Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012
|
CASE REPORT
|
|
Post-traumatic duodenal obstruction by intramural hematoma: a case report and literature review |
|
|
Autho(rs): Henrique Silva Thé Pontes1; Eugênio Albuquerque Pequeno2 |
|
|
Keywords: Hematoma; Blunt abdominal trauma; Intestinal obstruction. |
|
|
Abstract: INTRODUCTION
Intramural duodenal hematoma is an uncommon cause of high intestinal obstruction in children with a history of blunt abdominal trauma. Such traumas are so trivial that sometimes they may even be forgotten by the child or, in other cases, may be so violent that young patients will not tell about it for fear of being punished by their parents. The present study is aimed at always including the possibility of duodenal intramural hematoma in the differential diagnosis in cases of acute high intestinal obstruction in children, even in the absence of accurate clinical data and pathognomonic imaging findings of parietal hematoma, taking into consideration the appropriateness criteria for imaging diagnosis in the pediatric group. CASE REPORT A six-year-old, female, white patient born in Mossoró, RN, Brazil was admitted to the emergency department of Hospital Infantil Luís França, in the city of Fortaleza, CE, Brazil on June 30, 2011, with clinical signs of high intestinal obstruction (postprandial bilious vomiting for two days, signs of mild dehydration and pain in the upper abdominal region). Her caretakers denied previous history of similar symptoms and/or previous known disorders. No history of weight loss or child maltreatment was reported. On the date of admission (June 30, 2011) a complete blood count and chest radiography were performed, both with normal results, and untimely, upper digestive endoscopy reaching only the first duodenal segment, revealing the presence of gastric stasis with a subtle inflammatory process, with no reference to the other duodenal segments. One day after admission (July 1st, 2011), esophageal-gastroduodenal seriography was performed, demonstrating complete obstruction in the transition between the second and third duodenal segments, blocking the passage of contrast agent and indicating luminal obstruction caused by due to parietal thickening (Figure 1). Abdominal ultrasonography was subsequently performed, demonstrating the presence of a hypoechoic solid lesion measuring 5.5 × 2.3 cm in the retroperitoneal region of the upper abdomen, at the level of the midline between the great vessels (inferior vena cava/aorta) and the normal pancreas. The lesion determined the ballottment of the superior mesenteric artery and obstruction of the duodenal transit (reverse peristalsis of the second segment causing reflux of fluid into the stomach and gastric stasis - which was utilized as acoustic window). No intralesional blood flow was observed at color Doppler study, suggesting the presence of post-traumatic obstruction by intramural duodenal hematoma, despite the absence of report on trauma or hematoma on the skin of the epigastric region (Figure 2). Then, a nasogastric tube was inserted for stomach decompression in association with parenteral hydration (venous), and computed tomography scan was requested for a better characterization of the condition.  Figure 1. Gastroduodenal seriography revealing total obstruction in the transition between the second and third duodenal segments, blocking the passage of the contrast agent. 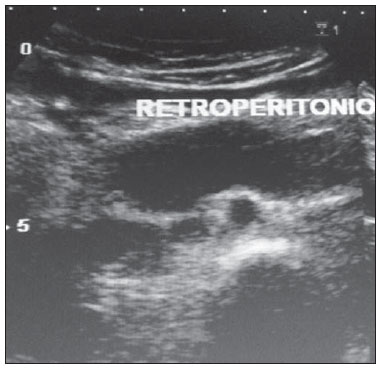 Figure 2. Abdominal ultrasonography showing a hypoechoic retroperitoneal lesion (5.5 x 2.3 cm) in the upper half of the abdomen, on the midline between the great vessels (inferior vena cava/aorta) and the normal pancreas. The lesion determined obstruction of the duodenal transit (reverse peristalsis of the second segment and fluid reflux into the stomach), and gastric stasis, which was utilized as acoustic window). On the second day of hospital stay, unenhanced and contrast-enhanced multislice computed tomography of the upper abdomen was performed in other institution, demonstrating the presence of a hypodense expansile lesion with subtle contrast uptake, located in a retroperitoneal site and determining extrinsic compression and/or duodenal invasion by contiguity (lesion of neoplastic lymphoproliferative nature determining duodenal obstruction) (Figure 3). 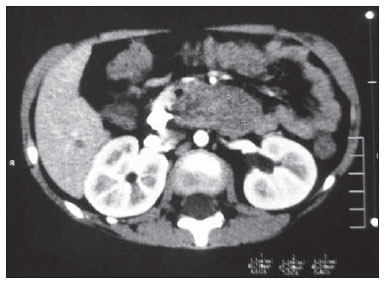 Figure 3. Contrast-enhanced multislice computed tomography demonstrating a hypodense expansile lesion with subtle contrast uptake in a retroperitoneal site (probable lymph node mass) determining extrinsic compression and/or duodenal invasion by contiguity. With the diagnostic hypothesis of lymphoproliferative neoplasia determining duodenal occlusion, surgery was indicated in order to have the lesion biopsied and provide treatment for the obstructive condition. However, immediately before the surgery (July 5, 2011) an adult reported that had witnessed a violent abdominal trauma suffered by the patient, caused by a bicycle handlebar, two days before admission to the emergency department. Because of the good overall condition of the patient and, with basis on the new information, the surgery was cancelled and parenteral feeding and expectant treatment were indicated. The patient presented a good response to the treatment, with absence of drainage of gastric/biliary juice through the tube and no abdominal pain. Follow-up with gastroduodenal seriography was performed on the ninth day after admission (July 7, 2011), demonstrating duodenal transit free from any obstacles (Figure 4). The patient, totally healed, was discharged on the tenth day.  Figure 4. Gastroduodenal seriography showing free duodenal transit in physiological time, with no obstacle. DISCUSSION Post-traumatic intramural duodenal hematomas in children occur in about 2-3% of cases of blunt abdominal trauma(1,2). Anatomical factors such as the retroperitoneal attachment of the duodenum, positioning in front of the lumbar spine, a wealthy subserous/submucosal vascular plexus and a poor muscle-tone of the anterior abdominal wall contribute to the onset of intramural duodenal hematomas. Intramural duodenal hematomas may occur at any age and in both men and women, but, in the pediatric group, boys are most frequently affected(3). The proximity between the duodenum and the pancreas explains why traumatic pancreatitis is the comorbidity most frequently associated with intramural duodenal hematomas. Jewett et al.(1) have reported association with pancreatitis in 21% of their cases in a review article on 182 cases of parietal duodenal hematoma in children. However, the trauma is sometimes trivial, and some children simply forget to report their occurrence(4). Traumas caused by bicycle handlebars, traffic accidents and violent sports constitute the main etiological factors in these cases(4,5). Child maltreatment must always be considered as a causative factor, particularly in children under the age of five(6,7). In patients with coagulopathies - a special subgroup -, such coagulopathies represent an etiological factor in cases of minimum trauma and endoscopic procedures(8). Such a fact suggests the indication of endoscopic procedures in children only when platelets count is above 50,000/mm3, with normal prothrombin time and partial thromboplastin time(9). The physiopathology of post-trauma intramural duodenal hematomas is related to the shock of the loop against the lumbar spine caused by a trauma agent, resulting in contusion and parietal bleeding which generates the hematoma. Such hematoma may grow and gradually cause luminal obstruction of the organ. The diagnosis of intramural duodenal hematoma is based on signs and symptoms of high intestinal obstruction after a trauma, supported by radiological evidences of the condition(10). Contrast-enhanced computed tomography is the method of choice for the diagnosis of intramural duodenal hematoma, but ultrasonography is a valuable and noninvasive method, which provides important data on the intramural nature of the lesion. Endoscopic study and magnetic resonance imaging may be performed in isolated cases where clinical data and conventional imaging methods are inconclusive. In the present case, there was a certain inversion in the sequence of supplementary studies because a computed tomography apparatus was not available in the service at that moment. The conservative treatment consists in gastric decompression (nasogastric tube) and parenteral nutrition. Coagulation disorders must be ruled out or treated. If pancreatitis is present, it must be duly treated. The clinical follow-up may be performed by means of ultrasonography. After few days, usually one week, the nasogastric tube may be periodically closed for testing and stimulation of the duodenal transit. Clear liquids are introduced and the diet is gradually reestablished (restricted liquid → pureed → bland → general). In most cases, hematomas resolve in two weeks. If neither clinical improvement nor resolution is observed in two weeks, surgery is indicated. The conservative treatment of intramural duodenal hematomas is very successful, particularly in early diagnosed cases. As regards the present case, two situations should be taken into consideration to avoid misdiagnosis: the first one is related to the denial of abdominal trauma. The second situation refers to the fact that a brutal trauma abruptly inflicted with extreme violence/velocity may injure an organ or internal structure without injuring the skin on the structure where trauma was inflicted. Martial arts students are specifically instructed to do so. Thus, the medical community must be aware of these factors, and include this diagnostic possibility (intramural duodenal hematoma), even if it is very improbable, in the presence of signs of high intestinal obstruction. REFERENCES 1. Jewett TC Jr, Caldarola V, Karp MP, et al. Intramural hematoma of the duodenum. Arch Surg. 1988;123:54-8. 2. Kaufman RA, Towbin R, Babcock DS, et al. Abdominal upper trauma in children: imaging evaluation. AJR Am J Roentgenol. 1984;142:449-60. 3. Felson B, Levin EJ. Intramural hematoma of the duodenum: a diagnostic roentgen sign. Radiology. 1954;63:823-31. 4. Bass D. Duodenal hematoma occurs in children with bicycle injuries. BMJ. 2001;323:754-5. 5. Lam JP, Eunson GJ, Munro FD, et al. Delayed presentation of handlebar injuries in children. BMJ. 2001;322:1288-9. 6. Andersson A, Bergdahl L. Intramural hematoma of the duodenum in children: review of literature and report of two cases. Am Surg. 1973;39:402-5. 7. Woolley MM, Mahour GH, Sloan T. Duodenal hematoma in infancy and childhood: changing etiology and changing treatment. Am J Surg. 1978;136:8-14. 8. Karjoo M, Luisiri A, Silberstein M, et al. Duodenal hematoma and acute pancreatitis after upper gastrointestinal endoscopy. Gastrointest Endosc. 1994;40:493-5. 9. Ramakrishna J, Treem WR. Duodenal hematoma as a complication of endoscopic biopsy in pediatric bone marrow transplant recipients. J Pediatr Gastroenterol Nutr. 1997;25:426-9. 10. Maull KI, Fallahzadeh H, Mays ET. Selective management of post-traumatic obstructing intramural hematoma of the duodenum. Surg Gynecol Obstet. 1978;146:221-4. 1. MD, Radiologist, Head of the Service of Ultrasonography Petite Image, Hospital Infantil Luís França, Fortaleza, CE, Brazil. 2. MD, Radiologist, Head of the Service of Radiology, Hospital Infantil Luís França, Fortaleza, CE, Brazil. Mailing Address: Dr. Henrique Silva Thé Pontes Hospital Infantil Luís França Avenida Heráclito Graça, 60, Centro Fortaleza, CE, Brazil, 60140-060 E-mail: henriquesilvathe@terra. com.br Received August 17, 2011. Accepted after revision March 1st, 2012. Study developed at Hospital Infantil Luís França, Fortaleza, CE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554