INTRODUCTION
Physeal injuries are common sports-related fractures of the knee in children and adolescents. Distal femur physeal fractures correspond to 5-15% of all epiphyseal fractures, and most of them are of the Salter-Harris type II.
Proposed mechanisms, based on gross radiologic and morphologic features, include hyperextension or varus or valgus strain. Magnetic resonance imaging is a useful supplement to radiography in cases of occult or subtle injuries because distal femoral physeal injury leads to physeal growth disturbance or potential limb shortening in 14-38% and angular deformity in 24-51% of cases(1).
Historically, most Salter-Harris type I or II fractures are considered as innocuous injuries(2). The usual management is closed manipulation and casting of the leg. Failed closed reduction is recognized in the orthopedic literature as most often due to an interposed periosteal flap.
If the periosteal fragment is sufficiently large, surgical reduction is indicated with the purpose of reducing the incidence of premature physeal closure(3,4). Entrapped periosteum has been described as a cause of irreducible fractures in different sites including distal radius, proximal humerus and distal tibia(5). Other soft tissues such as muscles, tendons, ligaments and neurovascular bundles, may also get trapped in the fracture site, resulting in irreducibility.
CASE REPORT
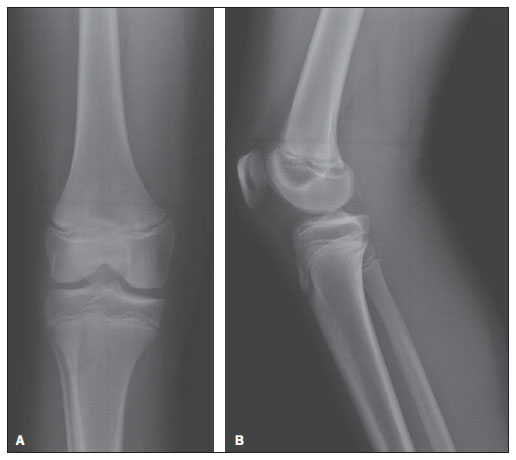
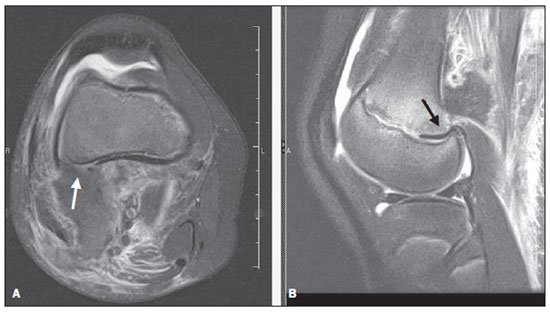
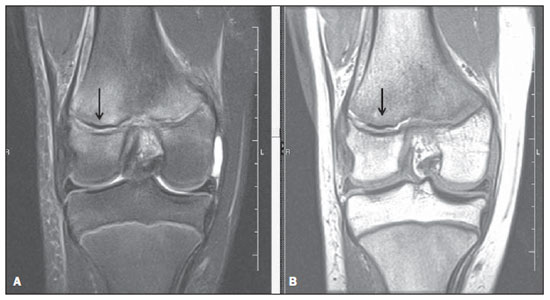
A female, 11-year-old child complaining of pain in the right knee after hyperextension while playing on a trampolin. Conventional radiography revealed a subtle widening of the physis in the lateral compartment of the knee (Figure 1). Because of failed closed reduction of the fracture, magnetic resonance imaging was performed four days after the trauma and demonstrated the presence of trapped periosteal fragment in the posterolateral aspect of the distal femoral physeal in association with distension of the belly of the femoral biceps muscle and small joint effusion (Figures 2 and 3). There were no other tendinous, ligament or meniscal injuries.
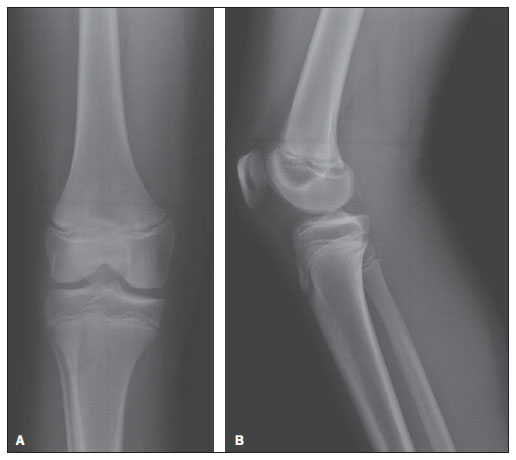
Figure 1.
A: Anteroposterior radiograph – subtle widening of the distal femoral physis lateral compartment.
B: Lateral radiograph – absence of significant changes.
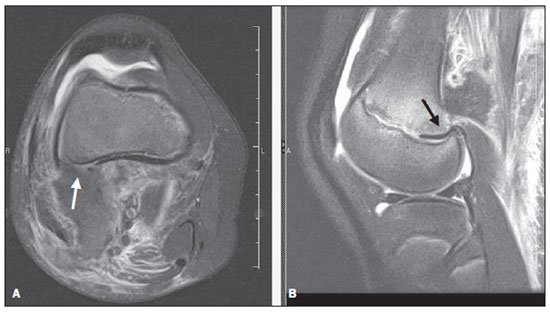
Figure 2. Magnetic resonance imaging, axial (
A) and sagittal (
B) T2-weighted images with fat saturation. Discontinuity in the posterolateral aspect of the cortical bone (A) associated with distension of the femoral biceps muscle and interposition of hypointense linear structure along the epiphyseal plate, compatible with periosteal fragment (
B).
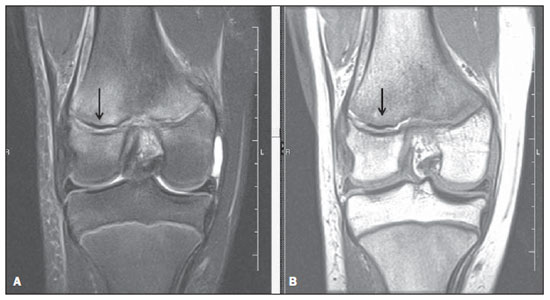
Figure 3. Magnetic resonance imaging, sagittal T2-weighted image with fat saturation (
A) and T1-weighted image (
B). Change in signal intensity along the lateral distal femoral epiphyseal plate, with interposition of a hypointense structure compatible with periosteal fragment.
After one week, the patient was submitted to surgery for removal of the periosteal fragment confirming diagnosis.
DISCUSSION
Conventional radiography is the mainstay of imaging for physeal injuries. Although the periosteum is not directly visualized with plain radiography, inappropriate closed reduction may suggest the presence of a trapped periosteum. A study has concluded that Salter-Harris types I and II fractures of the distal tibia with a residual physeal gap > 3 mm after closed reduction is suggestive of trapped periosteum(6). Such finding has been associated with premature physeal closure in 60% of the patients versus 17% in cases where the gap ranged from 1 to 3 mm. However, using radiography alone may underdiagnose the presence of trapped structures in the fracture. In some patients, trapped periosteum is not associated with physeal widening(6). Computed tomography with multiplanar reconstructions provides better outlining of osseous structures compared to radiography but it also does not allow visualization of the periosteum. Physeal widening, metaphyseal compression and epiphyseal fractures are better visualized at computed tomography than at conventional radiography. Late complications such as bony bridges are also better quantified with computed tomography(5).
Magnetic resonance imaging is not required in most cases of physeal injuries, but it does present some advantages such as absence of ionizing radiation, visualization of soft tissues and cartilage (including nonossified epiphysis) in addition to its multiplanar capability. The role of magnetic resonance imaging in the evaluation of Salter-Harris types I and II fractures is not yet well defined(7), but it is considered the best method for the assessment of the complications of such injuries, such as, for example, avascular necrosis and development of bony bridges through the epiphyseal plate, which cause developmental disorders.
Magnetic resonance imaging can be used to confirm or exclude physeal injuries that may be difficult or impossible to depict on radiography, particularly Salter-Harris types I and V fractures. It is also helpful to reveal associated ligamentous injuries, which occur in half of patients with physeal separations around the knee(3).
Although this entity of entrapped periosteum has been reported numerous times as a cause of irreducible fractures, there is a lack of preoperative diagnostic imaging depictions. The absence of normal periosteum and an asymmetrically wide physis with low signal intensity material within it suggest periosteal interposition in a physeal fracture(7).
CONCLUSION
Few studies have been published about radiological findings of trapped periosteum in epiphyseal fractures, in spite of the relevance of such a diagnosis in the selection of the treatment for Salter-Harris types I and II fractures. Magnetic resonance imaging may be effectively utilized for demonstrating soft tissue interposition in fractures, as reported in the present article, allowing an appropriate and safe surgical planning.
REFERENCES
1. Kritsaneepaiboon S, Shah R, Murray MM, et al. Posterior periosteal disruption in Salter-Harris Type II fractures of the distal femur: evidence for a hyperextension mechanism. AJR Am J Roentgenol. 2009;193:W540–5.
2. Rohmiller MT, Gaynor TP, Pawelek J, et al. Salter-Harris I and II fractures of the distal tibia: does mechanism of injury relate to premature physeal closure? J Pediatr Orthop. 2006;26:322–8.
3. Whan A, Breidahl W, Janes G. MRI of trapped periosteum in a proximal tibial physeal injury of a pediatric patient. AJR Am J Roentgenol. 2003;181:1397–9.
4. Dharmarajan R, Kumar AJ, Aldridge MJ. Medial meniscus interposition in proximal tibial epiphyseal fracture: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2003;11:252–4.
5. Quinn SF. Trapped periosteum. MRI Web Clinic – August 2011. [cited 2011 Aug 8]. Available from: http://www.radsource.us/clinic/1108
6. Barmada A, Gaynor T, Mubarak SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2003;23:733–9.
7. Raman S, Wallace EC. MRI diagnosis of trapped periosteum following incomplete closed reduction of distal tibial Salter-Harris II fracture. Pediatr Radiol. 2011;41:1591–4.
MD, Radiologist at Biocor Instituto, Nova Lima, MG, Brazil.
Mailing Address:
Dra. Marina Vimieiro Timponi de Moura
Rua Rio Grande do Norte, 501/501, Santa Efigênia
Belo Horizonte, MG, Brazil, 30130-130
E-mail: mvtimp@gmail.com
Received August 11, 2011. Accepted after revision February 24, 2012.
* Study developed at Biocor Instituto, Nova Lima, MG, Brazil.
 Vol. 45 nº 3 - May / June of 2012
Vol. 45 nº 3 - May / June of 2012