Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Josie Naomi Iyeyasu1; Nivaldo Adolfo Silva Júnior2; Renata Bertanha3; Keila Monteiro de Carvalho4; Fabiano Reis5 |
|
|
A 21-year-old male patient was complaining of right-sided pulsatile proptosis since five months, after head trauma.
Images description Figure 1. Axial enhanced head CT discloses significant dilatation of right cavernous sinus and superior ophthalmic vein, suggesting the diagnosis of carotid cavernous fistula. The left cavernous sinus is normal. 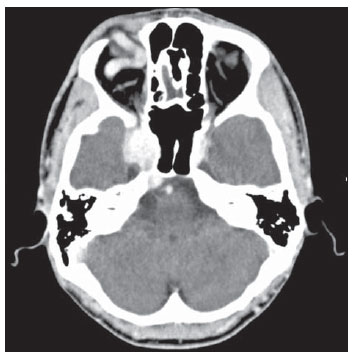 Figure 1. Axial enhanced head computed tomography (CT). Figure 2. 3D TOF MRA axial source image shows a dilated right cavernous sinus with a high signal intensity quite similar to the cavernous segment of the internal carotid artery. The arterio-venous junction is identified which confirms the presence of a fistula. The right superior ophthalmic vein is also dilated. The left-sided cavernous sinus and the superior ophthalmic vein present are normal. 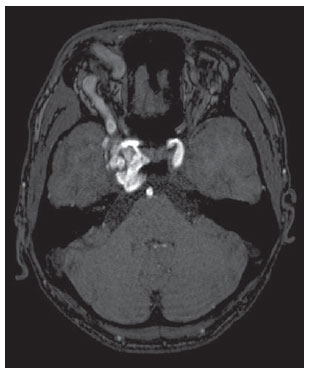 Figure 2. 3D time of flight (TOF) magnetic resonance angiography (MRA) source image. Figure 3. Axial MIP reconstruction of 3D TOF MRA shows a significant dilatation of the right cavernous sinus and superior ophthalmic vein. Moreover, the inferior petrosal sinus, the internal jugular vein bulb, the distal segment of the sigmoid sinus and the sphenoparietal sinus of Breschet can be visualized in the right side. 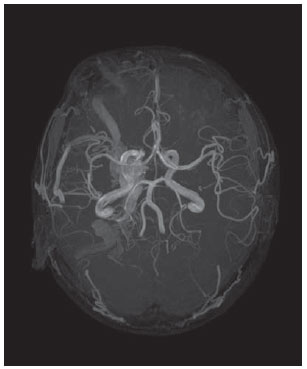 Figure 3. 3D TOF MRA maximum intensity projection (MIP) reconstruction. Diagnosis: Carotid cavernous fistula (CCF). COMMENTS Fistula is a pathological communication between one or several arterioles towards a vein, without an interposing nidus. Such lesions have high flow and pressure(1). CCFs are a specific type of fistula where an abnormal communication between the cavernous segment of the internal carotid artery and the venous plexus of the cavernous sinus occurs(2,3). Such fistulas may be either spontaneous (25% of cases) or secondary to trauma (75% of cases)(3). The latter may develop immediately or hours/ days after trauma(1). It is estimated that 0.17% of craniofacial traumas evolve with development of a carotid cavernous fistula(1). CCFs may be classified as direct (Barrow type A), where there is o a direct communication between the cavernous segment of the carotid artery and the cavernous sinus, or indirect (Barrow types B, C and D) in which it is found an indirect communication between branches of the internal/external carotid arteries and the cavernous sinus(4). CCFs associated signs and symptoms include: headache, intracranial (subarachnoid and subdural) hemorrhages and epistaxis that result from the venous hypertension in the dural sinuses(1). On the other hand, the most frequent ocular signs and symptoms are: pulsatile exophthalmos, orbital bruit, hyposphagma, ophthalmoplegia, ocular pain, increased intraocular pressure and decreased visual acuity due to the reversal blood flow towards the ophthalmic veins and the overload/ dilatation of the cavernous sinus(1). The radiologic diagnosis may be suggested either by conventional CT or MRI. Both can demonstrate morphological anomalies (the most common ones corresponding to dilatation of the superior ophthalmic vein(5) and exophthalmos(6)) The diagnosis is confirmed by conventional catheter angiography which also provides information about flow velocity, the arterial feeders as well as the pattern and location of the venous drainage. These clues allow the best selection of treatment. The analysis of the venous drainage pattern is critical to predicts the prognosis. The fistulas in which the venous drainage occur mainly towards to the ophthalmic vein are associated with progressive visual loss and those with reflux into cortical veins present a high risk for intracranial hemorrhage. CT angiography(5) or MRA (specially 3D TOF MRA source images) are extremely useful diagnostic modalities in the evaluation of carotid cavernous fistulas. Except for flow velocity, the angioarchitecture of the fistula (location, arterial feeders and drainage veins) can be demonstrated with high sensitivity and specificity(7). The treatment of choice depends on the intensity of the blood flow through the lesion. Low-flow fistulas may be managed conservatively or by using manual carotid compression considering that 25-50% of the fistulas present spontaneous resolution(3). Ocular hypotensive drugs and stereotactic surgery(8) can be also used. On the other hand, high-flow fistulas and those with cortical venous drainage require treatment since they may evolve with intracranial hemorrhage, vision loss, lethal epistaxis(4) and neurological deterioration(8). Endovascular intervention is the first option for treatment. This consists on the occlusion of the fistulous zone by devices like detachable balloons, microcoils, liquid embolic agents or covered stents. The most frequently used endovascular approach is the arterial one, mainly in cases of direct fistulas (Barrow type A). In other types of fistulas, venous or combined approach may be utilized(8). The rate of success of the procedure depends on the dimensions of both the cavernous and fistula(2). In treatment failure, surgery can still be applied. It consists in the surgical ligation of the internal carotid artery or packing of the cavernous sinus(8). REFERENCES 1. Borba R, Sonda I, Dini LI, et al. Carotid-cavernous fistula with lethal epistaxis: case report. Arq Neuropsiquiatr. 2001;59:276-9. 2. Vasconcelos BC, Porto GG, Carneiro SC. Posttrauma exophthalmos caused by a carotid-cavernous fistula. Braz J Otorhinolaryngol. 2009;75:767. 3. Mesa JC, Mascaró F, Muñoz S, et al. Orbital approach for treatment of carotid-cavernous sinus fistula. Arch Soc Esp Oftalmol. 2008;83:719-22. 4. Kaplan JB, Bodhit AN, Falgiani ML. Communicating carotid-cavernous sinus fistula following minor head trauma. Int J Emerg Med. 2012;5:10. 5. Kubal WS. Imaging of orbital trauma. Radiographics. 2008;28:1729-39. 6. Chen CC, Chang PC, Shy CG, et al. CT angiography and MR angiography in the evaluation of carotid cavernous sinus fistula prior to embolization: a comparison of techniques. AJNR Am J Neuroradiol. 2005;26:2349-56. 7. Rucker JC, Biousse V, Newman NJ. Magnetic resonance angiography source images in carotid cavernous fistulas. Br J Ophthalmol. 2004;88:311. 8. Gemmete JJ, Chaudhary N, Pandey A, et al. Treatment of carotid cavernous fistulas. Curr Treat Options Neurol. 2010;12:43-53. 1. Master, MD, Ophthalmologist, Department of Ophthalmo-Otolaryngology, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. 2. Attending Physician, Department of Radiology, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCMUnicamp), Campinas, SP, Brazil. 3. MD, Resident, Department of Radiology, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. 4. Professor, Department of Ophthalmo-Otolaryngology, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. 5. PhD, Professor, Department of Radiology, Faculdade de Ciências Médicas da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. Mailing Address: Dr. Fabiano Reis Hospital de Clínicas da Universidade Estadual de Campinas (HC-Unicamp) Rua Vital Brasil, 251, Cidade Universitária Zeferino Vaz Campinas, SP, Brazil, 13083-888 Caixa Postal 6142 E-mail: fabianoreis2@gmail.com This study was developed at Hospital de Clínicas da Universidade Estadual de Campinas (HC-Unicamp), Campinas, SP, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554