INTRODUCTION
Tenosynovitis of the first extensor compartment of the wrist is a common condition, surrounded by myths. In the recent years, there is a growing interest in the utilization of ultrasonography either as a diagnostic tool or as a forensic tool in medical-legal litigations involving the disease. The present article is aimed at scientifically reviewing some of the most relevant aspects regarding terminology, physiopathogenesis, diagnosis and follow-up of tenosynovitis of the first extensor compartment of the wrist.
TERMINOLOGY
Tenosynovitis of the first extensor compartment of the wrist is also recognized as De Quervain's tenosynovitis after the Swiss surgeon Fritz de Quervain, who was also famous for his studies on the thyroid gland. However, the appropriateness of such eponym is controversial, since the original article simultaneously describes the cases of three physicians, Quervain, Sandos and Kocher, the latter having formerly been boss of Quervain and a Nobel prize winner in 1909 for his studies on the thyroid gland(1). The pioneerism in these reports is also questionable, since a very similar clinical entity had been described about 20 years before by Henry Gray on his classical anatomy book, where the term
washerwoman's sprain was coined(2).
The term
tenosynovitis is also somewhat inappropriate, since the main histological marker for the condition is the mucopolysaccharide deposition in the tendon sheath, indicating degenerative process(3,4). More precisely, the external reticular layer of the sheath is histologically normal, while the internal layer demonstrates myxoid or mucinous degeneration, and the central layer demonstrates vascular proliferation, and macrophage infiltration. Despite this remark, the authors routinely use the term
tenosynovitis to describe the tendon sheath thickening in order to facilitate the communication with the referring physician. Fluid distension of the tendon sheath, without associated parietal thickening or tendon abnormalities, is described as
synovitis. In the present paper, the term tenosynovitis is liberally utilized to describe the clinical syndrome and not the anatomopathological diagnosis.
PHYSIOPATHOGENESIS
To the best of the author's knowledge, there is no scientific evidence indicating that the condition is
caused by occupational or recreational overuse. Conversely, the analysis of historical series documents its higher prevalence among women over the centuries, even at times when only men effectively participated in the manual, repetitive work.
Therefore, even though overuse may
exacerbate symptoms, the
cause of tenosynovitis is widely unknown, with a probable predominant role of sex-related genetic factors. An illustrative comparison can be made with patients suffering from ischemic heart disease, in whom excessive physical activity
exacerbates symptoms, but does not
cause the disease. The legal implications of the semantic difference between the verbs
cause and
exacerbate are considerable and must be emphasized.
Genetic factors may equally predispose individuals to anatomical variations in the first compartment such as vertical septum and accessory tendons of the abductor pollicis longus, both considered as risk factors for development of tenosynovitis. Besides predisposing to the development of anatomical variations, genetic factors may also be involved in the physiopathogenesis while modulating individual's sensitivity to pain and psychological profile.
CLINICAL DIAGNOSIS
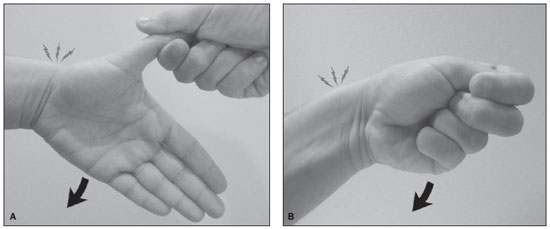
The diagnosis of tenosynovitis of the first extensor compartment of the wrist has been historically based on the finding of pain over the styloid process of the radius that is exacerbated with thumb and wrist movement. Crepitation and triggering may also be rarely observed. However, most recently, a worrisome question on the subjectivity and reproducibility of the clinical diagnosis in medical-legal litigations has emerged, and helped to popularize the use of ultrasound in the assessment of the patients. In this context, it is widely known that there may be discrepancies between the clinical and sonographic diagnoses. The choice between clinical assessment and imaging evaluation as the best diagnostic method is controversial, with fervorous supporters in both sides. A relevant factor contributing to such controversy is the lack of a gold standard, so the comparison between different methods is complex and imperfect. In the authors' opinion the evaluation by the referring physician is sovereign to determine the treatment, but not to establish the anatomical diagnosis. Regardless such uproar, it is interesting to recognize the correct terminology of clinical tests frequently used in the clinical assessment of these patients, which could be utilized as a strong argument to neutralize those who heavily criticize the virtues of the imaging modality. In fact, no other area of semiology has a misconception so deeply rooted as the Finkelstein's test. Over the years, several variations of the test have been described without taking historical background into consideration, which has lead to innumerable redundant, ambiguous and equivocal designations. In order to solve such misunderstandings, one should get back to 1930, when Finkelstein published his classical article describing the original technique for assessing patients with tenosynovitis of the first extensor compartment(5) (Figure 1A): "
On grasping the patient's thumb and quickly abducting the hand ulnarward, the pain over the styloid tip is excruciating. This is probably the most pathognomonic objective sign."
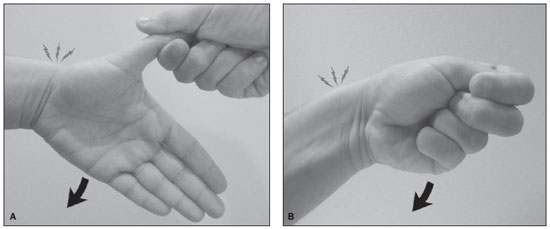
Figure 1. Tests utilized for clinical diagnosis of tenosynovitis of the first extensor compartment. A: Finkelstein's test, which consists in holding the patient's thumb while the hand is forced into ulnar deviation. B: Eichoff's test, which consists in grasping the thumb in the palm of the hand while the wrist is ulnar deviated. Both tests are positive in the presence of pain over the radial styloid process during the ulnar deviation of the wrist. The tests names were not confused or equivocally written, for surprise of those who equivocally describe the maneuver of grasping the thumb in the palm of the hand as Finkelstein's test.
At that time, other physicians shared the Filkelstein's interest in the assessment of individuals with tenosynovitis of the first extensor compartment, including Eichoff, who had published his work in 1927(6). The Eichoff's report, however, had poor global penetration, possibly because it was written in a non-English language. Ironically, it was Finkelstein himself who first translated into English and published the description of the clinical test created by Eichoff, duly referencing his peer(5) (Figure 1B): "
Eichoff explains... a simple experiment... if one places the thumb within the hand and holds it tightly with the other fingers, and then bends the hand severely in ulnar abduction, an intense pain is experienced on the styloid process of the radius, exactly at the place where the tendon sheath takes its course."
For unknown reasons, the historical correction has faded away over time. In the recent years, with few exceptions(7,8), a number of textbooks and scientific papers have been unfair to Eichoff, as they mentioned the maneuver of grasping the thumb in the palm of the hand as
Finkelstein's test.
SONOGRAPHIC DIAGNOSIS
In the authors' routine, ultrasound examination is performed while the patient comfortably rests the ulnar aspect of his hand on the examination table, utilizing only one focal zone of the equipment adjusted for the depth of the first extensor compartment. The investigation often requires generous amount of conductive gel on the skin surface in order to bring the region of interest into the focal zone. The transducer is placed transversely, adjacent to the radial tubercle, over the second extensor compartment. From the second extensor compartment, the transducer is moved to transversely scan the first extensor compartment, adjacent to the radial styloid process. The extensor pollicis brevis (EPB) and abductor pollicis longus (APL) occupy the first extensor compartment. A useful tip to memorize the names of the extensor tendons passing over the dorsal wrist consists in recognizing that their surnames alternate between
longus and
brevis as they advance towards the ulnar direction from the first to the third compartment: abductor pollicis
longus, extensor pollicis
brevis, extensor carpi radialis
longus, extensor carpi radialis
brevis and extensor pollicis
longus. In the first compartment, the abductor pollicis longus is thicker than the extensor pollicis brevis, which should not be confused with disease. The synovial sheath is depicted as a thin structure that surrounds the echogenic tendon fibers.
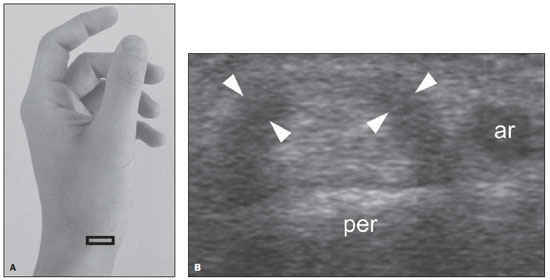
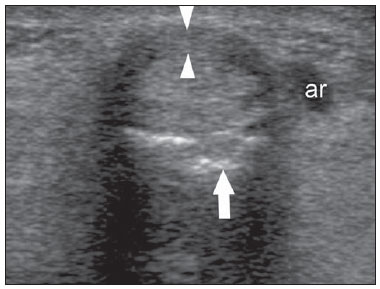
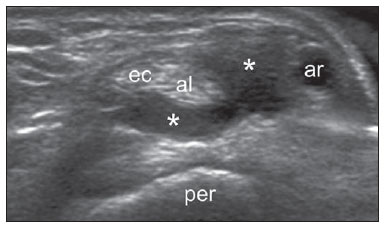
On ultrasound, the typical finding of tenosynovitis is the thickening and hypoechogenicity of the tendon sheath at the level of the radial styloid process (Figure 2). We rely on the subjectivity rather than on a mathematical definition of sheath thickening, which reinforces the relevance of the experience of the examiner, particularly because tendon sheath usually measures less than 1 mm thick. Contralateral comparison may be useful to identify subtle lesions. In chronic cases, bone erosion may be associated (Figure 3). More rarely, the tendon sheath has normal thickness, but there is fluid distension of the compartment caused by synovitis (Figure 4). The examination does not end with the diagnosis, since predisposing factors such as vertical septum and accessory tendons must be actively investigated as a cause of synovitis or secondary tenosynovitis. The role of these anatomical variations as risk factor for development of disease is intuitive, in the first case, with space reduction, and in the second case, with increase in the compartment contents.
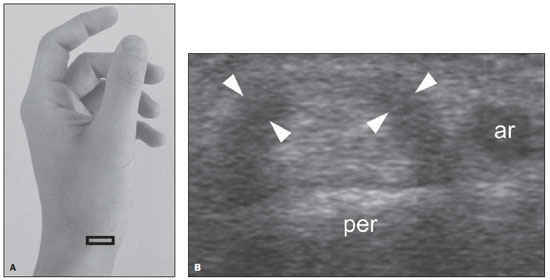
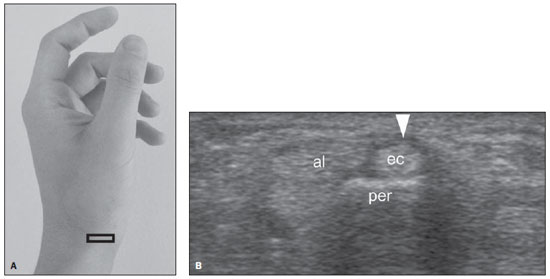
Figure 2. Tenosynovitis of the first extensor compartment. A: Transducer positioning. B: Corresponding image demonstrating thickening and hypoechogenicity of the tendon sheath (arrowheads), at the level of the radial styloid process (per), adjacent to the radial artery (ar). The involvement is most prevalent in women at a (at least) 10:1 ratio. The particular predisposition of tenosynovitis to affect puerperal women is also well established, primarily by endocrine influence on water retention, although mechanical factors resulting from the newborn care activities cannot be neglected.
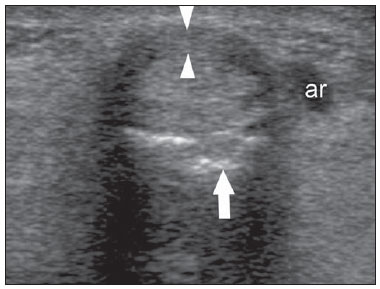
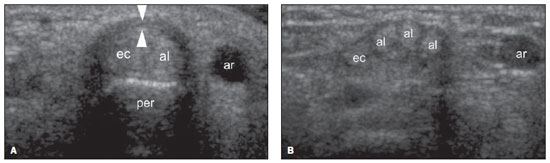
Figure 3. Tenosynovitis of the first extensor compartment in association with bone erosion. Transverse scan demonstrating thickening and hypoechogenicity of the tendon sheath (arrowheads) and a bone erosion (arrow) at the level of the radial styloid. Additionally, note the radial artery (ar).
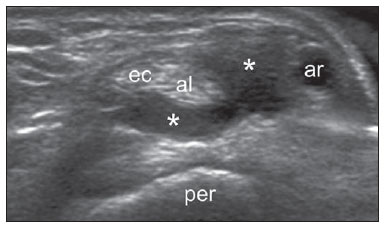
Figure 4. Synovitis of the first extensor compartment. Transverse scan demonstrating fluid distension of the tendon sheath (asterisks) which presents normal parietal thickness at the level of the radial styloid process. Also, note radial artery (ar), abductor pollicis longus (al), and extensor pollicis brevis (ec). Synovitis of the first extensor compartment is rare, but should be recognized, since its response to the conservative management tends to be more favorable, while its surgical indication is more controversial as compared with the classical presentation of tenosynovitis.
Vertical septum may be present in up to half of cases. It divides the first compartment into a ventral larger area, that contains the abductor pollicis longus, and a dorsal smaller space, that contains the extensor pollicis brevis(9). Subcompartimentalization and incomplete tenosynovitis is defined as vertical septum restricting the process to the sheath that surrounds only one of the tendons (Figure 5).
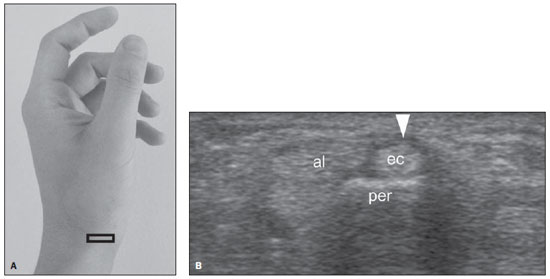
Figure 5. Tenosynovitis of the first extensor compartment, incomplete form. A: Transducer positioning. B: Corresponding image, at the level of the radial styloid process (per), demonstrating the tenosynovitis (arrowhead) restricted to the extensor pollicis brevis (ec). Note the abductor pollicis longus (al) with normal appearance. The description of the incomplete form of tenosynovitis of the first extensor compartment is relevant for management because it restricts the diffusion of locally injected substances; and from the surgical point of view it requires the release of the septum in order to avoid refractory postoperative symptoms.
Accessory tendons of the abductor pollicis longus are other recognized predisposing factor for the development of tenosynovitis of the first extensor compartment. Its detection is rather intuitive, distally to the radial styloid process where the sheath thickening is not so noticeable (Figure 6).
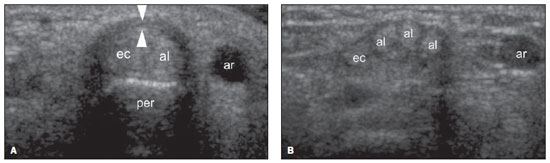
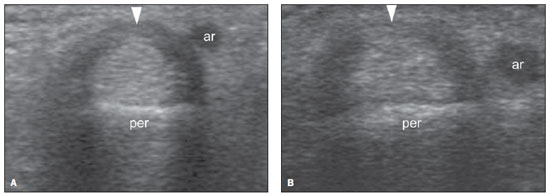
Figure 6. Tenosynovitis of the first extensor compartment with accessory tendons of the abductor pollicis longus. A: Transverse scan at the level of the radial styloid process (per), demonstrating tenosynovitis (arrowheads) affecting both the extensor pollicis brevis (ec) and the abductor pollicis longus (al), in an apparently trivial case. B: However, distal transverse evaluation demonstrates accessory tendons of the abductor pollicis longus. The identification of such anatomical variation that is seen in up to 75% of autopsies requires screening distally to the radial styloid process, where one can observe divergent tendons towards their insertion points. Also, note the radial artery (ar).
Although the usefulness of ultrasonography in the diagnosis of tenosynovitis of the first extensor compartment is unquestionable, its role in the follow-up is not established. In the follow-up of more than 200 patients over the last ten years, we have never observed resolution of the tendon sheath thickening after conservative treatment, thus we do not recommend sonographic follow-up to record the disappearance of the process after symptoms remission. Curiously, the authors' personal experience demonstrates that follow-up examination in patients who became asymptomatic after treatment are counterproductive and usually trigger symptoms relapse as the patient is informed about the persistence of the anatomic injury (Figure 7). Sheath thickening is not an inflammatory or infectious process (like sinusitis and pneumonia), but rather a degenerative phenomenon (like osteoarthritis). Thus, the treatment is not aimed at correcting an already-established anatomic injury, but rather at improving symptoms and slowing the progression of the disease. The authors' experience in the follow-up after surgical treatment is more positive, with some cases demonstrating complete sheath thickening regression (Figure 8). Synovitis is morphologically less refractory and fluid distension of the sheath usually disappears after conservative management.
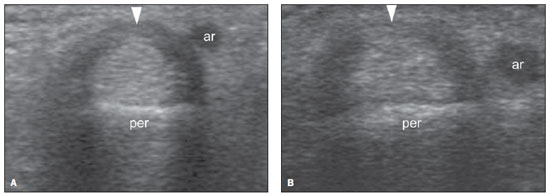
Figure 7. Follow-up of tenosynovitis of the first extensor compartment in a patient submitted to conservative treatment. A: Baseline transverse scan demonstrating thickening and hypoechogenicity of the sheath of the first extensor compartment (arrowhead) at the level of the radial styloid process (per). Also, note the radial artery (ar). B: Follow-up image acquired from a patient responsive to conservative treatment. In this specific case, the patient was asymptomatic and satisfied with the treatment as he entered the examination room, but symptoms relapsed after being informed about the persistence of the anatomical findings.

Figure 8. Follow-up of tenosynovitis of the first extensor compartment in a patient submitted to surgical treatment. A: Baseline transverse scan demonstrating thickening and hypoechogenicity of the first compartment sheath (arrowhead) at the level of the radial styloid process (per). B: Follow-up image acquired one year after surgical management, documenting complete resolution of the anatomical injury. Note the normal appearance of the extensor pollicis brevis (ec) and the abductor pollicis longus (al) after tendon sheath release. Also, note the radial artery (ar).
Tenosynovitis of the first extensor compartment of the wrist is a common condition, with controversial terminology and poorly known physiopathology. In this group of patients, ultrasonography can differentiate tenosynovitis from synovitis, the first one being an eminently inflammatory condition, and the later, predominantly degenerative. Additionally, ultrasonography can identify anatomical elements such as vertical septum and accessory tendons of the abductor pollicis longus, both potentially responsible for symptoms refractoriness, which may guide the adoption of a more aggressive management.
REFERENCES
1. de Quervain F. Ueber das Wesen und die Behandlung des stenosierenden Tendovaginitis am Processus styloideus radii. Munch Med Wochenschr. 1912;59:5-6.
2. Gray H. Anatomy, descriptive and surgical. Philadelphia, PA: Lea Brothers & Co.; 1893.
3. Clarke MT, Lyall HA, Grant JW, et al. The histopathology of de Quervain's disease. J Hand Surg Br. 1998;23:732-4.
4. Read HS, Hooper G, Davie R. Histological appearances in post-partum de Quervain's disease. J Hand Surg Br. 2000;25:70-2.
5. Finkelstein H. Stenosing tenovaginitis at the radial styloid process. J Bone Joint Surg. 1930;12:509-40.
6. Eichoff E. Zur Pathogenese der Tendovaginitis stenosans. Bruns' Beitrage Z Klin Chir. 1927; CXXXIX:746.
7. Arend CF. Master - Ultrassonografia musculoesquelética. 2ª ed. Rio de Janeiro, RJ: Revinter; 2012.
8. Dawson C, Mudgal CS. Staged description of the Finkelstein test. J Hand Surg Am. 2010;35:1513-5.
9. Kulthanan T, Chareonwat B. Variations in abductor pollicis longus and extensor pollicis brevis tendons in the Quervain syndrome: a surgical and anatomical study. Scand J Plast Reconstr Surg Hand Surg. 2007;41:36-8.
MD, Radiologist at Radimagem Diagnóstico por Imagem, Porto Alegre, RS, Brazil.
Mailing Address:
Dr. Carlos Frederico Arend
Avenida Cristóvão Colombo, 1691, Floresta
Porto Alegre, RS, Brazil, 90560-001
E-mail: carlos_arend@hotmail.com
Received December 16, 2011.
Accepted after revision June 28, 2012.
Study developed at Radimagem Diagnóstico por Imagem, Porto Alegre, RS, Brazil.
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012