INTRODUCTION
The imaging evaluation of the small bowel has traditionally been performed by means of bowel transit time test, enteroclysis and computed tomography (CT). Recently, magnetic resonance imaging and capsule endoscopy have been included as alternative investigation methods(1).
Over the last years, technical developments have allowed improvement in CT evaluation of the small bowel. Among those advances, the use of multidetector row CT (MDCT) can be highlighted, with isotropic imaging allowing multiplanar evaluation, introduction of neutral oral contrast with attenuation similar to that of water(2) and techniques of contrast agents administration to increment bowel loops distention and delay its absorption by the intestinal mucosa, in addition to images acquisition oriented towards the maximum intestinal wall enhancement time(1). This set of technical factors has been called computed tomography enterography (CT enterography)(1,2).
CT enterography differs from conventional abdominal CT for the great amount of oral contrast required and thin slicing, with multiplanar reconstruction acquired by means of MDCT(1-4). The main indications for this method are the following: evaluation of obscure gastrointestinal bleeding, diagnosis and follow-up of inflammatory bowel disorders, particularly Crohn's disease, and investigation of intestinal neoplasms(1).
Neutral oral contrast agents allow a better distinction of segments with increased mural enhancement, hypervascular masses, and other inflammatory and vascular processes(3,4). Luminal distention is essential for the diagnosis of bowel disorders, since collapsed loops may obscure intraluminal disorders or mimetize wall thickening and areas of increased enhancement of bowel segments. Macari et al.(1) have considered intestinal distention as being satisfactory when the transverse diameter of the small bowel is at least 2 cm. Insufficient distention or luminal collapse may result from the short time elapsed between contrast agent intake and images acquisition, water absorption, delayed gastric emptying, or ingestion of inappropriate amount of contrast medium(3).
Multiple low-attenuation contrast agents have been studied in the literature(1- 3,5-9), namely: water, water with methylcellulose, 0.1 % barium solution with sorbitol (VoLumen
®), polyethylene glycol (PEG) (2%) solution and milk (4%). Some solutions, such as VoLumen
®, are not yet available in the Brazilian market, so it is necessary to find alternatives. Polyethylene glycol at the currently utilized concentrations (59 g/l) produces good results in terms of bowel distention, but it is not well accepted by patients, because of its side effects such as colic and diarrhea(3). Notwithstanding the several studies comparing different bowel preparations for CT enterography studies, so far no study is found in the literature comparing the three main contrast agents (milk, water and PEG), with PEG at a lower concentration and with the objective of reducing its undesirable effects, while maintaining its bowel lumen distention capability. The present study proposes the comparison between the solutions available in the Brazilian market, namely, water, whole milk and PEG solution at a lower concentration (52.5 g/l) with a view to reducing side effects and, consequently, improving the acceptance of the latter by patients.
The present study is aimed at assessing the performance of three neutral oral contrasts, comparing degree of bowel distention and bowel wall distinction, in addition to assessing the acceptance and side effects reported by patients.
MATERIALS AND METHODS
A prospective study was developed with 30 patients submitted to CT with administration of intravenous iodinated contrast and oral neutral contrast agents, divided into three groups. The study was approved by the Committee for Ethics in Research of the authors' institution and a term of free and informed consent was signed by all participating patients.
Inclusion criteria were the following: patients above 18 years of age with spontaneous requests for abdomen and pelvis CT studies with indication for utilization of intravenous and oral contrast agents. Exclusion criteria were the following: history of gastrointestinal tract surgery, known neoplasia of the gastrointestinal tract, intolerance to lactose, current intake of laxatives, tricyclic antidepressants, phenobarbital or opiates, and presence of gastrointestinal symptoms such as nausea, vomiting, diarrhea and early satiety; besides pregnancy, allergy to iodinated contrast agents and creatinine levels above 2.0 mg/dl.
The group distribution according to the utilized oral neutral contrast agents was the following: group 1 - 1000 ml of whole milk 3.2%; group 2 - 1800 ml of water; group 3 - PEG solution in 1500 ml of water; all administered over a time interval of approximately 45 minutes, representing safe alternatives according to studies in the literature(5). The utilized PEG was Muvinlax
® (PEG3350), commercially available in 13.125 g sachets. The utilized dilution was six sachets for 1500 ml of water (52.5 g/l), which is a lower concentration than that utilized in previous studies
(3,5,6). Each group of 10 consecutive patients received a different type of oral contrast agent.
All the abdomen and pelvis CT studies were performed in a 64-detector row Brilliance model apparatus (Philips Medical System; Best, The Netherlands). The studies were performed with the multislice and 3D volume rendering technique, from the diaphragm to the pubic symphysis, 65 seconds after intravenous contrast injection, at a rate of 3 ml/s, with a dose of 2 ml/kg of weight, up to a maximum of 150 ml. Technical CT parameters were the following: collimation, 64 × 0.625 mm; 0.891 pitch, 3 mm-thick slice, with 120 kVp and variable mAs, as a function of patient's abdominal thickness. Coronal and sagittal reconstructions were obtained.
The images were consensually interpreted by two radiologists with four- and ten-year experience in abdominal CT and blind to the type of oral contrast agent utilized in the study. The radiologists' analysis considered the degree of bowel distention, divided into four regions of bowel segments, as follows: left hypochondrium, mesogastrium, pelvis and terminal ileum. Each region was classified according to a scale ranging from 1 to 3, as follows: 1 - loops with a caliper < 1 cm; 2 - loops with calipers between 1 cm and 2 cm; 3 - loops with calipers > 2 cm. In addition, the radiologists classified the loop walls as visible or not, also in the four regions.
As regards the degree of acceptance of the ingested solution, the patients answered a questionnaire on the following items: flavor, on a scale ranging from 1 to 3: 1 - bad taste; 2 - reasonable taste; 3 - good taste; as regards nausea during ingestion, on a scale of 1 to 3: 1 - no nausea; 2 - mild nausea; 3 - severe nausea; and, after 24 hours, report the absence or presence of diarrhea and amount of watery evacuations.
The differences of mean ages of the groups were calculated by means of the Kruskal-Wallis test. The degree of bowel distention was evaluated according to the above described three-point scale, with the calculation of the percentage for each one of the degrees. Additionally, the calculation of the percentages of visible loop walls was obtained, and the assessment of the degree of acceptance of the contrast agent ingested by the patients followed the above described scale. The analysis of statistical significance was performed by utilizing the chi-square test, considering a 5% significance level (
p < 0.05).
RESULTS
The mean age in group 1 (whole milk 3.2%) was 59 years, while in group 2 (water) it was 60 years, and in group 3 (PEG), 53 years, with no significant difference among the three groups (
p < 0.05).
Appropriate bowel distention, with a caliper > 2 cm, was observed in 14 of the 40 studied segments (35%) in patients who ingested milk; in 10 segments (25%) in patients who ingested water; and in 23 segments (57.5%), in patients who ingested PEG. The bowel preparation with PEG resulted in the best intestinal distention (
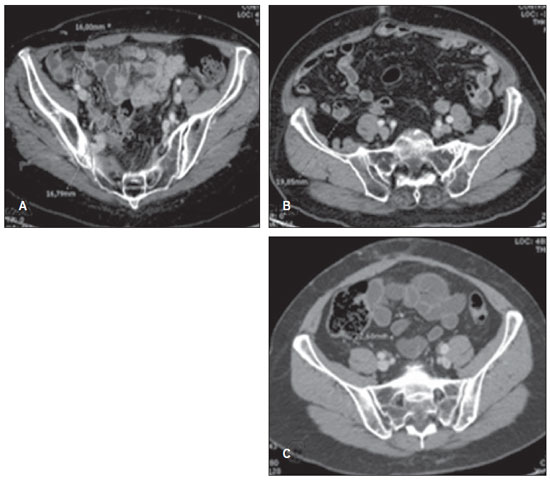
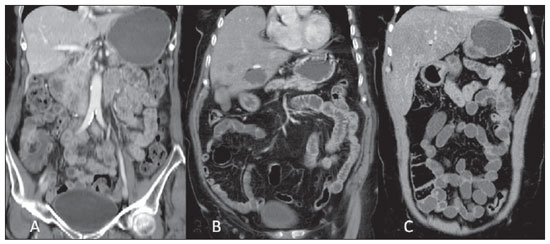
p = 0.01), with no significant difference between milk and water (Figure 1). The intestinal wall distinction was observed in 39 of the 40 studied segments (97.5%) in the milk group; in 33 segments (82.5%) in the water group; and in 38 segments (95%) in the PEG group, with no significant difference among the three groups (Figures 1 and 2).
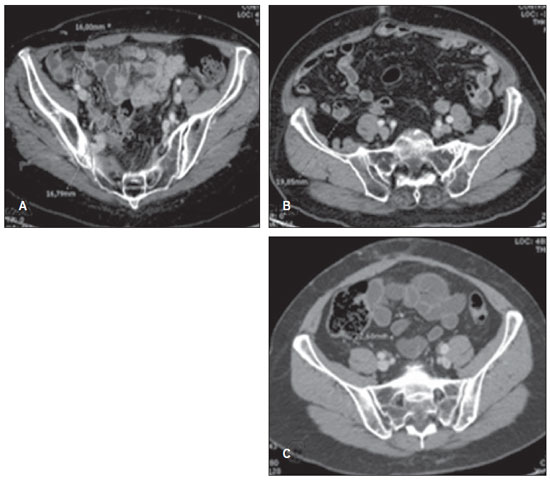
Figure 1. CT enterography with oral preparation utilizing milk (A), water (B) and PEG (C). It is possible to observe appropriate intestinal distention (small bowel distention > 2 cm) only in the study with the PEG preparation. The intestinal wall is well visualized with the three types of contrast agents.
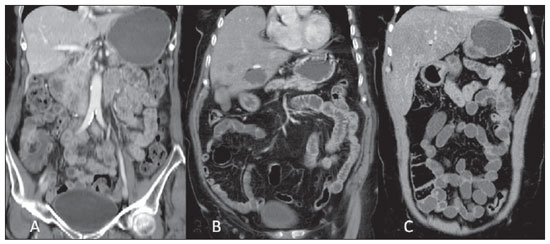
Figure 2. CT enterography coronal reconstruction with oral preparation utilizing milk (A), water (B) and PEG (C). The intestinal wall is well defined with the three types of contrast agents, but intestinal distention is best with PEG (C).
The milk flavor was considered bad by one patient (10%); reasonable by three patients (30%); and good by six patients (60%). The water flavor was considered reasonable by two patients (20%), and good by eight patients (80%). The PEG flavor was considered reasonable by eight patients (80%), and good by two (20%) patients. Nausea was reported by three patients (30%) who ingested milk; by two patients (20%) who ingested water, and also by two patients who ingested PEG, with no indication of differences. As regards diarrhea, eight patients who ingested PEG (80%) reported its occurrence while in the milk and water groups there were no reports of such an occurrence, which clearly demonstrates a tendency to a higher incidence of diarrhea with PEG than with milk or water.
DISCUSSION
CT enterography has been progressively replacing bowel transit study and enteroclysis in the imaging assessment of the small bowel as it allows the visualization of the whole bowel, without loop overlapping, as well the evaluation of the intestinal walls, detection of pathological extraluminal conditions and eventual associated findings(4,10). Additionally, such method allows the evaluation of segments which cannot be reached by traditional endoscopic methods. In general, such method provides good results in the detection of small bowel conditions, with good acceptance and tolerability by patients, besides being fast, widely available, and with high interobserver reproducibility and low rates of related complication(11). Thus, it is becoming a method with increasing utilization in the clinical and radiological practices.
As already mentioned, different neutral enteric contrasts have been utilized in CT enterography. In the present study, comparisons were made between some of the contrast agents available in the local market, such as water, milk and PEG, compared with respect to the degree of bowel distention and distinction of the intestinal wall, besides acceptance and side effects reported by the patients. The present study is the first one comparing the performance of those three neutral oral contrast agents.
Water is not considered a good contrast agent in enterography, since it is rapidly absorbed along the bowel, thus providing poor intestinal distention(1,11-13). On the other hand, a previous study has demonstrated that water was the oral contrast agent preferred by patients, and the least associated with side effects(3).
PEG is routinely utilized as a bowelcleansing agent, being widely available and considered safe for utilization in humans, besides the fact that it is not absorbed into the circulation, thus reducing the risk for systemic side effects(6). It has the property of advancing through the intestinal tract without the need for association with peristalsis stimulating drugs, with a relatively rapid transit time and no significant absorption, remaining in the small bowel lumen(5). Previous studies have demonstrated excellent distention of the small bowel loops with the utilization of PEG as compared with water(1-3,5,6). However, PEG has been associated with a higher patient's dissatisfaction because of its flavor and side effects, such as diarrhea(3,5). Even so, it is important to remind that such side effect is commonly reported after small bowel studies, particularly after small bowel transit time studies, as large amounts of liquids are injected into the bowel over a short period of time(6).
Agents containing fat in their composition, such as milk containing 4% (whole milk) or 2% fat, may also be utilized as oral contrast agent. One believes that the fat content of milk can reduce the peristalsis in the gastrointestinal tract, thus allowing luminal distention and bowel walls distinction. In a previous study, it was observed that milk 4% was superior in bowel distention and intestinal wall distinction as when compared with water and milk 2%(8). In Brazil, the available whole milk presents 3.2% fat content, and such was the milk utilized in the present study.
The present study reproduced isolated results previously published in the literature(1-3,5,6), demonstrating better bowel distention with the utilization of PEG, which allowed a higher rate of intestinal loops with calipers > 2 cm. Similarly, water presented a lower rate of segments with satisfactory distention. As regards the flavor of the ingested contrast agent, a lower acceptance of PEG was observed, but none of the patients considered its taste as being bad. As regards the incidence of diarrhea, as expected, it was significantly more frequent with PEG than with milk or water, even with the utilization of PEG at a lower concentration than that utilized by other authors(3). As regards other side effects such as nausea, for example, there was no difference in its incidence among the three groups in this study.
There were some limitations in the present study. The first one was the relatively small number of patients, which partially impaired the application of some statistical tests, but nevertheless allowed a clear identification of result tendencies. Further studies with larger samples will be necessary to confirm the present results. The second limitation refers to the fact that the amount of oral contrast agent was different among the three preparations, which may somehow influence the tolerance level of the liquid ingested by the patient. On the other hand, the method utilized for contrast agent administration was similar to the one adopted by most authors in the reviewed literature and in the clinical practice(3,5,6,8).
CONCLUSION
CT enterography is currently considered a relevant imaging method for evaluating small bowel disorders. Inflammatory bowel disorders, obscure intestinal bleeding and small bowel tumors constitute the main indications for evaluation by CT enterography. A protocol with appropriate bowel distention is required to obtain accurate diagnostic results. The present study has demonstrated that the utilization of PEG as a neutral oral contrast agent at CT enterography allows greater degree of intestinal distention, with a good level of distinction of the intestinal walls in most cases, but at the expense of a higher frequency of diarrhea and worse acceptance by patients, as compared with milk or water.
REFERENCES
1. Macari M, Megibow AJ, Balthazar EJ. A pattern approach to the abnormal small bowel: observations at MDCT and CT enterography. AJR Am J Roentgenol. 2007;188:1344–55.
2. Megibow AJ, Babb JS, Hecht EM, et al. Evaluation of bowel distention and bowel wall appearance by using neutral oral contrast agent for multi-detector row CT. Radiology. 2006;238:87–95.
3. Young BM, Fletcher JG, Booya F, et al. Head-to-head comparison of oral contrast agents for cross-sectional enterography: small bowel distention, timing, and side effects. J Comput Assist Tomogr. 2008;32:32–8.
4. Paulsen SR, Huprich JE, Fletcher JG, et al. CT enterography as a diagnostic tool in evaluating small bowel disorders: review of clinical experience with over 700 cases. Radiographics. 2006;26:641–62.
5. Hebert JJ, Taylor AJ, Winter TC, et al. Low-attenuation oral GI contrast agents in abdominal-pelvic computed tomography. Abdom Imaging. 2006;31:48–53.
6. Sood RR, Joubert I, Franklin H, et al. Small bowel MRI: comparison of a polyethylene glycol preparation and water as oral contrast media. J Magn Reson Imaging. 2002;15:401–8.
7. Koo CW, Shah-Patel LR, Baer JW, et al. Cost-effectiveness and patient tolerance of low-attenuation oral contrast material: milk versus VoLumen. AJR Am J Roentgenol. 2008;190:1307–13.
8. Thompson SE, Raptopoulos V, Sheiman RL, et al. Abdominal helical CT: milk as a low-attenuation oral contrast agent. Radiology. 1999;211:870–5.
9. Wold PB, Fletcher JG, Johnson CD, et al. Assessment of small bowel Crohn disease: noninvasive peroral CT enterography compared with other imaging methods and endoscopy – feasibility study. Radiology. 2003;229:275–81.
10. Elsayes KM, Al-Hawary MM, Jagdish J, et al. CT enterography: principles, trends, and interpretation of findings. Radiographics. 2010;30:1955–70.
11. Costa-Silva L, Martins T, Passos MCF. Enterografia por tomografia computadorizada: experiência inicial na avaliação das doenças do intestino delgado. Radiol Bras. 2010;43:303–8.
12. Fidler JL, Guimaraes L, Einstein DM. MR imaging of the small bowel. Radiographics. 2009;29:1811–25.
13. Hara AK, Swartz PG. CT enterography of Crohn's disease. Abdom Imaging. 2009;34:289–95.
1. Associate Professor, Department of Imaging Diagnosis - Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil.
2. MDs, Trainees, Abdominal Imaging Section, Department of Imaging Diagnosis - Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil.
3. MDs, Fellows, Abdominal Imaging Section, Department of Imaging Diagnosis - Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil.
4. PhD, MD, Abdominal Imaging Section, Department of Imaging Diagnosis - Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil.
Mailing Address:
Dr. Giuseppe D'Ippolito
Rua Professor Filadelfo Azevedo, 617, ap. 61, Vila Nova Conceição
São Paulo, SP, Brazil, 04508-011
E-mail: giuseppe_dr@uol.com.br
Received February 1st, 2012.
Accepted after revision May 4, 2012.
* Study developed at Department of Imaging Diagnosis - Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil.
 Vol. 45 nº 3 - May / June of 2012
Vol. 45 nº 3 - May / June of 2012