Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 3 - May / June of 2012
Vol. 45 nº 3 - May / June of 2012
|
ICONOGRAPHIC ESSAY
|
|
Common findings and pseudolesions at computed tomography colonography: pictorial essay |
|
|
Autho(rs): Augusto Castelli von Atzingen1; Dario Ariel Tiferes2; Carlos Alberto Matsumoto3; Thiago Franchi Nunes4; Marcos Vinicius Alvim Soares Maia5; Giuseppe D'Ippolito6 |
|
|
Keywords: Colonography; Computed tomography; Colorectal neoplasm; Colonic polyps. |
|
|
Abstract: INTRODUCTION
Computed tomography colonography (CTC), or virtual colonoscopy, is an imaging method based on the acquisition of multiple sections obtained by multidetector computed tomography (MDCT), generating sectional views of the colon that later can be reformatted in multiple planes and also processed in to allow endoluminal navigation, as in optical colonoscopy (OC)(1). Among its main advantages, this method is fast, as the examination is performed in less than 15 minutes, without requiring sedation. For over a decade, CTC has been utilized in the investigation of colonic polyps and colorectal cancer (CRC). Developments in the clinical and epidemiological knowledge on CRC and the many technological advances incorporated by CTC have transformed the method from an investigation tool into a viable option for CRC screening(2-4). The method is less invasive than OC for the screening of polyps and may preferably be utilized in asymptomatic individuals with low risk for development of CRC, in those who do not wish or cannot undergo OC, and in those cases where OC is incomplete(3). On the other hand, CTC presents some limitations as compared to OC in what concerns the impossibility of performing biopsies and the exposure to ionizing radiation(2). In spite of CTC having been introduced more than a decade ago, studies locally undertaken and published in the Brazilian literature are still scarce(5,6). The present essay is aimed at demonstrating the findings of the most common colonic lesions and pseudolesions observed at virtual colonoscopy and familiarizing the readers with the main technical features of the method. Patient preparation Bowel preparation if essential in CTC, in order to facilitate the detection of lesions and minimize the occurrence false-positive findings(7). It consists of the cleansing of the large bowel by means of a low residue diet for two days, and the use of non-irritating osmotic laxatives (bysacodil or macrogol) and antiflatulent drugs (simethicone). The utilization of either iodinated (ioxitalamic acid) or barium sulphate oral contrast agent is also indicated to label non-eliminated fecal residues and to facilitate the differentiation of pseudolesions(7). Iodinated contrast agent is most frequently utilized and is administered in the 12 hours preceding the CTC examination, by means of ingestion of 50 ml of the agent diluted in 200 ml of water(7). Technical features The images acquisition is done with the patient in dorsal and ventral decubitus, during apnea, after colonic distension with ambient air, according to patient's tolerance(8). The scans are preferably performed with tomography apparatuses with 16 or more detector rows. In the present study, a 64-detector-row CT apparatus (Brilliance 64; Philips Medical Systems, Cleveland, OH, USA) was utilized, and all the examinations were made with 64 × 0.625 mm collimation, slice thickness of 2 mm, reconstruction interval of 1 mm, pitch of 1079, rotation time of 0.5 s, and 120 kV and 60 mAs per section. The equivalent radiation dose per examination was, on average, 10 mSv, ranging between 6 and 19 mSv depending upon patients' size. No antispasmodic drug was utilized in the present study. The post-processing of the images was performed by means of the software package with volume-rendering capabilities (Philips Brilliance Workspace; Philips Medical Systems, Cleveland, OH, USA), with 2D multiplanar reformation and endoluminal navigation with virtual 3D colon dissection technique (Figures 1, 2 and 3). 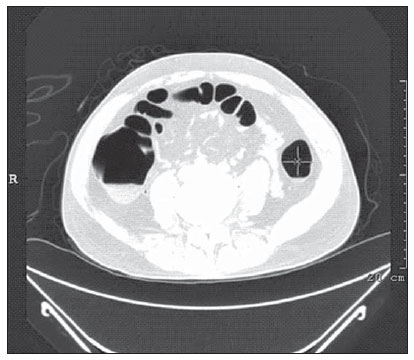 Figure 1. Normal colon. 2D CTC in the axial plane. 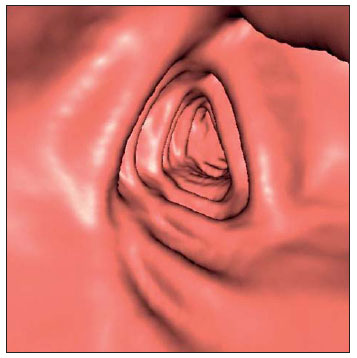 Figure 2. Normal colon. 3D endoluminal view. 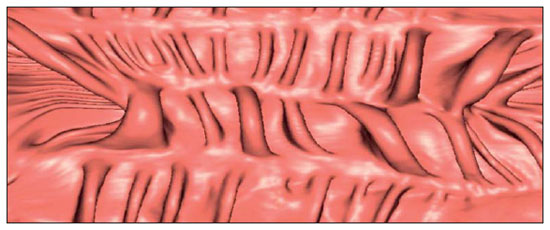 Figure 3. Colon with normal mucosal relief. CTC with virtual dissection. COMMON LESIONS Colonic polyps Most of the CRCs develop from adenomatous polyps. The minute, small and large polyps risk for malignant transformation corresponds to 0.08%, 0.7% and 15.7% respectively(3). Polyps may be either sessile or pedunculated; the first ones are most frequently found. The prevalence of polyps in the population is high and increases with age, ranging from 20% to 25% at 50 years, to 50% between 75 and 80 years of age. Recent studies on CTC describe a sensitivity of the method of up to 96% in the detection of polyps = 10 mm and 88% for polyps between 6 and 9 mm(9). At CTC, polyps present soft tissue density, with enhancement after intravenous contrast injection, and are fixed at change in decubitus (Figures 4, 5 and 6). 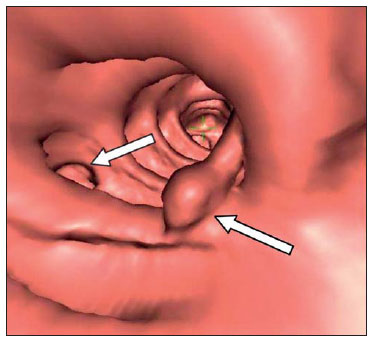 Figure 4. Pedunculated adenomatous polyp with 10 mm (right arrow) and diverticulum (left arrow). Virtual colonoscopy with endoluminal view. 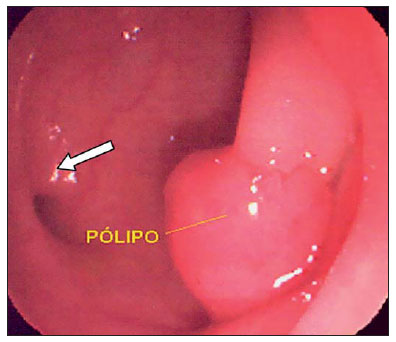 Figure 5. Pedunculated adenomatous polyp measuring 10 mm and diverticulum (arrow). Correlation with colonoscopy findings of the case presented on Figure 4. 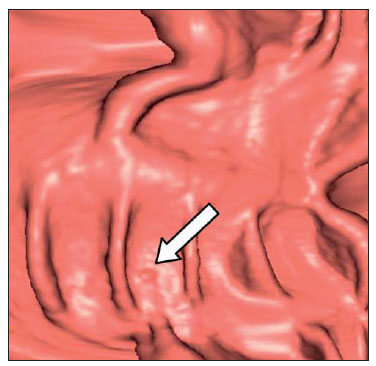 Figure 6. Minute hyperplastic polyp (arrow) in the descending colon. CTC: endoluminal view with virtual dissection. Colorectal cancer Adenocarcinoma is the most common primary malignant tumor of the colon, with 30% of the cases being found in the rectum and 20% in the sigmoid. Synchronous carcinomas are present in 5% of the cases, which increases the need to perform CTC in patients whose OCs are incomplete because of the presence of stenosing lesion (Figure 7). A periodic population screening is recommended after the age of 50. CTC presents sensitivity and specificity of 96% in the detection of CRC(3,9). An additional advantage of CTC is allowing, simultaneously, distant staging after intravenous contrast injection (Figures 8 and 9). At CTC, infiltrating CRC is characterized by asymmetrical, irregular parietal thickening that may extend to the pericolic fat and structures.  Figure 7. Synchronous cancer in transverse colon. Stenosing and infiltrative lesions (arrows). View of the colic frame at 3D CTC reconstruction. 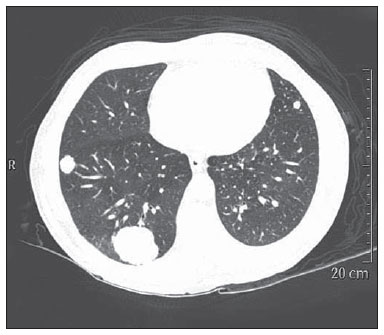 Figure 8. Pulmonary lesions with a secondary appearance at axial CTC images with pulmonary window. 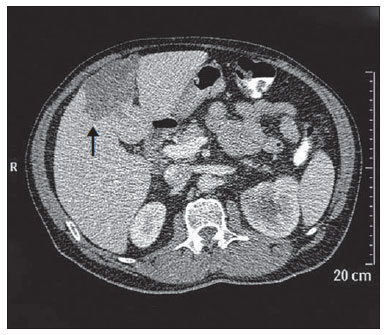 Figure 9. Secondary hepatic hypovascular lesion (arrow) observed at CTC after intravenous contrast injection in a patient with colon neoplasia. Inflammatory colorectal disease Crohn's disease and ulcerative rectocolitis are the most common inflammatory disorders. Ulcerative rectocolitis typically initiates in the rectum and extends towards the proximal colon, with inflammation restricted to the mucosa and the submucosa (Figures 10 and 11). Crohn's disease is a granulomatous inflammatory disease which may affect the whole gastrointestinal tract, but is most frequently observed in the terminal ileum and in the cecum(10). The utilization of CTC in cases of intestinal inflammatory disorders and hereditary colon syndromes is controversial and is routinely contraindicated. Notwithstanding such a controversy, CTC may be useful as an alternative strategy with a supplementary character in the diagnosis(11). 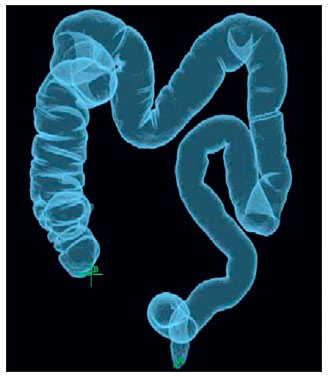 Figure 10. Ulcerative rectocolitis in the left colon with diffuse loss of haustra in transverse and descending colon. 3D CTC view of the colic frame. 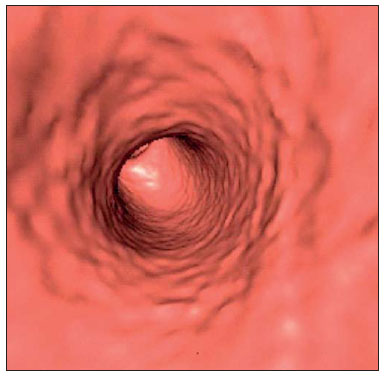 Figure 11. Ulcerative rectocolitis in the left colon with diffuse loss of haustra. Endoluminal CTC view. Colonic diverticular disease Colonic diverticular disease is the most common colonic disease, associated with diet-related factors, and may affect any part of the large bowel, but it is most commonly found in the sigmoid and very rarely in the rectum. At CTC, cases of advanced diverticular diseases are frequently observed, with segmental parietal thickening(11) (Figure 12). In order to avoid complications, CTC should be performed between four and six weeks after the conservative treatment of diverticulitis and previously performed biopsies(8,11). 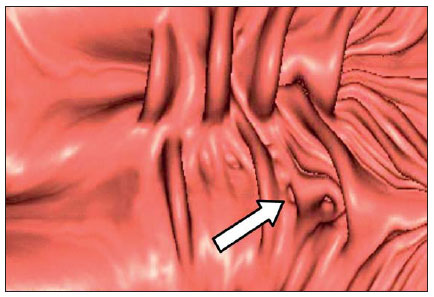 Figure 12. Colonic diverticulum (arrow). Endoluminal CTC view with virtual dissection. Intestinal lipoma Lipoma is the most common mesenchymal tumor, which develops from the submucosa and may be large, with a predominantly extraluminal appearance. The ileocecal valve is most commonly affected. The CTC allows the diagnosis confirmation based on the presence of fat content(11) (Figures 13 and 14). 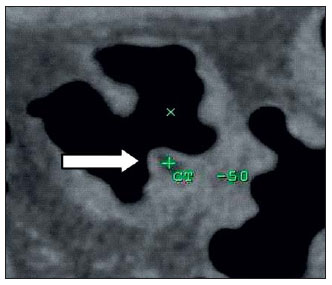 Figure 13. Lipoma simulating a polyp. Submucosal nodule (arrow) with smooth surface and negative density on axial image (UH: –50). 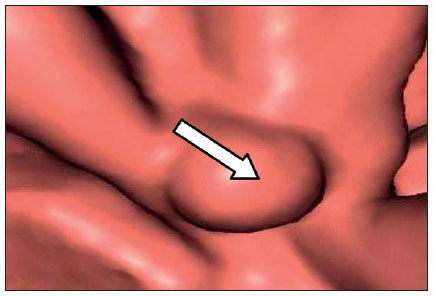 Figure 14. Lipoma simulating a polyp. Polypoid lesion with smooth endoluminal surface (arrow). Endometriosis It is estimated that 12% to 37% of the women with endometriosis also present implants in the gastrointestinal tract, with the rectum and the sigmoid colon the most affected locations(11). At CTC, endometriosis presents as a lesion with extramucosal retractile appearance and as focal intestinal wall thickening (Figure 15). The usefulness of CTC in endometriosis lies in the definition of the extent of the disease in cases where submucosal and infiltrative lesions simulating CRC are identified at OC(11). 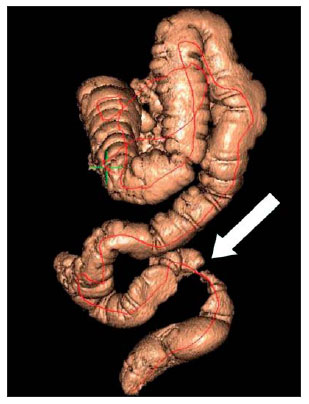 Figure 15. Deep endometriosis in the rectosigmoid transition zone (arrow). The serous implant determines focal stenosis of the loop. 3D CTC view of the colic frame. PSEUDOLESIONS Fecal residue (polypoid-like) It is the most common pseudolesion and differs from true polyps for being mobile, presenting heterogeneous attenuation and many times with intermingled gas, tending to present geometrical morphology. The bowel preparation with contrast agent ingestion is useful for labeling non-eliminated fecal residues, allowing their differentiation from true polyps(11) (Figures 16 and 17). 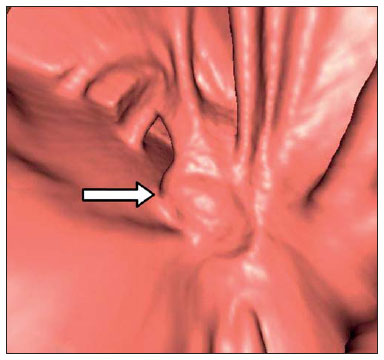 Figure 16. Fecal residue (arrow) simulating flat lesion on endoluminal view. 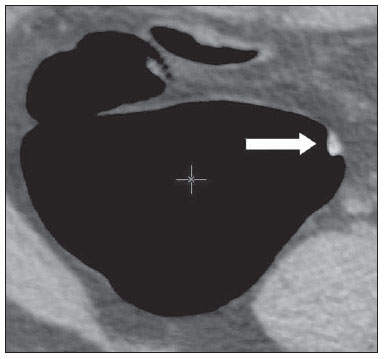 Figure 17. Barium-labeled fecal residue (arrow) simulating a polyp on axial image. Ileocecal valve Ileocecal valve is a lip-shaped structure and frequently accumulates fat, sometimes simulating polypoid lesions and lipomas(11)(Figure 18). 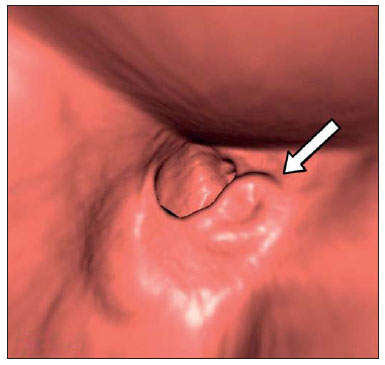 Figure 18. Normal appearance of ileocecal valve (arrow) at CTC. Endoluminal image. Appendicular stump The presence of an inverted appendicular stump after appendectomy may simulate a polyp. The typical location and coronal reformation may be useful for recognizing such pseudolesion(7) (Figures 19 and 20). 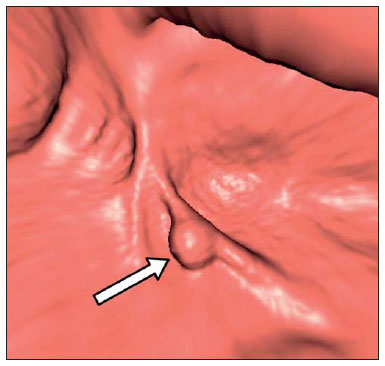 Figure 19. Appendicular stump (arrow) after appendectomy, simulating a polyp. Endoluminal view. 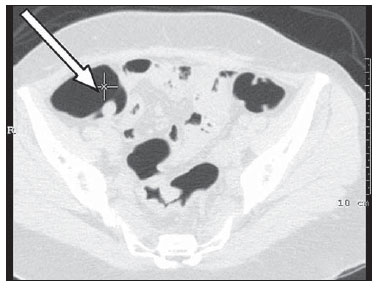 Figure 20. Appendicular stump (arrow) after appendectomy simulating a polyp on 2D axial image. CONCLUSION The technical aspects related to bowel preparation and acquisition of CTC images, as well as the knowledge of the main characteristics of lesions and pseudolesions are of utmost importance to ensure the high performance of the method in the screening for colorectal neoplasias. REFERENCES 1. Klabunde CN. Trends in the use and quality of colorectal cancer screening in the U.S. Presented at: NIH State-of-the-Science Conference: Enhancing Use and Quality of Colorectal Cancer Screening; February 2–4, 2010; Bethesda, MD, USA. 2. Levin B, Lieberman DA, McFarland, et al. Screening and surveillance for the early detection of colorectal cancer adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58:130–60. 3. Pickhardt PJ, Hassan C, Halligan S, et al. Colorectal cancer: CT colonography and colonoscopy for detection – systematic review and meta-analysis. Radiology. 2011;259:393–405. 4. Kim DH, Pickhardt PJ, Taylor AJ, et al. CT colonography versus colonoscopy for the detection of advanced neoplasia. N Engl J Med. 2007;357:1403–12. 5. Ramos O Jr, Boguszewski CL, Teixeira S, et al. Performance of computed tomographic colonography for the screening of colorectal polyp in acromegalic patients: a prospective study. Arq. Gastroenterol. 2009;46:90–6. 6. Pfeifer GK, Corleta O, Gus P. Avaliação do desempenho da colonografia tomográfica computadorizada (colonoscopia virtual) no diagnóstico de pólipos colorretais. Arq. Gastroenterol. 2008;45:301–7. 7. Mang T, Maier A, Plank C, et al. Pitfalls in multi-detector row CT colonography: a systematic approach. Radiographics. 2007;27:431–54. 8. Kim DH, Pickhardt PJ. Colonic distention for CT colonography. In: Pickhardt PJ, Kim DH, editors. CT colonography: principles and practice of virtual colonoscopy. 1st ed. Philadelphia, PA: Saunders Elsevier; 2010. p. 131–47. 9. Rosenberg JA, Rubin DT. Performance of CT colonography in clinical trials. Gastrointest Endosc Clin N Am. 2010;20:193–207. 10. Costa-Silva L, Martins T, Passos MCF. Enterografia por tomografia computadorizada: experiência inicial na avaliação das doenças do intestino delgado. Radiol Bras. 2010;43:303–8. 11. Pickhardt PJ, Kim DH. Indications of performing CT colonography. In: Pickhardt PJ, Kim DH, editors. CT colonography: principles and practice of virtual colonoscopy. 1st ed. Philadelphia, PA: Saunders Elsevier; 2010. p. 72–390. 1. MD, Fellow PhD degree of Clinical Radiology, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 2. PhD, MD, Radiologist, Abdominal Imaging Section, Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 3. MD, Radiologist, Abdominal Imaging Section, Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 4. MD, Radiologist, Fellow Master degree of Clinical Radiology, Abdominal Imaging Section Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 5. MD, Radiologist, Fellow of Abdominal Imaging Section, Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 6. Associate Professor, Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. Mailing Address: Dr. Giuseppe D'Ippolito Rua Professor Filadelfo Azevedo, 617, ap. 61, Vila Nova Conceição São Paulo, SP, Brazil, 04508-011 E-mail: giuseppe_dr@uol.com.br Received December 5, 2011. Accepted after revision February 24, 2012. * Study developed at Abdominal Imaging Section, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (Unifesp), and at Laboratório Fleury - Medicina e Saúde, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554