Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012
|
ICONOGRAPHIC ESSAY
|
|
Imaging findings of abdominal gossypibomas |
|
|
Autho(rs): Francisco Abaeté das Chagas Neto1; Paulo Moraes Agnollitto2; Fernando Marum Mauad3; André Rodrigues Façanha Barreto4; Valdair Francisco Muglia5; Jorge Elias Junior5 |
|
|
Keywords: Gossypiboma; Abdominal; Imaging diagnosis. |
|
|
Abstract: INTRODUCTION
The first case report about intra-abdominal foreign body after laparotomy dates back to 1884(1,2). Despite all precautions taken by surgeons and by other specialists, besides other preventive measures, postoperative intracavitary retention of foreign bodies is a relatively frequent event. Its incidence is estimated to be 0.15% to 0.2%, with one case for every 500 to 1,000 laparotomies, sometimes determining important complications, with a mortality rate of up to 10% to 18%(3—5). The term gossypiboma is utilized to describe a mass which develops from a cotton matrix surrounded by an inflammatory reaction. The word comes from the Latin gossypium (cotton) and from the Kiswahili boma (place of concealment, or hiding)(6). There are basically two types of hemostatic materials utilized in surgeries: those constituted by absorbable materials and those that are non-absorbable. Examples of non-absorbable materials are swabs, cotton and synthetic rayon synthetic gauzes, which originate gossypibomas. Absorbable materials most frequently utilized include gelatin foam (Gelfoam®), oxidized cellulose (Surgicel®, Oxycel®) and microfibrillar collagen (Avitene®), which are left in the manipulated site to avoid repeated hemorrhage. It is important to differentiate the cases that the identified foreign body is an intentional component of the surgical procedure (absorbable materials), from those involving unintentional components (non-absorbable materials)(6). Non-absorbable hemostatic materials induce two types of inflammatory reactions. The first type is an aseptic inflammatory reaction to the presence of a foreign body, with fibroblastic reaction and complete encapsulation of the process. Therefore, such type of reaction is generally asymptomatic, sometimes being identified as a palpable mass(6—8). The other is the exudative type, and frequently determines the development of an abscess, in association or not with a secondary bacterial infection(6—8). In such a type of reaction, more exuberant symptoms, such as abdominal pain and fever, are observed. Upper or lower intestinal obstruction, enterocutaneous fistulas, erosion or perforation of intestinal loops, adhesions and even granulomatous peritonitis may be associated. On the other hand, absorbable agents trigger a more controlled inflammatory reaction along the material absorption period. In most cases such a process is asymptomatic(6). Thus, gossypibomas represent a feared problem in medicine as, besides the complications to the patient, their impact on the physician-patient relationship and the medical-legal implications(7) are in both cases, very challenging. The diagnosis of gossypibomas may be extremely challenging for the radiologist because of their variable presentation, usually resulting from the investigation of complaints such as abdominal pain, palpable mass, intestinal obstruction, fistulas, or as part of routine postoperative imaging studies. In other occasions, the diagnosis results from an incidental finding, years after an abdominal surgery. Eventually, a suspicion may be raised by the clinical team that indicates imaging studies to corroborate the diagnosis of gossypiboma. Main factors involved in the occurrence of abdominal gossypibomas are the following: emergency surgeries, unexpected changes during the surgical act, two or more different teams involved in the surgical act, changes in the nursing team during the course of surgery, patient's obesity and occurrence of intraoperative hemorrhage. The early identification of such a condition is of most importance, as it results in reduction of morbidity, and may prevent potentially fatal complications, besides mitigating medical-legal complications(4,9). The present essay is aimed at demonstrating a series of typical cases of abdominal gossypibomas and illustrating their different presentations, emphasizing the findings at different imaging methods, by means of conventional radiology, ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI), with the purpose of familiarizing radiologists with this disorder and its main differential diagnoses. IMAGING EVALUATION OF ABDOMINAL GOSSYPIBOMAS Conventional radiology Conventional radiology is the imaging method most commonly utilized in the postoperative period for the detection of retained sponges or swabs (gossypibomas), which, in most cases, can be identified by the presence of radiopaque markers incorporated in their composition, with a sensitivity above 90% in such cases (Figures 1A and 2)(10). 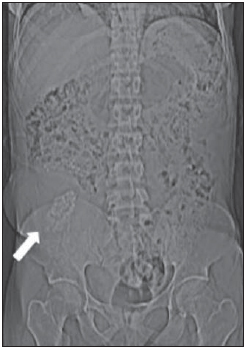 Figure 1A. Female, 35-year-old patient submitted to renal transplantation, complaining of bulging and pain in the right iliac fossa in the late postoperative period. Digital radiography (scanogram) showing bulging on the right lower quadrant associated with hyperdense linear serpiginous image on a projection of the right iliac fossa (arrow). 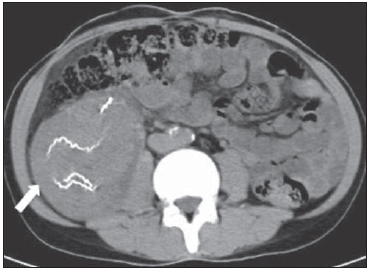 Figure 1B. Pre-contrast axial CT section of the abdomen demonstrating a mass with soft tissue density with hyperdense serpiginous structures inside (arrow). 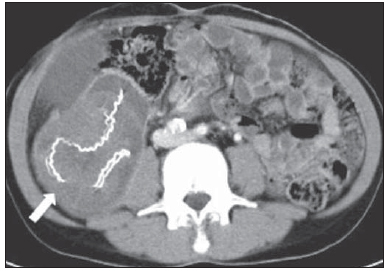 Figure 1C. Contrast-enhanced axial CT section demonstrating capsular reinforcement (arrow). 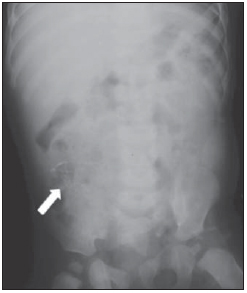 Figure 2. Male, one-year-old patient submitted to surgical correction of imperforate anus, progressing with pain and bulging in the right iliac fossa in the late postoperative period. Presence of spontaneously hyperdense linear image, projected into the right iliac fossa (arrow). Radiographs obtained at the surgery room, by means of bedside apparatuses, technical restrictions limiting the images quality therefore, the manipulation and post-processing of the images can be helpful in certain dubious cases. The appropriateness of the field of view in the study must also be considered, as well as the careful evaluation of the periphery of the obtained image, which may include part of a gossypiboma. The imaging finding of gossypiboma at plain radiography is variable. The most common presentation includes radiodense irregular linear images, some of them serpiginous, associated or not with increase in volume and density of adjacent soft tissues. In some cases, amorphous radiolucent images are observed, probably caused by gas entrapment or secondary infection by gas-forming germs(10). However, eventually small fragments of surgical material may not include radiodense filaments, so their direct identification by X-ray emitting imaging methods is difficult. In such cases, US and MRI are extremely useful. Ultrasonography Ultrasonography allows the identification of practically all types of gossypibomas, including radiolucent gossypibomas, besides providing information on their anatomical relationships (Figure 3A). 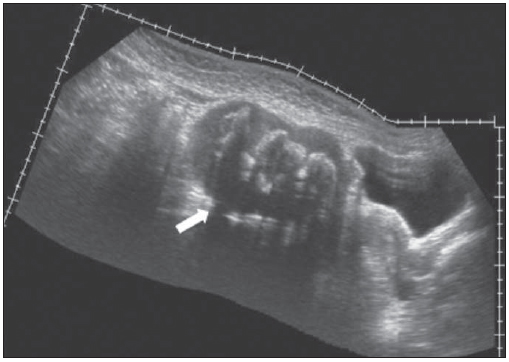 Figure 3A. Female, 25-year-old patient complaining of increased abdominal volume, and bulging in the hypogastric region. History of gynecologic surgery (tubal desobstruction) three years ago. Panoramic US, sagittal scan, demonstrating a complex mass in the hypogastric region, adjacent to the urinary bladder and the uterus (arrow). Sonographic findings in cases of gossypiboma can be divided into three types as follows: 1) hyperechogenic image with posterior acoustic shadowing; 2) well defined mass with cystic contents and echogenic, undulated internal structures; 3) non-specific finding of complex and/or hypoechoic mass. Invariably, internal vascular flow is absent at Doppler study (Figure 3B)(10—12). 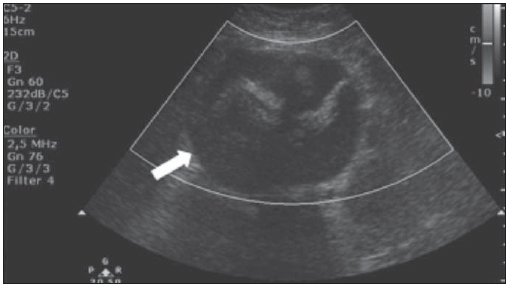 Figure 3B. Axial US section of the hypogastric region demonstrating a predominantly hypoechogenic, well defined ovoid image with mixed echotexture, associated with hyperechogenic linear foci and posterior acoustic shadowing, without internal vascular flow detectable at the Doppler study (arrow). Posterior acoustic shadowing is generally present and may be related to the attenuation of the acoustic beam by the foreign body itself, as well as by the presence of gas and, occasionally, by the presence of calcified areas(10—12). Some studies in the literature suggest that US may be considered the imaging method of choice for the diagnosis of gossypibomas, since it does not rely on ionizing radiation, presents high sensitivity (between 95% and 98%) and can be useful in the differential diagnosis with other types of postoperative complications(10—12). However, US presents some limitations, such as being operator-dependent, besides the possibility of not identifying foreign bodies at greater depths or located posteriorly to gas containing hollow viscus. Also, it may present false-positive results in cases where scars and calcifications of other etiologies are present. Computed tomography At CT, gossypibomas are generally identified as a mass with well defined contours, with soft tissues density, high or even mixed densities, sometimes containing air bubbles and high density capsule that may presents enhancement in the post-contrast phase (Figures 1B, 1C, 3C and 4)(10,12—14). 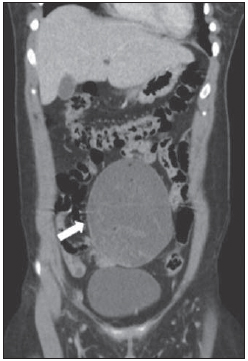 Figure 3C. Coronal reformatation of contrast-enhanced abdominal CT showing predominantly hypodense mass in the hypogastric region, with linear hyperdense images inside and adjacent to the urinary bladder, with some small hypoattenuating foci (gas) inside and subtle capsular enhancement (arrow). 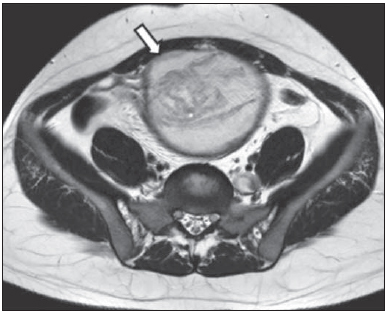 Figure 3D. Axial MRI T2-weighted section demonstrating the presence of an intra-abdominal, complex, well delimited, expansile cystic lesion, with low signal capsule, containing serpiginous linear images with intermediate signal inside (arrow).  Figure 3E. Paramedian sagittal abdominal MRI, T2-weighted section demonstrating the relationship between complex abdominal cystic lesion and the bladder (arrow).  Figure 3F. Paramedian sagittal, contrast-enhanced abdominal MRI, T1-weighted section demonstrating the capsular reinforcement of the lesion (arrow). 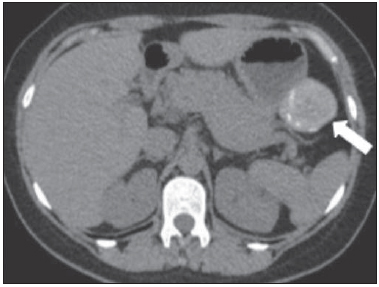 Figure 4. Asymptomatic, female, 39-year-old patient submitted to partial gastrectomy for gastrointestinal stromal tumor, in the late postoperative period. Axial, non-contrast-enhanced CT demonstrating a circumscribed ovoid lesion with soft tissue density and internal hyperdense linear structures (arrow). Sterile gas bubbles may be identified next to the gossypiboma up to six months after surgery(10). However, the presence of gas densities within the gossypiboma should alert the radiologist to the possibility of associated infection (Figure 3C). The CT scout image or scanogram must always be evaluated as many times it holds the key for a correct diagnosis, particularly in those cases where beam hardening artifacts impair the identification of the radiopaque marker on tomographic sections. Gossypibomas should not be confused with a fluid collection, in spite of the possibility of association with the development of abscess. Multidetector CT (MDCT) allows reformation of images acquired in different planes, including oblique ones, besides three-dimensional reconstruction, providing the method with extremely high sensitivity and accuracy. However, the utilization of ionizing radiation and iodinated contrast media constitute limiting factors in this method that should be taken in consideration. The tomographic differentiation between hemostatic absorbable and non-absorbable materials lies in the fact that the latter present a radiopaque marker that is not present in the several absorbable materials. However, the clinical team members interaction and the knowledge on the utilized surgical techniques are determinants of an appropriate interpretation of postoperative images. Magnetic resonance imaging Few experimental studies on the utilization of MRI for the detection of gossypibomas are found in the literature. However, in some studies, such method seems to present a sensitivity close to 100%(6,10). Also, there are reports describing cases of patients with retained gossypibomas, submitted to other diagnostic modalities such as plain radiography and CT, in whom only MRI was capable of identifying them, or was utilized as a complementary diagnosis method(10,11,15,16). Therefore, MRI should be utilized only in those cases where other more easily available imaging methods have not been capable of identifying direct or indirect signs suggestive of gossypibomas, or in those cases where those methods were inconclusive. Gossypibomas appearance at MRI is varied, being most commonly identified as a heterogeneous mass, sometimes presenting a solid-cystic component, with well defined contours, surrounded by a well delimited capsule. Hyposignal and hypersignal predominate respectively on T1-weighted and T2-weighted images, including internal serpiginous and irregular images with intermediate signal on both T1- and T2-weighted imaging (Figures 3D, 3E, 3F, 5A and 5B)(6,10,11,15,16).  Figure 5A. Female, 53-year-old patient presenting a palpable mass in the mesogastric region. History of previous abdominal surgery for colon adenocarcinoma. Coronal MRI, T2-weighted section demonstrating ovoid, circumscribed lesion with heterogeneous signal intensity, located in the mesogastric region (arrow).  Figure 5B. Coronal MRI T1-weighted section demonstrating the same lesion identified on Figure 5A, with predominant intermediate signal intensity (arrow). The capsule usually presents with low signal intensity on all pre-contrast sequences, and may or may not present enhancement on the sequences after administration of paramagnetic contrast agent (Figures 3F and 5C)(6,10,11,15,16). 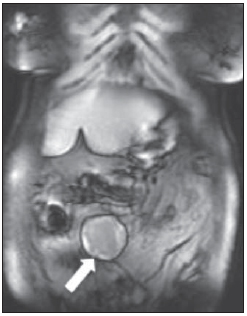 Figure 5C. Coronal MRI T1-weighted section acquired after intravenous gadolinium administration, demonstrating a low signal capsule, with no sign of contrast uptake (arrow). DIFFERENTIAL DIAGNOSIS The main differential diagnoses of gossypibomas include intra-abdominal expansile masses/lesions such as hematomas, abscesses/collections, neoplastic lesions and fecalomas(17). Hematomas are seen in the early postoperative period and in general present progressive resorption at follow-up studies. Abscesses are visualized as fluid density masses with well defined walls with capsular reinforcement. In some cases, gas may be identified within the lesion, producing air-fluid level. However, the development of an abscess may occur as a complication related to the presence of a gossypiboma. Neoplastic lesions simulating gossypibomas are in general identified as an abdominal palpable mass in asymptomatic patients or in patients with non specific abdominal complaints associated with a previous history of abdominal surgery. In cases of oncologic surgery, the differentiation between residual lesion, tumor recurrence and gossypiboma may represent a diagnostic challenge to radiologists. Fecalomas may present irregular contours and poorly defined limits at CT, but are located inside colon loops and do not present a well defined and thick capsule. Other conditions, such as postoperative adhesions, intestinal invagination, mesenteric panniculitis and retained absorbable hemostatic materials should be remembered and considered among diagnostic possibilities(18). CONCLUSION Imaging findings of gossypibomas have variable presentations; however their diagnosis may be suggested in cases where there is a correlation with a history of previous abdominal surgery, and should be considered among the differential diagnosis of abdominal masses/collections. In the suspicion of gossypiboma, imaging findings should be impartially and objectively reported by the radiologist. However, the knowledge on the utilized surgical techniques is necessary in order to allow the radiologist differentiating between intentionally implanted materials/absorbable hemostatic materials and gossypibomas. Thus, the radiologist must have the knowledge on the different usual presentations of gossypibomas and be prepared to interact with the assisting medical team in order to propose strategies that can better support the specific diagnostic and therapeutic approaches for the patient. REFERENCES 1. Iglesias AC, Salomão RM. Gossipiboma intra-abdominal — análise de 15 casos. Rev Col Bras Cir. 2007;34:105—13. 2. Mafalda LG, Caitano MJC, Magioni FM, et al. Textiloma simulando tumor de cólon e mesentério, assintomático durante 40 anos. ABCD Arq Bras Cir Dig. 2009;22:186—7. 3. Rappaport W, Haynes K. The retained surgical sponge following intra-abdominal surgery. A continuing problem. Arch Surg. 1990;125:405—7. 4. Gawande AA, Studdert DM, Orav EJ, et al. Risk factors for retained instruments and sponges after surgery. N Engl J Med. 2003;348:229—35. 5. Gonzales-Ojeda A, Rodríguez-Alcantar DA, Arenas-Marquez H, et al. Retained foreign bodies following intra-abdominal surgery. Hepatogastroenterology. 1999;46:808—12. 6. Martins MCB, Amaral RPG, Andrade CS, et al. Características de imagem na ressonância magnética de gossipiboma intracraniano: relato de caso e revisão da literatura. Radiol Bras. 2009;42:407—9. 7. Schanaider A, Manso JEF. Corpos estranhos provenientes de acessos cirúrgicos à cavidade abdominal: aspectos fisiopatológicos e implicações médico-legais. Rev Col Bras Cir. 2006;33:250—5. 8. Olnick HM, Weens HS, Rogers JV Jr. Radiological diagnosis of retained surgical sponges. JAMA. 1955;159:1525—7. 9. Kaiser CW, Friedman S, Spurling KP, et al. The retained surgical sponge. Ann Surg. 1996;224:79—84. 10. O'Connor AR, Coakley FV, Meng MV, et al. Imaging of retained surgical sponges in the abdomen and pelvis. AJR Am J Roentgenol. 2003;180:481—9. 11. Zbar AP, Agrawal A, Saeed IT, et al. Gossypiboma revisited: a case report and review of the literature. J R Coll Surg Edinb. 1998;43:417—8. 12. Malik A, Jagmohan P. Gossypiboma: US and CT appearance. Indian J Radiol Imaging. 2002;12:503—4. 13. Ariz C, Horton KM, Fishman EK. 3D CT evaluation of retained foreign bodies. Emerg Radiol. 2004;11:95—9. 14. Kalovidouris A, Kehagias D, Moulopoulos L, et al. Abdominal retained surgical sponges: CT appearance. Eur Radiol. 1999;9:1407—10. 15. Sugimura H, Tamura S, Kakitsubata Y, et al. Magnetic resonance imaging of retained surgical sponges. Case report. Clin Imaging. 1992;16:259—62. 16. Matsuki M, Matsuo M, Okada N. Case report: MR findings of a retained surgical sponge. Radiat Med. 1998;16:65—7. 17. Pelandré GL, Djahjah MC, Nobre LF, et al. Aspectos tomográficos do tumor estromal gastrintestinal de origem gástrica: estudo de 14 casos. Radiol Bras. 2008;41:297—303. 18. Brandão EM, Batista TP, Silva Junior JJ, et al. Paniculite mesentérica pseudotumoral: aspectos tomográficos de um caso. Radiol Bras. 2010;43:59—61. 1. MD, Radiologist, Fellow MSc degree, Program of Health Sciences applied to the Locomotor System, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRPUSP), Ribeirão Preto, SP, Brazil. 2. MD, Resident, Division of Radiology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRPUSP), Ribeirão Preto, SP, Brazil. 3. MD, Physician Assistant, Division of Radiology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRPUSP), Ribeirão Preto, SP, Brazil. 4. MD, Radiologist, Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto DA- Universidade de São Paulo (HC-FMRPUSP), Ribeirão Preto, SP, Brazil. 5. Professor, PhDs, Division of Radiology, Department of Medical Practice, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRPUSP), Ribeirão Preto, SP, Brazil. Mailing Address: Dr. Francisco Abaeté das Chagas Neto Secretaria do Setor de Radiologia (CCIFM) – Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo Avenida Bandeirantes, 3900, Campus Universitário, Monte Alegre Ribeirão Preto, SP, Brazil, 14048-900 E-mail: abaeteneto@yahoo.com.br Received November 7, 2011. Accepted after revision January 18, 2012. Study developed at Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HC-FMRPUSP), Ribeirão Preto, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554