Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011
|
REVIEW ARTICLE
|
|
Impact of radiotherapy on the orofacial region and management of related conditions |
|
|
Autho(rs): Ana Emília Holanda Rolim1; Lino João da Costa2; Luciana Maria Pedreira Ramalho3 |
|
|
Keywords: Head and neck tumors; Radiotherapy; Acute effects; Late effects. |
|
|
Abstract: INTRODUCTION
Radiotherapy is a treatment modality that relies on the utilization of electromagnetic or corpuscular ionizing radiation capable of interacting with tissues for treatment of malignant neoplasias. The electrons move through the tissues, ionizing the medium and causing chemical and biological effects, such as damage to DNA, impairing the replication of neoplastic cells(1). However, the ionizing treatment is not selective, and also affects healthy cells, which makes it toxic for the organism(2). The radiation dose is measured in gray (Gy) and patients with head and neck carcinoma generally receive between 50 and 70 Gy (1 Gy = 1 J/kg = 100 rads) as curative dose. Such a dose is generally fractionated over a period of five to seven weeks, once a day, five days a week with a daily dose to the tumor of approximately 2 Gy(3,4). With doses as low as 10 Gy, side effects are already noticeable (cutaneous radiation syndrome, mucositis and glandular changes)(4). High radiation doses may cause hypoxia, decrease in blood supply, necrosis and susceptibility to infection. The irradiation field skin may develop the following sequelae: erythema, desquamation, development of blisters, necrosis, and also pain and burning. In the buccal mucosa, besides histophysiological changes, structural and functional changes may also occur in the support tissues(5). The most frequent systemic complications occur in 65% to 100% of the cases and are characterized by the presence of malaise, nausea, occasional vomiting, anorexia and fatigue(2). The aim of this present updated literature review is to describe the action of radiotherapy on neoplastic oral lesions, its indications, describing biological mechanisms, side effects, current treatment protocols, and to promote a better clinical approach by the dental surgeon in the assistance to such irradiated patients. MATERIALS AND METHODS Updated literature review was undertaken covering articles approaching the theme at the following data bases: Bireme, Medline, Cancerlit, Scirus, Portal Capes, SciELO, Medscape, PubMed. The following descriptors were utilized in the search for publications: oral mucositis, radiotherapy, stomatitis, neoplasm, xerostomia, osteoradionecrosis, candidiasis, cancer, dentistry, laser therapy, LLLT, head and neck tumors, sequelae. Searches with the same descriptors in Portuguese were also undertaken. One hundred scientific papers published in the period from 1985 to 2011 were retrieved for analysis. After exploratory reading and critical analysis of all the articles, 59 were excluded, either for presenting methodological limitations or for being published before 2000, without a high number of citations. Thus, 41 studies were selected for analysis, including books, reviews, case studies, multicentric clinical trials and publications by Instituto Nacional de Câncer and by the Cancer Prevention Research Institute of Texas. Most of these references corresponded to the period from 2000 to 2011, in the English and Portuguese languages, published in national and international journals. Exceptionally, five articles published in the English language by highly regarded journals before 2000, which presented a number of citations above three, were included. Besides two reference books, seven articles were written in the Portuguese language and published in Brazilian journals. The collected data were organized on a Microsoft Office Excel worksheet, version 2003, including: the reference, year of publication, number of citations; type of study, main interventions for prevention and treatment of sequelae of radiotherapy according to the findings in the literature review; and presentation of the interventions most recommended by the authors. LITERATURE REVIEW Radiotherapy causes chemical, physical and biological changes at cellular level, by direct action and obliteration of local microcirculation. The positive effect of such a therapy depends on the repair, repopulation, redistribution and reoxygenation capacity of the cells, tissues and organs. Thus, the side effects vary according to each individual's capability of biological response and depend on the irradiated area extent, radiation dose delivered, type and radio-sensitivity of the healthy tissue involved by the radiation, dose fractioning, age and systemic condition of the patient. Additionally, other modifying factors must be considered, such as alcoholism and smoking, and mainly the situations that might compromise the oral mucosa integrity, such as a poorly adapted prosthesis, dental caries and pre-existing periodontal disease, deficient hygiene habits, status of previous restorations and endodontic treatments, patient awareness and cooperation during radiotherapy treatment(2,6). Deleterious effects of radiotherapy may occur immediately during treatment and/or months or even years after its conclusion. The most frequent effects and acute symptoms of head and neck radiotherapy are the following: dysphagia, odynophagia, mucositis, bleeding, presence of opportunistic infections such as candidiasis, xerostomia, dysgeusia, periodontopathy, weight loss, hoarseness and skin changes(7,8). The following late effects of treatment with ionizing radiations are highlighted: radiation caries, subcutaneous tissue fibrosis, trismus, skin and/or mucosa ulcerations, infections, cartilage necrosis, fistulas, hearing changes, ocular changes, hormonal changes (hypothyroidism), face and neck edema, pain, hair loss, upper limbs numbness and/or tingling, cervical osteomyelitis, osteoradionecrosis(6,9). PREVENTION AND MANAGEMENT OF RADIOTHERAPY SEQUELAE The necessity of maintaining the oral health of oncologic patients submitted to radiotherapy is aimed at providing such patients with better quality of life(10). The periodontium must be maintained in healthy conditions by means of routine procedures, during and after irradiation. The guidance on oral hygiene techniques, the patient's motivation and cooperation capacity are essential to achieve the best prognosis(11—13). Bruins et al.(14) have proposed a method to assess the need for dental extractions before radiotherapy. Among the criteria for such evaluation, the following may be mentioned: dental status (periodontal and endodontic conditions, presence of impacted teeth), location and role of the tooth in the oral cavity, radiation dose and periodontal disease degree(15). Patients with previous history of periodontal disease with considerable bone loss may face severe complications such as osteoradionecrosis in cases of extractions. Dental extraction is indicated before radiotherapy treatment in cases where periodontal pockets are > 6 mm or > 4 mm with grade I tooth mobility(11). The decreased blood perfusion in the irradiated tissues leads to a progressive decrease in tissue oxygenation, as well as in the immune response from the host and in the quantity and quality of saliva(8). The saliva loses its antimicrobial, buffering and remineralization potential. Thus, the development of some microorganisms is enhanced in the oral environment, among those the obligate anaerobe Porphyromonas gingivalis, which are present in irradiated patients six months after treatment. Such bacteria take part in the development of lateral periodontitis, endodontic infections, acute abscesses, anginas and facial cellulitis. Porphyromonas gingivalis induce the release of cytokines that may contribute to an ineffective local and systemic response by the host, the inflammatory condition. Dental plaque accumulation increases the severity of mucosal infections, besides predisposing to gingivitis. If the patient present low platelet count, spontaneous bleeding may occur. Additionally, septic episodes in neutropenic patients are related to the oral microbiota(16). Thus, the management of oral cavity infections is of utmost importance, as it allows the continuation of the radiotherapy itself, since the presence of uncontrolled infections is a limiting factor for the success of such therapy, and the use of antibacterial drugs is problematic for such patients. Therefore, guidance regarding appropriate oral hygiene is indispensable for such patients. Still, regarding the oral environment, amalgam restorations pose a risk as such material emits secondary radiation and lichenoid reactions may develop due to the contact between amalgam and the oral mucosa(16). As an alternative, 5 mm-thick polyvinylsiloxane protectors may be utilized in order to protect teeth with metal restorations and tongue protectors to minimize the deleterious effects of radiation(17). For such patients, therefore, treatment must be planned with a multidisciplinary and personalized approach, taking the patient's needs into consideration. Some examples of therapeutic approaches found in the literature are described below. MUCOSITIS Mucositis is characterized by oral mucosal desquamation, erythema, development of pseudomembrane and ulceration. Typically, its onset occurs seven days after the beginning of the therapy, as the radiation dose achieves 10 to 30 Gy, and it may disappear between two and four weeks after conclusion of the treatment(18). Symptoms such as pain and burning occur particularly upon ingestion of spicy and rough-textured foods, making food swallowing and oral hygiene more difficult. The increased incidence of mucositis has been related to the increase in alcohol and tobacco consumption, and is aggravated by local traumatic factors such as poorly adapted prostheses(2,19,20). The World Health Organization has established scores for grading mucositis, with grade 0 representing absence of mucositis; grade 1, erythema; grade II, presence of erythema, edema, painful ulcer in patients who are still able to eat solid foods; grade III, severe cases with oral ulcerations in patients who can only swallow liquid foods; and grade IV, as the patient is unable eat through the mouth, requiring enteral or parenteral nutritional support(1,20). Treatment Laser therapy is a recommended alternative for the management of mucositis, as the laser light stimulates cellular activity and enhances the release of macrophage growth factors, the proliferation of keratinocytes, increases the population and degranulation of mast cells and enhances angiogenesis. Such effects accelerate the injury healing process, in part because of the decrease in the acute inflammation duration. Additionally, the daily laser application reduces the intensity, severity and duration of mucositis, besides reducing the pain and the need for morphine administration(21—24). Before such a therapy, both the patient and the laser therapy parameters must be carefully evaluated, and laser applications must be avoided in tumor areas. In order to minimize the radiation effects, in the management of mucositis and xerostomia, the application of low level laser has been suggested, with a wave length of 685 nm, at a power level of 35 mW and 1 to 4 J/point, on the following sites: three points on each parotid gland; one right and one left submandibular points; two points on the jugal mucosa at left and right; one point on each side of the floor of the mouth; two points on the tongue; one point on each tonsillar pillars; and 1 point on the uvula(23). Laser therapy delivered to similar points of application (parameters: 830 nm, 15 mW, 12 J/cm2 and 2,4 J), applied on a daily basis from the first to the last day of radiotherapy, before each session during five consecutive days, has demonstrated more satisfactory results as compared with the administration of 310 mg/5 ml aluminum hydroxide, four times a day for the duration of radiotherapy(25). However, in another study with laser application in 75 oncologic patients (parameters: 660 nm, 10 mW, 2,5 J/cm2 and 0,1 J), satisfactory results in the reduction of grades III and IV mucositis have not been observed(26). Repair or elimination of all the potential irritation sources, such as sharp and fractured cusps, broken dental pins, poorly adapted prosthesis or orthodontic bands are important before radiotherapy(4). It is also important to instruct the patient to avoid hard, hot, acid and spicy foods and to always maintain proper hydration level. The use of cocoa butter lip balm is recommended(5). In some cases, it is necessary to prescribe topical anesthetics (triamcinolone acetonide; topical benzocaine or solution; 2% lidocaine hydrochloride suspension; topical lidocaine hydrochloride and prilocaine), or systemic analgesics in cases of more severe painful symptoms(27). In cases of secondary opportunistic infections, the utilization of corticoids associated with antibiotics may be necessary, such as 40 to 80 mg prednisone oral solution daily for a week; 5 ml dexamethasone, every 8 hours, for seven days, alternating with 250 mg/5 ml erythromycin mouthwashes every 8 hours for seven days(27). In cases of mucositis associated with candidiasis, the utilization of antifungal drugs is recommended as follows: nystatin suspension with the swish-and-swallow technique, four times a day; or 10 mg clotrimazole tablets five times a day; and in cases where Candida is located under a prosthesis or in the labial commissure, nystatin cream 100,000 units/g (15 g or 30 g tubes) should be applied three times a day. In cases of children, nystatin suspension, 1/2 to 3/4 table spoon for each ice cube tray is recommended to be used as popsicles or ice cubes(27). The use of 0.12% or 0.2% clorexidine solution twice a day, or 100 ml povidone/iodine solution (1:8) may be instituted as treatment. A solution comprising diphenhydramine hydrochloride (aqueous solution at 0.25%), lidocaine hydrochloride at 2%, nystatin (100,000 u/ml) and an antiacid compound (200 mg of magnesium hydroxide, 200 mg of aluminum hydroxide and 20 mg of dimethicone) at a rate of 30 ml of each component, four to six times a day, helps alleviate mucositis symptoms(2,27). Bicarbonate water (a tea spoon of sodium bicarbonate in two cups of water) every two hours, or saline water (a tea spoon of salt for 1/4 cup of water) helps reduce the mucosal irritation, increases moisture in the mouth and removes secretions and debris, being also recommended in the treatment of leukemic gingivitis(5). Such a solution may be associated with benzidamine hydrochloride for pain reduction. The utilization of cytoprotective agents is reported in literature. For example, aminophostine, 15 to 30 minutes before each radiotherapy session, for six to 7.5 weeks, stimulates the proliferation of basal cells and tissue repair(28). Satisfactory results are also noticeable with the use of silver nitrate(28), steroids, E vitamin and oral supplementation with glutamine(29—32). HYPOGEUSIA AND DYSGEUSIA Irradiation can affect the taste buds in cases where the tongue is located in the irradiation field, causing loss of taste sensation(4). Such changes start around the first or second week of irradiation, sometimes with progression up the end of the treatment. Such changes in taste sensation are affected by the decrease in salivary flow and in mucositis(33). Hypogeusia is defined as decrease or substantial loss of the four tastes, resulting from the compromising of the taste buds and also as a consequence of stomatitis and xerostomia. For most patients, the taste sensation returns in four months, however in some cases the sequelae are permanent. Dysgeusia occurs before mucositis symptoms(4). The taste buds undergo atrophy with doses around 10 Gy. The perception of the sour and bitter tastes is most commonly affected in early phases of the radiotherapy, with later changes in sweet and salty tastes perception. Such changes are transitory and reversible, with recovery of taste perception occurring between two and four months after radiotherapy(1,3,4). Treatment Because of all such changes, the patient presents weakness, malaise, dehydration, loss of appetite with a negative impact on the patient's general condition. In such cases, where the oral and systemic health are compromised, frequent patient's weight monitoring and follow-up by a nutritionist are essential(5). Preventive supplementation with zinc and copper during the whole radiotherapy period and for some time after the conclusion of the treatment may reduce dysgeusia(31,34). OPPORTUNISTIC INFECTIONS Mucositis may be aggravated by fungal (Candida albicans), viral and bacterial (Gram-positive and Gram-negative bacilli) infections. The following factors should be evaluated in patients with oral infections: presence of endocrine dysfunctions, lesions in the mucosa, poor oral hygiene, prolonged treatment with antibiotics and corticosteroids. Irradiated patients are immunosuppressed, namely, their immune system is debilitated and cannot fight microorganisms in their own oral microbiota and other opportunistic microorganisms. Decreased salivary flow reduction and poor quality of the saliva are other predisposing factors in irradiated patients(18). The local infection origin, either in the mouth or systemic, is many times caused by pre-existing periodontal or endodontic infection. In neutropenic patients, buccal candidiasis may cause fungal septicemia, with 60% of death cases being associated with pre-existing infections. Presence of ulcerative lesions of the mucosa or compromising of the gastrointestinal tract may be related to systemic fungal infection(16). Viral lesions caused by herpes infections are also commonly observed in oncologic patients undergoing treatment and may compromise not only the keratinized mucosa, but any area of the buccal mucosa(16). Treatment Fungal infections must be treated with hydrogen peroxide salt or topical anti-fungal agents such as nystatin, preferably in powder or suspension forms, with no sugar in its composition, clotrimazole, ketoconazole and chlorhexidine. More severe infections require prescription of systemic antifungal agents such as 200 mg ketoconazole once a day for up to one week after the signs and symptoms disappear, or fluconazole 100 mg per day for 7 to 14 days, or amphotericin B(27). Chlorhexidine at 0.12% may also be prescribed. Mouthwash is recommended at least 30 minutes before or after the utilization of any topical antifungal agent and of teeth brushing. It must be used twice a day for a maximum of seven days, as the prolonged use may cause changes in the oral flora, retards healing, and the alcohol may dehydrate the oral mucosa. Additionally, chlorhexidine may cause teeth and restorations staining, reduce toothpaste and nystatin effectiveness, enhance bacterial growth (Pseudomonas), present unpleasant taste and affect taste sensation(2,5). In cases of bacterial infections, the use of topical or systemic antibiotics is recommended. The utilization of hydrogen peroxide, in the form of diluted solutions (1:4) for short periods of one to two days is recommended in periodontal bacterial infections. The adverse effects of its prolonged use are the following: delayed wound healing, enamel demineralization, induction of emesis, dry mouth, thirst and discomfort, enhancement of fungi growth, and disagreeable taste(5). In cases of viral infections, particularly by herpes, in immunosuppressed adults, the use of 400 mg acyclovir, in the form of two 200 mg tablets every six hours, during five days is recommended. In children, the acyclovir dose is 30 mg/kg per day, every 8 hours, or the option for topical use every four hours, during seven days(16). Low level laser is also effective in cases of herpes at the lesion healing phase(12). XEROSTOMIA Radiation in doses between 40 and 65 Gy promotes a degenerative inflammatory reaction, particularly in the salivary glands serous acinar cells. Additionally, anxiety and depression, many times present in such patients, favor the occurrence of xerostomia(5). In patients irradiated in the regions of head and neck, the salivary flow may decrease by up to 90% or to as low as 0.3 ml/min, with the saliva becoming thick, with more organic contents, decreased transparency and yellowish. In most severe cases, the patients present the mucosa without any moisture, with impaired chewing and preparation of alimentary bolus, and consequently impaired swallowing and even impaired speech. There are changes in tasting, causing dysphagia, nutritional changes with appetite and weight loss, affecting the patient's quality of life(3). The loss of salivary function causes numerous sequelae, including: esophageal dysfunction (chronic esophagitis); greater frequency of intolerance to oral drugs and oral hygiene products; increased incidence of local/regional infection (glossitis, candidiasis, dental caries, halitosis, bacterial sialadenitis); change in pH and lower buffering capacity; decreased remineralization capacity, leading to dental sensitivity and greater susceptibility to dental caries; decrease in structural resistance of teeth due to abrasion, friction and erosion (corrosion); increased susceptibility to mucosal injury; incapacity of wearing dental prosthesis(5). Permanent xerostomia is one the most prevalent late effects(1). It is necessary to evaluate the salivary flow, by means of resting and stimulated sialometry (Table 1). 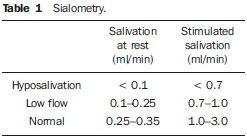 Treatment The following measures are recommended to irradiated patients with xerostomia: correct water intake (8 to 12 glasses per day), sugarless drinks, sugarless chewing gum and candies, foods rich in ascorbic acid, malic acid or citric acid, avoiding coffee, soft drinks, teas and salty foods, avoiding smoking and alcoholic drinks(31,32,34). Salivary flow tests must be performed not only previously to the radiotherapy, but also periodically to evaluate possible functional damages to the salivary glands. In irradiated patients, the control of oral microorganisms is necessary, and for such a purpose chlorhexidine gel 2%, for 5 minutes per day over 14 days promotes satisfactory results. However, in some cases, it is necessary to repeat the use every three or four months, until the salivary flow becomes normal(5,35). Artificial saliva or mouth moisturizers represent alternatives in cases of hyposalivation. They will keep the mouth pH between 6.0 and 7.0, and their composition can comprise important components for dental remineralization as follows: carboxymethylcellulose, xylitol, fluoride, amino acids enzymes, glycerol, calcium and phosphate ions(5). The systemic use of sialogogues is also an option for the treatment of most severe cases. Pilocarpine, cevimeline and urecholine may be prescribed. Pilocarpine 5 mg orally three to four times a day may be initiated one day before the beginning of radiotherapy, not exceeding 30 mg/day. The topical use of pilocarpine spray or gel should be avoided as the effects are inferior to those in systemic administration(5,13). Urecholine is an acetylcholine analogue, and a dose of 25 mg three times a day, for two to three weeks, may be prescribed. However its use should be interrupted for one week in case another sialogogue is being used. Anetholtrithione and cevimeline, 30 mg every four hours, are also systemic salivary stimulants(13). Saline solution at 0.9% (0.9 mg NaCl in100 ml of water) or a bicarbonate solution mouthwashing for 12 to 30 seconds every 6 hours or at 15-30-minute intervals, depending on the patient's need, may also be recommended(5). Acupuncture in the salivary glands for 2 to 20 minutes per week, over 6 weeks has also demonstrated acceptable results(13). Laser therapy with 685 nm wave length in a continuous form, with a power level of 35 mW, applied on three points in each parotid gland, one right and one left submandibular point, but far from tumor areas, brings positive results for patients presenting with xerostomia(23). The surgical displacement of the submandibular gland to a nonirradiated submental area is a conservative and effective approach(13). Topical and/or systemic anesthetics, anti-inflammatory and antihistaminic drugs must be prescribed after evaluation by the oncologist(5). In some cases, it is important that the patient is referred to non-pharmacological therapies for pain management. Physical activities, massotherapy, trans-cutaneous electrical nerve stimulation, acupuncture, cognitive-behavioral strategies, relaxation techniques, hypnosis, group therapy, psychosocial interventions are therapeutic alternatives that may bring improvement of the quality of life for oncologic patients(5). RADIATION CARIES From three weeks to one year after radiotherapy, caries lesions may develop, usually around the cervical margins. The absence of the salivary buffering action that regulates the oral cavity pH leads to alteration of organic and inorganic components of the teeth so as they may become more susceptible to decalcification(5). Treatment It is absolutely necessary to instruct the patient about oral hygiene, with advice about appropriate hydration and a balanced diet, with less sugar-containing foods(31). Artificial saliva containing fluoride and sialogogues, such as oral pilocarpine 5 mg, three or four times a day starting one day before the beginning of the treatment and maintained for the duration of the treatment, may be necessary to re-establish the balance of the oral microflora(5). The surgical displacement of the submandibular glands to a nonirradiated submental area preserves their function and prevents the development of xerostomia and caries(36). During radiotherapy, dental follow-up and fluoride prophylaxis must be frequent, at every 6 to 8 weeks. Restoration of incipient caries must be done after radiotherapy. The follow-up must proceed for at least 12 months or longer after radiotherapy, in cases where xerostomia persists. The daily utilization of neutral 1% sodium fluoride gel with an individual mold for 5 to 10 minutes is recommended. Acidulated gels are not recommended. Fluoride solutions at 1.0 to 1.1% once a week for one minute, or 0.05% fluoride solution twice a day, for one minute may also be utilized. Brushing with 0.4% stannous fluoride gel is also effective in cases of radiation caries, but its utilization should be avoided because of low fluoride concentration and acidic pH. Fluoride varnish (22,600 ppm of fluoride), two to three times a week may be an alternative, particularly in pediatric patients(5). Prescription of chlorhexidine gel at 1% or at 0.2%, twice a day, or chlorhexidine 0.12% solution for one minute twice a day, is also recommended to reduce the cariogenic bacterial flora(5). In such patients, preferably, one should opt for dual-curing resins or glass ionomer, avoiding amalgam restorations(5). OSTEORADIONECROSIS Osteoradionecrosis is one of the most severe complications of radiotherapy, with higher incidence in the elderly (10% to 37%), and occurs seven times more frequently in the mandible than in the maxilla, because of its higher bone density e smaller vascularization. According to Ben-David et al.(17), osteoradionecrosis may occur up to two years after the conclusion of radiotherapy. According to Thorn et al.(37), 74% of the cases occur within the first three years following radiotherapy, with higher frequency in patients who received doses above 60 Gy. The ionizing radiation results in narrowing of the vascular channels (endarteritis obliterans), which decreases the blood flow, producing an area with low resistance to trauma and with difficult regeneration capability, as there is also a decrease in viable osteocytes and osteocytes in the affected bone. The presence of periodontal or endodontic disease prior to radiation favors the access of buccal cavity microorganisms to systemic areas and bone necrosis(38). In cases of osteoradionecrosis, bone cells and vascularization may be irreversibly injured. Additionally, the risk for osteoradionecrosis remains indefinitely after irradiation(8). In chronic osteonecrosis, mixed anaerobic infections may occur, with prevalence of some types of bacteria such as Aggregatibacter actinomycetemcomitans, Fusobacterium, Parvimonas and Staphylococcus, originated from endodontic and periodontal infections(1,8). In general, extractions must be performed at least two weeks before the radiotherapy and at least one year after the conclusion of the treatment. There is a greater risk for osteoradionecrosis during radiotherapy in cases where the involved tooth is in the path of the radiation beam(17). The risk for post-extraction osteoradionecrosis is higher as the tumor and the extraction are located in the mandible, with doses higher than 5,000 cGy, particularly in patients with periodontal disease, poor buccal hygiene and in the elderly(2). In cases with dubious or poor prognosis, patients must have antibiotic coverage from the day before surgery up to the cicatrization is completed(15). Patients who utilize bisphosphonates, particularly zoledronic acid, present a greater risk for osteoradionecrosis(5). For that reason, traumatic dental procedures such as extractions, scaling and prosthesis installation must be carefully planned. Post-radiotherapy extractions must be carefully performed, with minimum mucoperiosteal detachment and alveoloplasty, without filling the alveolus and with appropriate suture(39). It is important to assess the risk for odontogenic infection in oncologic patients. For such reason, the patient's complete blood count must be evaluated. In case the leucocytes count is > 3,500 cells/mm3, and platelets count is > 100,000 cells/mm3, clinical procedures will be safer. However, in case of leukopenia or thrombocytopenia, it is necessary to evaluate the need for dental intervention in hospital environment, with platelet transfusion5 as the number of platelets is < 50,000 cells/mm3. Treatment Hyperbaric oxygenation is a treatment modality that improves healing of affected areas, enhancing angiogenesis and reducing free radicals. In some cases, 25 sessions with 90 minutes each are recommended(2). It is recommended to contact the oncologist for the interruption in the use of biphosphonates in those patients requiring extractions(5). In the treatment of osteoradionecrosis, the antibiotic association of amoxicillin, clavulanate and metronidazole is prescribed, for 10 days. Additionally, daily local irrigation with 0.2% chlorhexidine is necessary. Debridement and complete resection of the necrotic area and reconstruction with new antibiotic therapy should be carefully considered(5,17). PERIODONTAL DISEASE The periodontium, like all other tissues, is also sensitive to the effects of high radiation doses(40). The blood vessels, not only in the periodontium but also in the periosteum, are affected. Radiographically, changes in the alveolus such as periodontal ligament space widening and trabecular bone destruction are observed. Such changes increase the risk for periodontal disease, as there is a decrease in the capacity of bone repair and remodeling(4). Additionally, xerostomia and immune suppression lead to changes in the overall bacterial flora of the oral cavity, enhancing the growth of gram-negative bacteria (Streptococcus mutans, Lactobacilos and Actinomyces naeslundi, P. gingivalis)(8). Patients who present thrombocytopenia (< 30,000/mm3) cannot perform effective brushing and flossing, because of the risk for hemorrhage. In such cases, the utilization of cotton swabs or gauze with saline solution and mouth rinsing with antiseptic solutions are recommended for the removal of bacterial plaque. Dental and periodontal assessment as a pre-radiotherapy step is critical for the patient's prognosis. The literature is controversial about the appropriate period for teeth extraction. In teeth with periodontal pockets > 4 mm and/or grade I mobility(16), or with periodontal pockets > 6 mm and furcation involvement, with the tooth close to the irradiation field, high radiation doses, poor oral hygiene and poor patient cooperation(14), are indicative factors for pre-radiotherapy extraction in order to avoid osteoradionecrosis. Treatment Appropriate guidance on oral hygiene before and after radiotherapy is of utmost importance, particularly for patients with periodontal disease before the radiotherapy treatment. Scaling and root planning procedures should be instituted preferably either before or after radiotherapy(11). The removal of factors causing plaque accumulation, such as poorly adapted prosthesis, restorations excess, root fragments, fractured teeth, cavitated caries lesions, as well as extraction of teeth with major periodontal compromising, must be performed before radiotherapy. The reconstructive treatment of periodontal disease by means of the utilization of bone grafts may be performed before radiotherapy(38), but it should be carefully planned to avoid osteoradionecrosis. Laser therapy is a complementary alternative and should preferably be performed before radiotherapy(41). TRISMUS Trismus is a sequel whose onset generally occurs between the third and sixth weeks after conclusion of radiotherapy treatment and that limits buccal opening, impairing feeding, speech, the assessment of the oral cavity, dental treatment, oral hygiene and causes intense discomfort(1,2,4,33). Patients with pharynx tumors located in retromolar regions and posterior regions of the palate are most commonly affected. Still, in cases where the masticatory muscles are in the irradiation field, secondary effects such as edema, cellular destruction and muscle fibrosis will be observed(4,6). Treatment Physiotherapy exercising the involved masticatory muscles, with the utilization of dynamic bite openers to elongate such muscles is effective in increasing buccal opening(27). Non-steroid anti-inflammatory drugs and muscle relaxants (cyclobenzaprine, 10 mg, 8/8 hours for seven days) are recommended to reduce painful symptoms. Pentoxifylline is effective in cases of trismus, considering its immunomodulatory action, which regulates certain cytokines that mediate the post-irradiation fibrogenic reaction(27). DEVELOPMENTAL CHANGES The following developmental changes can be mentioned as the most common changes in pediatric patients: abnormalities in craniofacial skeletal development (mandibular micrognathia, or maxillary retrognathism), changes in odontogenesis, enamel hypoplasia, interruption in the development of dental organs, agenesias, microdontia and changes in rhizogenesis such as interruption, thinning and widening of the pulp chamber(16). CONCLUSIONS A protocol intended to minimize the sequelae of radiotherapy must be instituted and monitored before, during and after the conclusion of the treatment. The integral multidisciplinary clinical approach allows the prevention, diagnosis and management of radiotherapy side effects. The psychological aspects are relevant, and patient's self-esteem may favor the adherence to the proposed treatment, personal and dental care. REFERENCES 1. Langendijk JA. New developments in radiotherapy of head and neck cancer: higher precision with less patient discomfort? Radiother Oncol. 2007;85:1—6. 2. Salazar M, Victorino FR, Paranhos LR, et al. Efeitos e tratamento da radioterapia de cabeça e pescoço de interesse ao cirurgião dentista: revisão da literatura. Odonto (São Bernardo do Campo). 2008;16:62—8. 3. Huber MA, Terezhalmy GT. The head and neck radiation oncology patient. Quintessence Int. 2003;34:693—717. 4. Vissink A, Jansma J, Spijkervet FK, et al. Oral sequelae of head and neck radiotherapy. Crit Rev Oral Biol Med. 2003;14:199—212. 5. Rankin KV, Jones DL, Redding SW. Oral health in cancer therapy. A guide for health care professionals. 3rd ed. [Internet]. 2008. [cited 2010 Dec 14]. Available from: http://www.doep.org/images/OHCT_III_FINAL.pdf 6.Silverman S Jr. Oral cancer: complications of therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:122—6. 7. Dib LL, Gonçalves RCC, Kowalski LP, et al. Abordagem multidisciplinar das complicações orais da radioterapia. Rev Assoc Paul Cir Dent. 2000;54:391—6. 8. Geraldes AM, Jardim Júnior EG, Campos MJA, et al. Ocorrência de Porphyromonas gingivalis na microbiota bucal de pacientes submetidos à radioterapia para tratamento de lesões malignas de cabeça e pescoço. Rev Odontol Araçatuba. 2009;30(Supl 1):41. 9. Niehoff P, Springer IN, Açil Y, et al. HDR brachytherapy irradiation of the jaw — as a new experimental model of radiogenic bone damage. J Craniomaxillofac Surg. 2008;36:203—9. 10. Epstein JB, Robertson M, Emerton S, et al. Quality of life and oral function in patients treated with radiation therapy for head and neck cancer. Head Neck. 2001;23:389—98. 11. Faloni APS, Lorenzon AP, Margonar R, et al. Importância dos procedimentos periodontais prévios à radioterapia em região de cabeça e pescoço. Rev Int Periodontia Clin. 2005;2:93—9. 12. Wright WE, Haller JM, Harlow SA, et al. An oral disease prevention program for patients receiving radiation and chemotherapy. J Am Dent Assoc. 1985;110:43—7. 13. Shiboski CH, Hodgson TA, Ship JA, et al. Management of salivary hypofunction during and after radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103 Suppl:S66.e1—19. 14. Bruins HH, Jolly DE, Koole R. Preradiation dental extraction decisions in patients with head and neck cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:406—12. 15. Santos MG, Silva LCF, Lins CA, et al. Fatores de risco em radioterapia de cabeça e pescoço. RGO — Rev Gaúcha Odontol (Porto Alegre). 2010;58:191—6. 16. Albuquerque RA, Morais VLL, Sobral APV. Protocolo de atendimento odontológico a pacientes oncológicos pediátricos — revisão da literatura. Rev Odontol UNESP. 2007;36:275—80. 17. Ben-David MA, Diamante M, Radawski JD, et al. Lack of osteoradionecrosis of the mandible after intensity-modulated radiotherapy for head and neck cancer: likely contributions of both dental care and improved dose distributions. Int J Radiat Oncol Biol Phys. 2007;68:396—402. 18. Neville BW, Damm DD, Allen CM, et al. Patologia oral e maxilofacial. 2ª ed. Rio de Janeiro, RJ: Guanabara Koogan; 2004. 19. Karbach J, Callaway A, Kwon YD, et al. Comparison of five parameters as risk factors for peri-mucositis. Int J Oral Maxillofac Implants. 2009;24:491—6. 20. Raber-Durlacher JE, Elad S, Barasch A. Oral mucositis. Oral Oncol. 2010;46:452—6. 21. Bensadoun RJ, Franquin JC, Ciais G, et al. Low-energy He/Ne laser in the prevention of radiation-induced mucositis. A multicenter phase III randomized study in patients with head and neck cancer. Support Care Cancer. 1999;7:244—52. 22. Kelner N, Castro JFL. Laser de baixa intensidade no tratamento da mucosite oral induzida pela radioterapia: relato de casos clínicos. Rev Bras Cancerol. 2007;53:29—33. 23. Campos L, Simões A, Sá PHRN, et al. Improvement in quality of life of an oncological patient by laser phototherapy. Photomed Laser Surg. 2009;27:371—4. 24. Simões A, de Campos L, de Souza DN, et al. Laser phototherapy as topical prophylaxis against radiation-induced xerostomia. Photomed Laser Surg. 2010;28:357—63. 25. Lima AG, Antequera R, Peres MP, et al. Efficacy of low-level laser therapy and aluminum hydroxide in patients with chemotherapy and radiotherapy-induced oral mucositis. Braz Dent J. 2010;21:186—92. 26. Gouvêa de Lima A, Villar RC, de Castro G Jr, et al. Oral mucositis prevention by low-level laser therapy in head-and-neck cancer patients undergoing concurrent chemoradiotherapy: a phase III randomized study. Int J Radiat Oncol Biol Phys. 2010 Dec 14. [Epub ahead of print]. 27. Andrade ED. Terapêutica medicamentosa em odontologia. São Paulo, SP: Artes Médicas; 1998. 28. Antonadou D, Pepelassi M, Synodinou M, et al. Prophylactic use of amifostine to prevent radiochemotherapy-induced mucositis and xerostomia in head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2002;52:739—47. 29. Rosenthal C, Karthaus M. Current approaches in prevention and therapy of chemo- and radiotherapy-induced oral mucositis. Wien Med Wochenschr. 2001;151:53—65. 30. Noé JE. L-glutamine use in the treatment and prevention of mucositis and cachexia: a naturopathic perspective. Integr Cancer Ther. 2009;8:409—15. 31. van Bokhorst-de van der Schueren MA. Nutritional support strategies for malnourished cancer patients. Eur J Oncol Nurs. 2005;9 Suppl 2:S74—83. 32. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Consenso nacional de nutrição oncológica. [Internet]. 2009. [acessado em 6 de setembro de 2011]. Disponível em: http://www.inca. gov.br/inca/Arquivos/publicacoes/Consenso_Nutricao_internet.pdf 33. Harrison JS, Dale RA, Haveman CW, et al. Oral complications in radiation therapy. Gen Dent. 2003;51:552—60. 34. Moss RW. Should patients undergoing chemotherapy and radiotherapy be prescribed antioxidants? Integr Cancer Ther. 2006;5:63—82. 35. Lerman MA, Laudenbach J, Marty FM, et al. Management of oral infections in cancer patients. Dent Clin North Am. 2008;52:129—53. 36. Jha N, Seikaly H, McGaw T, et al. Submandibular salivary gland transfer prevents radiation-induced xerostomia. Int J Radiat Oncol Biol Phys. 2000;46:7—11. 37. Thorn JJ, Hansen HS, Specht L, et al. Osteoradionecrosis of the jaws: clinical characteristics and relation to the field of irradiation. J. Oral Maxillofac. Surg. 2000;58:1088—93. 38. Jegoux F, Malard O, Goyenvalle E, et al. Radiation effects on bone healing and reconstruction: interpretation of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:173—84. 39. Agbaje JO, Jacobs R, Michiels K, et al. Bone healing after dental extractions in irradiated patients: a pilot study on a novel technique for volume assessment of healing tooth sockets. Clin Oral Investig. 2009;13:257—61. 40. Epstein JB, Lunn R, Le N, et al. Periodontal attachment loss in patients after head and neck radiation therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.1998;86:673—7. 41. Angelov N, Pesevska S, Nakova M, et al. Periodontal treatment with a low-level diode laser: clinical findings. Gen Dent. 2009;57:510—3. 1. Surgeon Dentist, Fellow PhD degree – Organs/Systems Interactive Processes, Program of Post-graduation, Universidade Federal da Bahia (UFBA), Salvador, BA, Brazil. 2. PhD of Diagnosis of Oral Cavity, Full Professor, Department of Clinical Practice and Social Odontology – Universidade Federal da Paraíba (UFPB), João Pessoa, PB, Brazil. 3. PhD of Odontology, Associate Professor, Department of Diagnosis and Therapeutics – Universidade Federal da Bahia (UFBA), Salvador, BA, Brazil. Mailing Address: Dra. Ana Emília Holanda Rolim Rua Poetisa Cora Coralina, 229, Edifício Solar do Vale, ap. 204, Santa Teresa Salvador, BA, Brazil, 40265-070 E-mail: anaemilia.rolim@gmail.com Received May 11, 2011. Accepted after revision September 22, 2011. * Study developed at Universidade Federal da Bahia (UFBA), Salvador, BA, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554