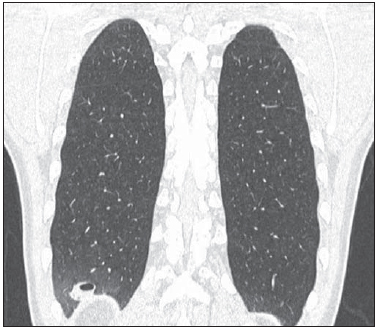 Figure 2. Coronal reformation of the small cavitary lesion demonstrating the extent of the adjacent ground-glass opacities. In the context of hemoptysis following an episode of blunt trauma in a patient with neither comorbidity nor any other previous systemic symptoms, the presence of a post-traumatic pseudocyst was considered as the main diagnostic hypothesis, so a conservative approach was adopted. Hemoptysis resolved at the fifth day following the trauma. Follow-up CT performed 30 days after the episode demonstrated a significant decrease in the cavitary lesion size and in the ground glass opacity. Only a small noncalcified nodule remained in the sub-pleural diaphragmatic region (Figures 3 and 4). The patient remains asymptomatic. 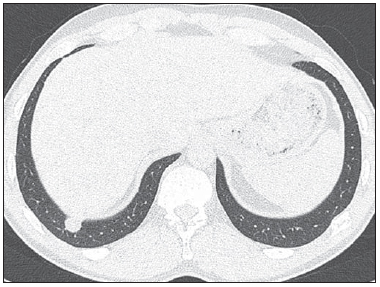 Figure 3. Follow-up CT 30 days after the trauma demonstrates the presence of a small lung nodule and disappearance of the perilesional ground-glass opacity 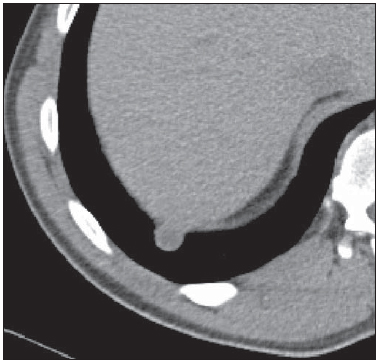 Figure 4. Follow-up CT scan demonstrated the presence of a small noncalcified nodule, an expected finding along the progression of this lesion. DISCUSSION The spectrum of lung parenchymal lesions occurring after blunt trauma ranges from simple contusions to complicated lacerations with pleural effusion and hydropneumothorax(1,2). Pseudocysts are included in the range of such complications, but represent a rare condition that is found in less than 3% of chest traumas(2,3). Characteristically, such condition is found in children and individuals under the age of 30. The term "pseudocyst" is justified by the presence of a thin wall of interstitial conjunctive tissue in association with the presence of macrophages and fibrous tissue, without epithelial lining or bronchial wall elements, which differentiates pseudocysts from true pulmonary cysts(2). The genesis of this lesion is explained by the greater pliability of the thoracic cage in the youngsters, allowing the transmission of the force caused by the sudden chest compression on the subjacent lung parenchyma. The fast compression and decompression cause small lacerations, resulting in small cavities which are filled with air and fluid. Each cavity tends to grow until a balance is achieved between the pressure of the adjacent parenchyma and the intracavitary pressure(3-6). Moreover, it is believed that the glottic closure at the moment of the trauma plays a relevant role in the development of such lesions, making that air remains in the contused parenchyma, triggering the mentioned lacerations(6). The differential diagnosis includes the spectrum of cavitary lesions of the lung parenchyma and is relatively extensive, involving from infections such as tuberculosis, mycosis, lung abscess, infectious pneumatocele, vasculitis and lung neoplasias, to congenital lesions such as bronchogenic cysts and adenomatoid cystic malformation. However, the diagnosis is based on the association of cavitary lesion with a clinical history of chest trauma. Computed tomography is the method of choice, since small pseudocysts may be masked at supine plain radiographs(7). The condition resolution observed at later imaging findings corroborates the traumatic nature of the entity. On average, such condition takes one to three months to resolve, but such time span may significantly increase in cases of pseudocysts measuring > 2 cm or pseudocysts with hematic content (7,8). The development of pseudocysts in areas of pulmonary contusion is considered as the usual pattern of the condition; on the other hand, reports on pseudocysts distant from the location of the original trauma are unusual(1,7). Additionally, such lesions develop in patients who had high-energy traumas. So the present case becomes peculiar as the mentioned pseudocyst developed in the lung contralateral to the site of a medium-intensity trauma, possibly because the greater pliability of the lower chest wall allowed the conduction of the kinetic force by the thoracic cage. The conservative treatment of the patient has allowed an appropriate clinical and radiological evolution compatible with the patterns described in the literature(1,2). REFERENCES 1. Yazkan R, Ozpolat B, Sahinalp S. Diagnosis and management of post-traumatic pulmonary pseudocyst. Respir Care. 2009;54:538-41. 2. Fagkrezos D, Giannila M, Maniatis P, et al. Posttraumatic pulmonary pseudocyst with hemopneumothorax following blunt chest trauma: a case report. J Med Case Rep. 2012;6:356. 3. Chon SH, Lee CB, Kim H, et al. Diagnosis and prognosis of traumatic pulmonary pseudocysts: a review of 12 cases. Eur J Cardiothorac Surg. 2006;29:819-23. 4. Watanabe M, Igarashi N, Naruke M, et al. Traumatic pulmonary pseudocyst with hemopneumothorax in a football player. Clin J Sport Med. 2005;15:41-3. 5. Monteiro AS, Addor G, Nigri DH, et al. Pseudocisto pulmonar traumático. J Bras Pneumol. 2005;31:80-2. 6. Tsitouridis I, Tsinoglou K, Tsandiridis C, et al. Traumatic pulmonary pseudocysts: CT findings. J Thorac Imaging. 2007;22:247-51. 7. De Dios JA, Paoletti L, Bandyopadhyay T. A 27- year-old man with pleuritic chest pain and hemoptysis after a rugby game. Chest. 2009;136:1165-7. 8. Melloni G, Cremona G, Ciriaco P, et al. Diagnosis and treatment of traumatic pulmonary pseudocysts. J Trauma. 2003;54:737-43. 1. PhD, MD, Pulmonologist, Hospital Sírio-Libanês and Instituto do Coração da Faculdade de Medicina da Universidade de São Paulo (InCor-FMUSP), São Paulo, SP, Brazil. 2. MD, Resident of Radiology and Imaging Diagnosis, Hospital Sírio-Libanês, São Paulo, SP, Brazil. 3. MD, Radiologist, Hospital Sírio-Libanês, São Paulo, SP, Brazil. 4. MDs, Pulmonologists, Hospital Sírio-Libanês, São Paulo, SP, Brazil. 5. PhD, Teacher at Faculdade de Medicina da Universidade de São Paulo (FMUSP), MD, Pulmonologist, Hospital Sírio-Libanês and Instituto do Coração da Faculdade de Medicina - Universidade de São Paulo (InCor-FMUSP), São Paulo, SP, Brazil. Mailing Address: Dra. Karina de Souza Giassi Instituto Sírio- Libanês de Ensino e Pesquisa Rua Coronel Nicolau dos Santos, 69, Bela Vista São Paulo, SP, Brazil, 01308-060 E-mail: ksgiassi@gmail.com Received September, 2012. Accepted after revision December 17, 2012. * Study developed at Hospital Sírio-Libanês, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554