Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 46 nº 1 - Jan. /Feb. of 2013
Vol. 46 nº 1 - Jan. /Feb. of 2013
|
ICONOGRAPHIC ESSAY
|
|
Magnetic resonance imaging in the differential diagnosis of infectious and inflammatory conus medullaris lesions |
|
|
Autho(rs): Gustavo Balthazar da Silveira Carvalho1; Gabriel Barbosa Sandim1; Luis Antônio Tobaru Tibana1; Franklin Freitas Tertulino1; Marcos Hideki Idagawa2; Nitamar Abdala3 |
|
|
Keywords: Magnetic resonance imaging; Myelitis; Transverse myelitis; Schistosomiasis. |
|
|
Abstract: INTRODUCTION
The conus medullaris is a site of frequent involvement by lesions of inflammatory or infectious etiology, generally established by hematogenous spread, but also disseminated through the cerebrospinal fluid or by meningeal or vertebral extension. Cases of neoplastic and vascular etiologies may present similar clinical signs. Many times, the clinical history and physical examination may be not sufficient to determine a specific cause because of interposition of symptoms(1). Magnetic resonance imaging (MRI) plays a relevant role in the diagnosis and differentiation as well as in the evolutive follow-up of such lesions. Such imaging method is highly sensitive and many times allows the differentiation with of other etiologies such as neoplasms and vascular diseases(1,2). However the specificity of this method is limited for differentiating between inflammatory etiologies. But some imaging findings in association with clinical and laboratory findings may lead to a more accurate diagnosis(1,3). The knowledge of such conditions and their presentations is fundamental for radiologists. The present study is aimed at approaching the findings related to conus medullaris lesions of inflammatory and infectious etiologies. For such purpose, the authors have selected images of individual cases in the files of their institution, demonstrating findings which may be useful to differentiate among the several etiologies. MEDULLARY SCHISTOSOMIASIS Schistosomiasis is endemic in Brazil. Its most frequent ectopic presentation - medullary schistosomiasis -, is considered the most common cause of non-traumatic and non-neoplastic myelitis(4). It is believed that the involvement of the central nervous system (CNS) occurs by means of retrograde flow through the Batson venous plexus, which is valveless. Schistosoma mansoni eggs are large and spiculated, impairing their progression through the CNS. For that reason, the conus medullaris is the most frequent presentation site and encephalic involvement is rare with this species(5). The clinical picture is that of acute/subacute myelopathy, characterized by pain and weakness of the lower limbs, loss of bowel and bladder sphincter control, besides changes in sensitive and sexual reflexes(4-6). MRI generally identifies a conus medullaris expansion, with hyposignal on T1-weighted, hypersignal on T2-weighted images and contrast-enhancement at the granuloma site. This finding may simulate a neoplastic lesion. A linear and nodular enhancement pattern with an "arborized" appearance is considered to be characteristic, and although it is not present in all cases, is a strong indication for the diagnosis of neuroschistosomiasis (Figure 1)(6). 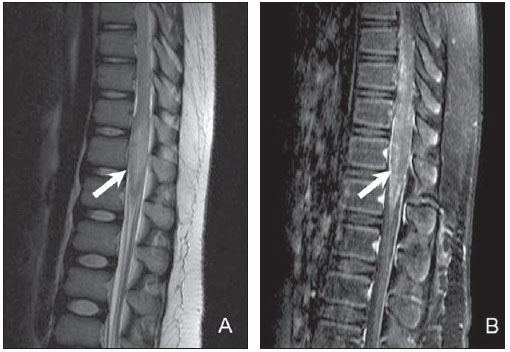 Figure 1. Twelve-year-old child diagnosed with neuroschistosomiasis. Sagittal MRI T2-weighted sequences (A), remarkable, central hypersignal with ill defined limits (arrow), besides volumetric increase of the conus medullaris obliterating the anterior and posterior CSF column. The contrast-enhanced T1-weighted sequence demonstrates heterogeneous enhancement with an "arborized" pattern (arrow in B). NEUROCYSTICERCOSIS Cysticercosis is the most common parasitic infection of the CNS. The intracranial presentation is most frequently found. Vertebral canal involvement is rare, representing only 2% to 5% of total neurocysticercosis cases. Leptomeningeal neurocysticercosis is the most common presentation, affecting the subarachnoid space by means of intracranial migration. Intramedullary involvement is rarely observed and occurs generally in the thoracic segment(5,7). In medullary neurocysticercosis, the clinical picture depends on the compression and edema mechanisms, as well as on the inflammatory response. It may be either asymptomatic or present signs and symptoms of myelopathy, including radiating pain, flaccid or spastic paresthesia, and neurogenic bladder(5,7,8). MRI is the method of choice for the study of medullary neurocysticercosis and shows cysts with similar signal to that of the cephalorachidian fluid, with hyposignal on T1-weighted and hypersignal on T2-weighted images (Figure 2). The scolex is represented by an eccentric nodule near the cyst wall, and its identification is diagnostic. In cysts with some degree of degeneration, peripheral postcontrast enhancement can be observed(7,8). 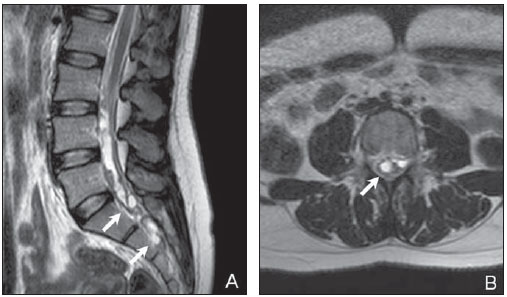 Figure 2. Sagittal (A) and axial (B) T2-weighted images showing multiple cyst-like images in close contact with the conus medullaris and cauda equina roots (arrows). Neurocysticercosis diagnosis was later confirmed. TUBERCULOSIS Involvement of the CNS occurs in approximately 10-15% of all infections by tuberculosis(9). Intramedullary tuberculoma is a rare finding, occurring in approximately 2% of cases of neurotuberculosis, with or without association with pulmonary involvement. The clinical presentation is generally subacute, with a variable picture of muscle weakness, paraparesis or quadriparesis. Constitutional symptoms such as fever and weight loss may not be present(9,10). At the disease onset, the inflammatory process with ill defined edema predominates. After formation of the granuloma, the lesions become more defined, generally with hyposignal on T1-weighted images and iso- to hypersignal on T2-weighted images. There is postcontrast enhancement, being such enhancement nodular and heterogeneous or annular and peripheral depending on the presence or not of caseous necrosis (Figure 3)(5,10). In immunocompromised patients, the finding of nodular lesions with nodular or peripheral enhancement may also be observed in cases of toxoplasmosis or fungal infections, but such conditions are extremely rare(11-13). 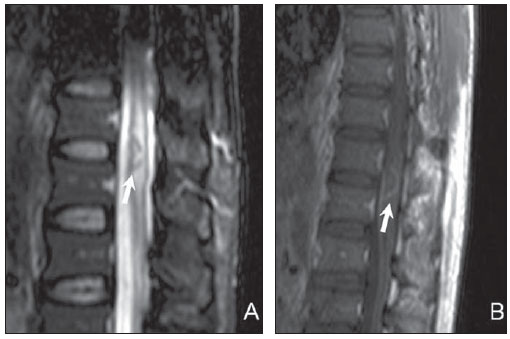 Figure 3. Immunocompromised patient diagnosed with neurotuberculosis. Sagittal MRI identify the presence of a nodular lesion with peripheral hyposignal and centrally located hypersignal on T2-weighted (arrow on A), besides adjacent edema presenting peripheral annular post-contrast enhancement (arrow on B). ACUTE TRANSVERSE MYELITIS Idiopathic acute transverse myelitis generally refers to a single phased, acute or subacute inflammatory process, without defined etiology, which develops with bilateral motor and sensitive deficit, sometimes with autonomic dysfunction. Approximately one third of the patients recover completely, one third remain with moderate sequels, and one third maintain severe dysfunction(5,14). Several conditions may present similar clinical signs, such as infectious, vascular and demyelinating diseases and actinic lesions. Therefore, the final diagnosis of idiopathic acute transverse myelitis depends on the investigation and ruling out of a possible identifiable etiology(1,14). The inclusion criteria for such diagnosis comprise motor/sensitive deficits or autonomic dysfunction attributed to the spinal cord, identifiable level of sensitivity, absence of compressive cause, medullary inflammatory process demonstrated by pleocytosis or increase in IgG in the cephalorachidian fluid, or post-gadolinium injection enhancement at MRI, with worsening peak in 4 hours to 21 days after the symptoms onset. The exclusion criteria are history of local radiation, evidence of collagen disease, syphilis, Lyme disease, HIV, HTLV and other viral etiologies, vascular diseases, lesions suggestive of multiple sclerosis or optic neuritis(15). Findings at MRI are variable, most frequently affecting thoracic segments, and least frequently the conus medullaris. A centrally located hypersignal is observed on T2-weighted images, with or without post-contrast enhancement (Figure 4). Increase in the spinal cord caliber, mimicking neoplastic lesion, may be observed(2,5,16). 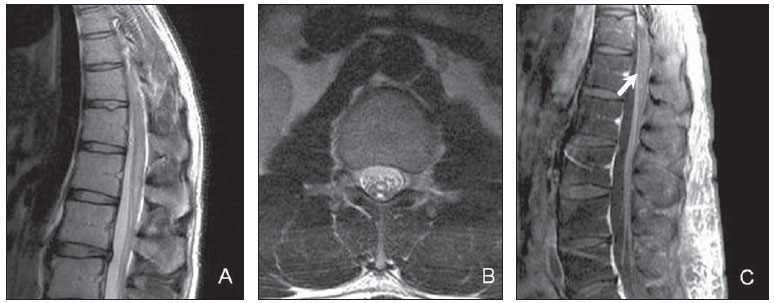 Figure 4. A 37-year-old patient with a history of sudden weakness in the lower limbs. In the conus medullaris region, central hypersignal is observed on T2weighted images, without significant increase in the spinal cord diameter on the sagittal (A) and axial (B) planes, besides heterogeneous and speckled post-contrast enhancement (arrow on C). Specific etiology was not confirmed, and the diagnosis of idiopathic transverse myelitis prevailed, with favorable clinical progression, with no sequel. In the suspicion of a myelinating etiology, further investigation should be undertaken in search of other lesions in the remaining medullary and intracranial segments, besides investigation for optical neuritis, in suspected cases. Approximately 90% of the patients with medullary lesions associated to multiple sclerosis present intracranial foci of demyelination(16). Usually, medullary lesions related to multiple sclerosis are peripherally located and with an extent of less than two vertebral bodies, while optic neuromyelitis presents lesions that extend for more than three vertebral bodies, with sharp hyposignal on T1weighted images and greater association with medullary atrophy(17). VIRAL MYELITIS Herpes virus, enterovirus and retrovirus (HIV) are some of the viral agents most frequently causing myelitis. The presentations are very similar to each other and the etiological diagnosis is only confirmed by means of laboratory tests. The clinical diagnosis of the infection by herpes zoster is many times difficult, as only one third of the patients present the typical skin lesion. Myelitis is a rare manifestation of the infection by herpes zoster and generally occurs after reactivation of a latent infection. In cases where a concomitant skin lesion is present, the medullary level corresponds to the affected dermatome(2,18). The presentation at MRI varies, ranging from single or multiple lesions, with or without postcontrast enhancement (Figure 5)(18). 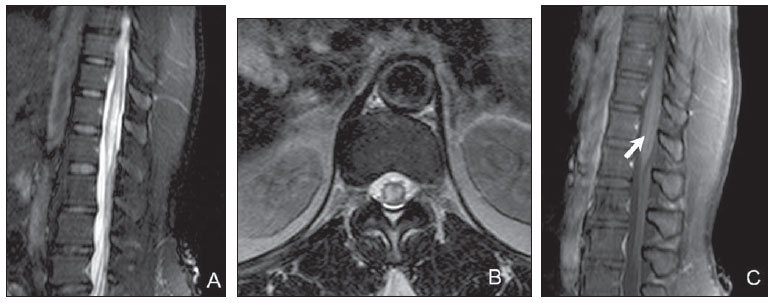 Figure 5. Patient with herpes-related myelitis, with no association with skin lesions. MRI demonstrates intense, central hypersignal on sagittal (A) and axial (B) T2-weighted sequence, with finely heterogeneous post-contrast enhancement (arrow on C). Myelitis related to HIV occurs in 5% to 8% of patients with acquired immunodeficiency syndrome, generally in association with a severe encephalic involvement(5). The HTLV-1 is associated to a progressive presentation of spastic paraparesis. The most affected medullary segment is the thoracic one and there may be association with medullary atrophy, besides lesions in the encephalic white matter(19). The infection by cytomegalovirus causes polyradiculomyelitis which frequently involves the conus medullaris and cauda equina roots, represented at MRI by contrast-enhanced, clumped and thickened nerve roots, a finding compatible with arachnoiditis(20). SARCOIDOSIS Neurosarcoidosis is a rare condition which occurs in approximately 5% of the cases of systemic sarcoidosis(21) and may affect any part of the CNS(22). Medullary involvement affection is rarely observed, and generally presents a subacute or chronic course. The symptoms are varied and generally are followed by pain, with possible occurrence of motor and sensitive deficits. The diagnosis of neurosarcoidosis represents a challenge in the clinical practice. Correlation with laboratory tests and imaging findings is essential(21,23). At MRI, frequently multiple and centrally located, heterogeneously contrast-enhanced lesions are observed with hypersignal on T2-weighted sequences. There may be fusiform medullary expansion. For patients with a compatible clinical condition, in the presence of pial enhancement beyond the intramedullary lesions, medullary sarcoidosis must be included among the differential diagnoses (Figure 6). The lesions tend to regress with the utilization of corticoids, generally after clinical improvement(22,24,25). 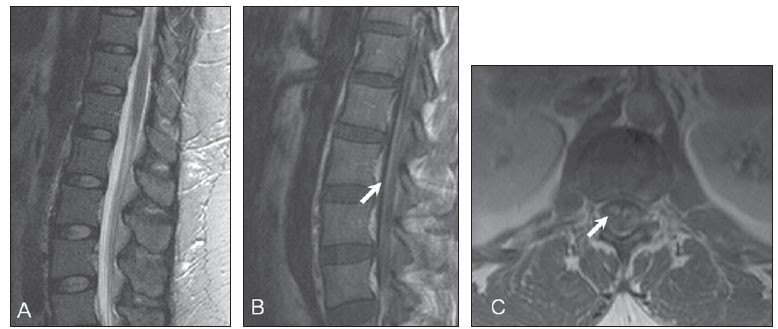 Figure 6. MRI study of a patient diagnosed with neurosarcoidosis, showing a slight increase of the conus medullaris on sagittal (A) T2-weighted sequence, with no alteration in central signal, with post-contrast pial and radicular enhancement (arrows on B and C). CONCLUSION MRI is the method of choice in the approach to myelitis. In the present study, the authors have attempted to describe some relevant imaging findings of inflammatory conus medullaris diseases which can differentiate them from neoplastic or vascular lesions, while suggesting a specific etiologic agent. The type of contrast-enhancement must be carefully evaluated. The "arborized" pattern is typical of neuroschistosomiasis, while a peripheral annular enhancement may be present in cases of granulomatous lesions such as in tuberculosis and toxoplasmosis. In the presence of cysts, the diagnosis of cysticercosis should be considered, and may be confirmed by the identification of the scolex. The differentiation amongst the several viral etiologies by MRI alone is difficult, and association of imaging findings with clinical and laboratory findings is necessary. Finally, a comprehensive evaluation of the whole neuroaxis may be useful in the definition of a specific etiology, since in many cases there is concomitant intracranial involvement. REFERENCES 1. Mendonça RA. Spinal infections and inflammatory disorders In: Atlas SW, editor. Magnetic resonance imaging of the brain and spine. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. p. 1647-737. 2. Choi KH, Lee KS, Chung SO, et al. Idiopathic transverse myelitis: MR characteristics. AJNR Am J Neuroradiol. 1996;17:1151-60. 3. Tumors of the spine [Book review]. AJNR Am J Neuroradiol. 2009;30:E137. 4. Silva LC, Maciel PE, Ribas JGR, et al. Schistosomal myeloradiculopathy. Rev Soc Bras Med Trop. 2004;37:261-72. 5. DeSanto J, Ross JS. Spine infection/inflammation. Radiol Clin North Am. 2011;49:105-27. 6. Sanelli PC, Lev MH, Gonzalez RG, et al. Unique linear and nodular MR enhancement pattern in schistosomiasis of the central nervous system: report of three patients. AJR Am J Roentgenol. 2001;177:1471-4. 7. Gonçalves FG, Neves PO, Jovem CL, et al. Chronic myelopathy associated to intramedullary cysticercosis. Spine (Phila Pa 1976). 2010;35: E159-62. 8. Homans J, Khoo L, Chen T, et al. Spinal intramedullary cysticercosis in a five-year-old child: case report and review of the literature. Pediatr Infect Dis J. 2001;20:904-8. 9. Prabhakar S, Thussu A. Central nervous system tuberculosis. Neurol India. 1997;45:132-40. 10. Lu M. Imaging diagnosis of spinal intramedullary tuberculoma: case reports and literature review. J Spinal Cord Med. 2010;33:159-62. 11. Elias J Jr, dos Santos AC, Carlotti CG Jr, et al. Central nervous system paracoccidioidomycosis: diagnosis and treatment. Surg Neurol. 2005;63 Suppl 1:S13-21. 12. Gültaşli NZ, Ercan K, Orhun S, et al. MRI findings of intramedullary spinal cryptococcoma. Diagn Interv Radiol. 2007;13:64-7. 13. Poon TP, Tchertkoff V, Pares GF, et al. Spinal cord toxoplasma lesion in AIDS: MR findings. J Comput Assist Tomogr. 1992;16:817-9. 14. de Seze J, Lanctin C, Lebrun C, et al. Idiopathic acute transverse myelitis: application of the recent diagnostic criteria. Neurology. 2005;65:1950-3. 15. Transverse Myelitis Consortium Working Group. Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002;59:499-505. 16. Tartaglino LM, Friedman DP, Flanders AE, et al. Multiple sclerosis in the spinal cord: MR appearance and correlation with clinical parameters. Radiology. 1995;195:725-32. 17. Filippi M, Rocca MA, Moiola L, et al. MRI and magnetization transfer imaging changes in the brain and cervical cord of patients with Devic's neuromyelitis optica. Neurology. 1999;53:1705-10. 18. Gilden DH, Beinlich BR, Rubinstien EM, et al. Varicella-zoster virus myelitis: an expanding spectrum. Neurology. 1994;44:1818-23. 19. Ferraz AC, Gabbai AA, Abdala N, et al. Magnetic resonance in HTL-I associated myelopathy. Leukoencephalopathy and spinal cord atrophy. Arq Neuropsiquiatr. 1997;55:728-36. 20. Whiteman ML, Dandapani BK, Shebert RT, et al. MRI of AIDS-related polyradiculomyelitis. J Comput Assist Tomogr. 1994;18:7-11. 21. Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001;164(10 Pt 1):1885-9. 22. Zajicek JP, Scolding NJ, Foster O, et al. Central nervous system sarcoidosis - diagnosis and management. QJM. 1999;92:103-17. 23. Bradley DA, Lower EE, Baughman RP. Diagnosis and management of spinal cord sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2006;23:58-65. 24. Sakushima K, Yabe I, Nakano F, et al. Clinical features of spinal cord sarcoidosis: analysis of 17 neurosarcoidosis patients. J Neurol. 2011;258:2163-7. 25. Cohen-Aubart F, Galanaud D, Grabli D, et al. Spinal cord sarcoidosis: clinical and laboratory profile and outcome of 31 patients in a case-control study. Medicine (Baltimore). 2010;89:133-40. 1. MDs, Radiologists, Fellows Master degree, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 2. MD, Radiologist, Assistant at the Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. 3. PhD, Professor of Radiology, Chief of the Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. Mailing Address: Dr. Gustavo Balthazar da Silveira Carvalho Departamento de Diagnóstico por Imagem - EPM-Unifesp Rua Napoleão de Barros, 800, Vila Clementino São Paulo, SP, Brazil, 04024-002 E-mail: gustavobalthazar@gmail.com Received December 7, 2011. Accepted after revision July 20, 2012. * Study developed at Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554