INTRODUCTION
Acute cerebellitis or cerebellar ataxia is an uncommon inflammatory syndrome characterized by an early onset of cerebellar dysfunction. Although this syndrome is generally benign and self-limited, it may run its course with deadly alterations(1).
This condition is considered as one of the main causes of acute cerebellar dysfunction in the childhood and its etiology may be infectious, usually viral, post-infectious or post-vaccinal(1). Cases of viral origin with varicella-related cerebellitis are most frequently reported, occurring in 25% of the affected infant patients(2).
The clinical picture is generally variable, with fever, abnormal, spontaneous eye movements, tremor, ataxia of trunk and limbs, dysarthria, headache, nausea, vomiting and consciousness alterations. Less frequently, signs of meningeal irritation and seizures may be observed(1,3). Severe complications, such as intracranial hypertension, obstructive hydrocephalus, tonsillar herniation and cerebral trunk compression are less frequently found(4).
The diagnosis of acute cerebellitis may be hardly achieved in the presence of subtle signs and symptoms of cerebellar compromise and normal cephalorachidian fluid analysis. In such cases, magnetic resonance imaging (MRI) is a valuable method for determining an early diagnosis. Case reports with MR images, particularly demonstrating the disease progression, are rarely found in the literature(1,4,5).
The present report is aimed at describing a clinical case of severe acute cerebellitis with favorable evolution due to early diagnosis and treatment.
CASE REPORT
A female, 12-year-old patient with clinical signs of headache, vomiting and inappetence for three days and history of recent hospital admission due to dehydration after gastroenteritis.
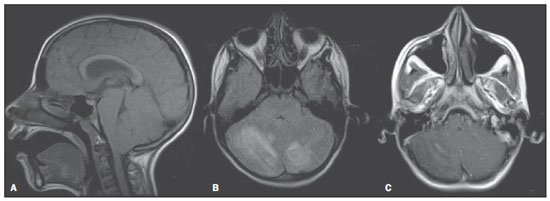
The patient underwent cranial computed tomography which demonstrated dilatation of the supratentorial ventricular system and diffuse fading of cortical sulci and fissures. Brain MRI demonstrated areas with hypersignal intensity on T2weighted and FLAIR images in the cerebellar hemispheres in association with expansile effect with fading of the sulci and tonsillar herniation, besides a slight leptomeningeal enhancement compatible with acute cerebellitis (Figure 1).
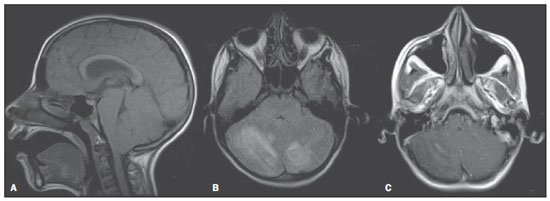
Figure 1. A: Sagittal MRI T1-weighted image demonstrating tonsillar herniation. B: Axial MRI FLAIR image with hypersignal on cerebellar hemispheres in association with expansile effect with compression over the floor of the fourth ventricle. C: Axial MRI T1-weighted image demonstrating subtle paramagnetic contrast uptake.
Treatment with mannitol and corticoid drugs was started and maintained up to the patient discharge. Three days after starting the treatment, the patient was asymptomatic. Follow-up CT demonstrated a favorable progression with decreased edema and hydrocephalus, with only small hypoattenuating areas in the cerebellar hemispheres. The last CT image acquired at the tenth day was normal.
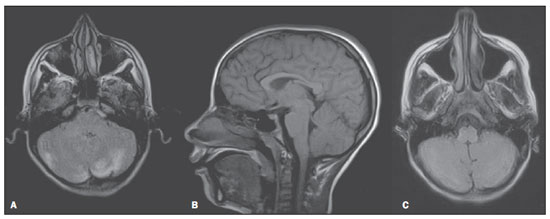
Follow-up with magnetic resonance imaging was performed at the 17th (Figure 2A) day and 75 days after admission (Figures 2B and 2C). A good evolution of the imaging findings was observed, with progressive decrease in areas of signal alteration, edema and resolution of the tonsillar herniation.
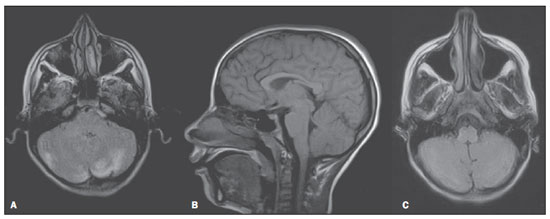
Figure 2. A: Axial FLAIR MRI demonstrating subtle reduction of areas with hypersignal intensity at the 17th day after admission. B,C: Last follow-up – sagittal MRI T1-weighted image with no significant alteration, and axial FLAIR MRI demonstrating minimal hypersignal in the cerebellar hemispheres.
The differential diagnosis for cerebellar syndromes is made with consideration of inflammatory/infectious processes, tumors, traumas, stroke and demyelinating diseases. In the present case, the etiologic agent of the cerebellitis could not be isolated, but the patient presented previous history of gastroenteritis. Varicella is the main pathogen, but in cases preceded by severe diarrhea, rotavirus infection should be considered(6,7).
Generally, the disease is benign and self-limited, but in cases of complication by hydrocephalus, intracranial hypertension and tonsillar herniation the prognosis is worse. In the present case, the patient presented such alterations, but recovered completely after the clinical treatment. Liquor pleocytosis was present, with normal protein and glucose levels.
In cases of cerebellitis, computed tomography images may be normal; on the other hand, in more severe cases, with mass effect, findings compatible with obstructive hydrocephalus shall be visualized, characterizing compression over the fourth ventricle, dilatation of the supratentorial ventricular system, and diffuse fading of cortical sulci and fissures(8).
The imaging method recommended for evaluating patients under clinical suspicion of acute cerebellitis is brain MRI(1). With such method, the posterior fossa is seen in better detail than with computed tomography, since artifacts produced by the skull bone are eliminated so the identification and differentiation of the cortex and white matter in the cerebellar hemispheres is easier. Signal alterations are typical and together with the clinical findings lead to diagnosis.
On T1-weighted sequences, the cerebellar hemispheres present symmetric low sign intensity of the cortex, and on T2weighted and FLAIR sequences present hypersignal(1,4,5). Diffusion can differentiate vasogenic from cytotoxic edema(6,7). With the utilization of paramagnetic contrast agents, cortical lesions and adjacent leptomeninges may demonstrate anomalous contrast uptake(1,8). Additionally, because of the multiplanar characteristic of this method, the mass effect generated by the inflammation of the cerebellum on the roof of the fourth ventricle can be evaluated, determining the degree of hydrocephalus and tonsillar herniation.
Signal alterations in the cerebellar hemispheres on MRI T2-weighted and FLAIR sequences, such as the ones described in the present case, are highly suggestive but not pathognomonic. The MRI studies performed presented neither diffusion restriction nor any signal on the corpus callosum, which may be related either to the early treatment of the disease or to the window between the scans. The followup of clinical and imaging findings have documented the disease progression as well as its gradual resolution, with reduction of edema, of hypersignal areas and regression of the tonsillar herniation and hydrocephalus.
The treatment must be started as early as possible and will be compatible with the etiologic agent. In cases of undetermined etiology and in the presence of complications such as hydrocephalus and tonsillar herniation, the use of mannitol and corticoid drugs is mandatory(9).
REFERENCES
1. De Bruecker Y, Claus F, Demaerel P, et al. MRI findings in acute cerebellitis. Eur Radiol. 2004;14:1478-83.
2. Connolly AM, Dodson WE, Prensky AL, et al. Course and outcome of acute cerebellar ataxia. Ann Neurol. 1994;35:673-9.
3. Sawaishi Y, Takahashi I, Hirayama Y, et al. Acute cerebellitis caused by Coxiella burnetti. Ann Neurol. 1999;45:124-7.
4. Jabbour P, Samaha E, Abi Lahoud G, et al. Hemicerebellitis mimicking a tumor on MRI. Childs Nerv Syst. 2003;19:122-5.
5. Horowitz MB, Pang D, Hirsch W. Acute cerebellitis: case report and review. Pediatr Neurosurg. 1991-1992;17:142-5.
6. Takanashi J, Miyamoto T, Ando N, et al. Clinical and radiological features of rotavirus cerebellitis. AJNR Am J Neuroradiol. 2010;31:1591-5.
7. Kobayashi S, Negishi Y, Ando N, et al. Two patients with acute rotavirus encephalitis associated with cerebellar signs and symptoms. Eur J Pediatr. 2010;169:1287-91.
8. Kato Z, Shimozawa N, Kokuzawa J, et al. Magnetic resonance imaging of acute cerebellar ataxia: report of a case with gadolinium enhancement and review of the literature. Acta Pediatr Jpn. 1998;40:138-42.
9. Göhlich-Ratmann G, Wallot M, Baethmann M, et al. Acute cerebellitis with near-fatal cerebellar swelling and benign outcome under conservative treatment with high dose steroids. Eur J Paediatr Neurol. 1998;2:157-62.
1. MDs., Residents in Radiology and Imaging Diagnosis at Hospital Escola de Itajubá, Itajubá, MG, Brazil.
2. MD, Radiologist, Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Physician Assistant at Hospital Escola de Itajubá, Itajubá, MG, Brazil.
3. MD, Neuroradiologist at Hospital Escola de Itajubá, Titular Professor, Division of Clinical Neurology, Faculdade de Medicina de Itajubá (FMIt), Neuroradiologist at Clínica Sul Mineira Tomosul and Clínica Magsul, Itajubá, MG, Brazil.
4. Neuropediatrician at Ambulatory of Learning Disorders, Universidade Estadual de Campinas (Unicamp), Campinas, SP, Neuroradiologist at Clínica Magsul, Pouso Alegre, MG, Brazil.
5. MD, Radiologist, Hospital Escola de Itajubá, Itajubá, MG, Brazil.
Mailing Address:
Dr. Gustavo Nunes Medina Coeli
Rua Oliveira Vieira de Souza, 456, Centro
Prata, MG, Brazil, 38140-970
E-mail: gustavonmc@yahoo.com.br
Received January 8, 2012.
Accepted after revision April 5, 2012.
Study developed at Hospital Escola de Itajubá, Itajubá, MG, Brazil.
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012