Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011
|
CASE REPORT
|
|
Basal sphenoethmoidal encephalocele in association with midline cleft lip and palate: case report |
|
|
Autho(rs): Maurus Marques de Almeida Holanda1; Artur Bastos Rocha2; Rayan Haquim Pinheiro Santos2; Paulo Germano Cavalcanti Furtado3 |
|
|
Keywords: Encephalocele; Cleft palate; Congenital malformation. |
|
|
Abstract: INTRODUCTION
Sphenoethmoidal meningocele is a congenital defect of the anterior cranial fossa with herniation of meninges and, eventually, of parts of the brain (encephalomeningocele), determining a protrusion toward the nasal cavity through a defect in the ethmoid and sphenoid sinus. Such a condition corresponds to a subtype of basal meningoencephalocele(1). Different classification have been proposed for the anterior cranial fossa encephaloceles that, in a simplified way, are divided into two major groups, according to the herniation topography. The first group includes sincipital (frontal) encephaloceles where the cranial contents herniate through the foramen cecum over the cribriform plate of the ethmoid. The second group includes basal encephaloceles with protrusion through the cribriform plate itself or through the sphenoid body(2). General encephaloceles prevalence is estimated to occur in one of every 35,000 to 40,000 live neonates. The basal presentations, that are even more rarely found, represent only 2% to 10% of such encephaloceles( 3,4). Considering the rarity of this malformations association, whose treatment leads to high morbidity and mortality, and with few reports in the literature, the authors analyze the clinical and radiological findings of the present case of have cranial dysraphism. CASE REPORT A female, nine-year-old child presenting midline cleft lip and palate, hypertelorism, low height/weight development and normal intellectual development. Examination of the oral cavity, demonstrated a wide cleft palate that allowed direct visualization of a round, pulsatile cystic mass, with a brownish color, regular and smooth surface, measuring about 4 cm in diameter, located on the nasal cavity midline (Figure 1). Free and informed consent was obtained from the child’s mother, and the Research Ethics Committee has approved the present study publication. 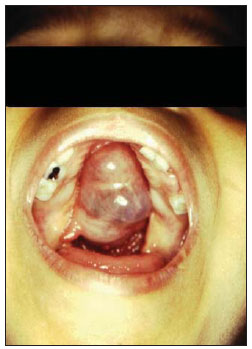 Figure 1. Basal sphenoethmoidal encephalocele. Visualization of a pulsatile cystic mass through the wide cleft palate. Computed tomography (CT) demonstrated metopic suture diastasis characterizing hypertelorism, and an empty sella turcica occupied by a cystic image. Magthrough Magnetic resonance imaging (MRI) demonstrated fluid density in the anterior region of the skull base, showing ethmoid and sphenoid defect on the midline with nasal extension, besides a hard palate defect (Figures 2 and 3). 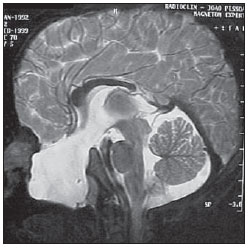 Figure 2. MRI, sagittal section demonstrating image with fluid density in the anterior region of the skull base (T2). 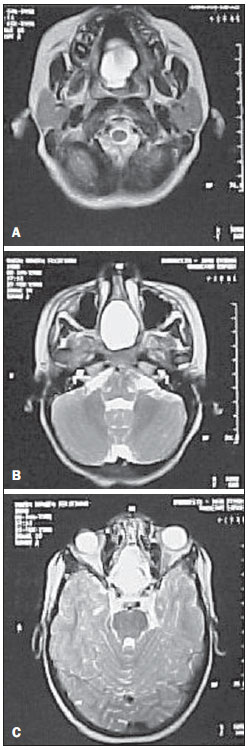 Figure 3. MRI, axial section demonstrating showing ethmoid and sphenoid defect on the midline with nasal extension, besides a hard palate defect (T2). The patient’s chronological age was nine years, while her osseous age was five years. Basal human growth hormone (HGH) levels after clonidine treatment was 0.2 ng/ml (reference: 0 to 10 ng/ml). DISCUSSION Data reporting such defects association are scarce in both the Brazilian and foreign literatures. Geographic and racial factors influence both the frequency of this condition and the encephalic area to be involved, showing endemic levels in the Southern Asia. At two health centers in Bangkok, Thailand, in the period from 1992 to 1996, 120 cases of frontoethmoidal encephalomeningocele (sincipital). However, the basal presentation is rarely observed in all of the racial groups(5). Clinically, basal encephaloceles may manifest as a mass on the nasal cavity midline causing, or not, obstruction, feeding difficulties, cerebrospinal fluid leakage and meningitis. Such a condition may be associated with cleft lip and palate, microphthalmos, bifid nose and optic nerve coloboma.Considering the presence of a nasal mass, glioma, dermoid cyst and polyp should be taken into consideration in the differential diagnosis(1). Advanced imaging studies are extremely necessary both to confirm de diagnosis and to analyze the hernial sac contents. Noncontrast- enhanced skull CT with 3D reconstruction is important to assess the skull base defect, and RMI plays a critical role in the analysis of the hernial sac elements(4). In the present case, preoperative MRI played a key role, providing valuable information such as the location of vital structures within the hernial sac. Only cerebrospinal fluid was observed within the hernial sac, without the presence of cerebral structures, rigorously characterizing a basal meningoceles. The empty sella turcica explains the hypothalamic-hypophyseal failure that may be present in 60% of cases(6). Additionally, MRI has been largely utilized in the intrauterine diagnosis of central nervous system anomalies for its higher sensitivity as compared with ultrasonography( 7,8). The prognosis, in such cases, is reserved. Only a little more than half of treated cases present a favorable evolution. In a study including 114 patients, 59% have presented normal development, 18% have presented some degree of physical or mental deficiency, and 23% have a severe deficiency( 2). Additionally to the rarity of the present case, it is important to highlight the high índex of morbidity, mortality and risk for extremely severe complications in cases where the condition is equivocally diagnosed as a dermoid cyst or nasal polyp and the surgeon inadvertently attempts to perform its resection. REFERENCES 1. Hoving EW. Nasal encephaloceles. Childs Nerv Syst. 2000;16:702–6. 2. Macfarlane R, Rutka JT, Armstrong D, et al. Encephaloceles of the anterior cranial fossa. Pediatr Neurosurg. 1995;23:148–58. 3. Monteiro M, Albuquerque AC, Nobre MC, et al. Meningoencefalocele transesfenoidal transpalatina. Arq Neuropsiquiatr. 2006;64:624–7. 4. Rathore YS, Sinha S, Mahapatra AK. Transsellar transsphenoidal encephalocele: a series of four cases. Neurol India. 2011;59:289–92. 5. Rocha LCM, Genes M. Disrafismo craniano – encefaloceles. Prat Hosp. 1989;4:6–16. 6. Lees MM, Hodgkins P, Reardon W, et al. Frontonasal dysplasia with optic disc anomalies and other midline craniofacial defects: a report of six cases. Clin Dysmorphol. 1998;7:157–62. 7. Peruzzi P, Corbitt RJ, Raffel C. Magnetic resonance imaging versus ultrasonography for the in utero evaluation of central nervous system anomalies. J Neurosurg Pediatr. 2010;6:340–5. 8. Rosen H, Chiou GJ, Stoler JM, et al. Magnetic resonance imaging for detection of brain abnormalities in fetuses with cleft lip and/or cleft palate. Cleft Palate Craniofac J. 2011;48:619–22. 1. PhD, Neurosurgeon, Associate Professor of Neurology at Universidade Federal da Paraíba (UFPB), João Pessoa, PB, Brazil. 2. Graduate Students of Medicine at Universidade Federal da Paraíba (UFPB), João Pessoa, PB, Brazil. 3. Associate Professor of Pediatric Surgery, Department of Pediatrics/Genetics, Universidade Federal da Paraíba (UFPB), João Pessoa, PB, Brazil. Mailing Address: Dr. Maurus Marques de Almeida Holanda Rua Borja Peregrino, 191, Torre João Pessoa, PB, Brazil, 58040- 050 E-mail: maurusholanda@hotmail.com Received April 18, 2011. Accepted after revision May 31, 2011. * Study developed at Universidade Federal da Paraíba (UFPB), João Pessoa, PB, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554