INTRODUCTION
Acute calcific prevertebral tendinitis, or acute calcific retropharyngeal tendinitis, is a clinical syndrome originally described by Hartley in 1964. In 1994, Ring demonstrated that the syndrome is caused by calcium hydroxyapatite deposition in the longus colli muscle, a cervical flexor muscle located in the prevertebral space(1–4).
We present two cases of prevertebral tendinitis, with emphasis on imaging findings.
Case 1
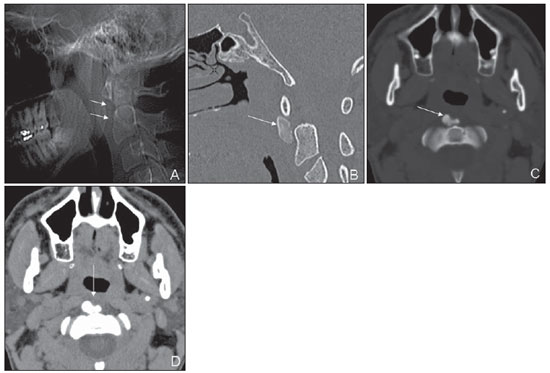
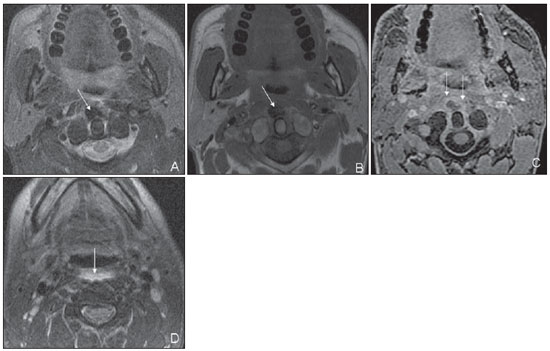
Male, 39-year-old patient complaining of occipital headache, cervical pain and limited neck movement over the past three days, without deterioration of his general condition and no fever. No previous history of surgery or pathological findings was reported. At clinical examination, normal general clinical signs, decreased neck movements amplitude, nuchal rigidity and positive Brudzinski’s sign were observed. The initial diagnostic hypothesis was meningism to be clarified, so general laboratory tests and cerebrospinal fluid analysis were requested with normal results, except for C-reactive protein whose value was 13 (reference value: 0–3.0). Cervical radiography was requested, demonstrating calcification in the prevertebral region, at C1-C2 level, and subsequently, computed tomography, which demonstrated the presence of calcification in the longus colli muscle with adjacent soft tissues swelling and fluid collections in the retropharyngeal space, suggesting acute calcific prevertebral tendonitis (Figure 1). A cervical magnetic resonance imaging scan was requested for improved evaluation of the fluid collection in the retropharyngeal space (Figure 2). As no local contrast enhancement was observed, the diagnosis was confirmed.
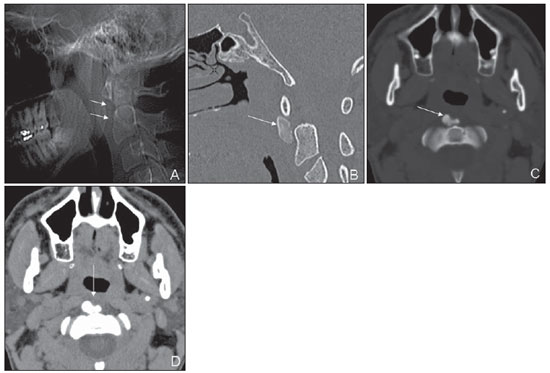
Figure 1. Digital radiography: lateral view (A) and sagittal CT reconstruction with bone window (B) and axial sections with bone window (C) of soft parts (D) in the cervical region. Note the presence of calcification in the prevertebral region, at C1-C2 level (arrows on A, B and C), adjacent soft tissues swelling (arrow on D).
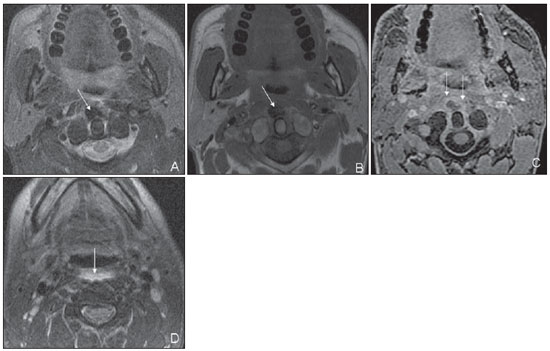
Figure 2. Axial cervical MRI T2-weighted images with fat suppression (A,D), T1-weighted image (B) and post-gadolinium T1-wieghted image (C). Prevertebral calcification is seen (arrows on A and B), with contrast enhanced adjacent soft tissues (arrows on C). Also, note the presence of fluid in the retropharyngeal space (arrow on D).
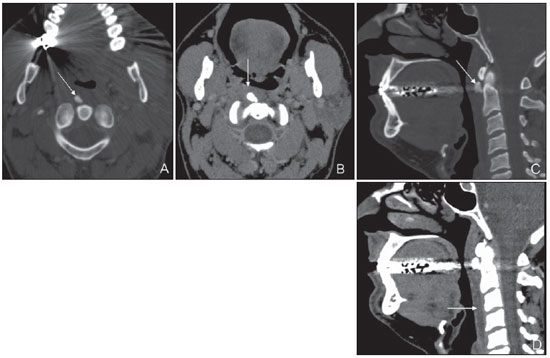
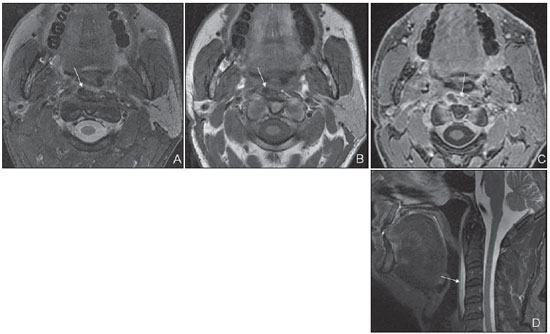
Male, 47-year-old patient presenting with neck pain with movement and odynophagia over the past four days, without deterioration of his general condition and no fever. No previous history of surgery or pathological findings was reported. At clinical examination, decreased neck movements amplitude was observed. No other particulars were observed. General laboratory tests results were normal. Cervical computed tomography was requested (Figure 3), with findings suggestive of acute prevertebral tendinitis. Later, a cervical magnetic resonance imaging scan corroborated the diagnosis (Figure 4).
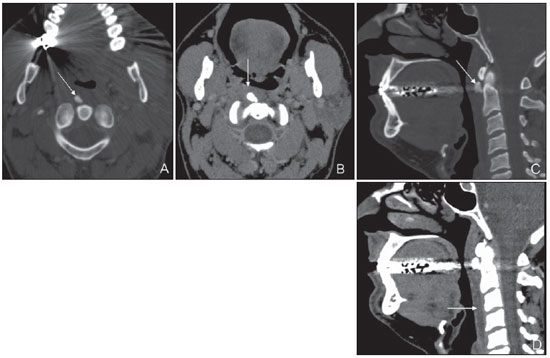
Figure 3. Axial computed tomography of the neck (A,B) sagittal reconstruction (C,D), with bone window (A,C) of soft tissues (B,D). Note the presence of prevertebral calcification at C1-C2 level in the longus colli muscle (arrow on A and C), as well as adjacent soft tissues swelling (arrow on B) and fluid in the retropharyngeal space (arrow on D).
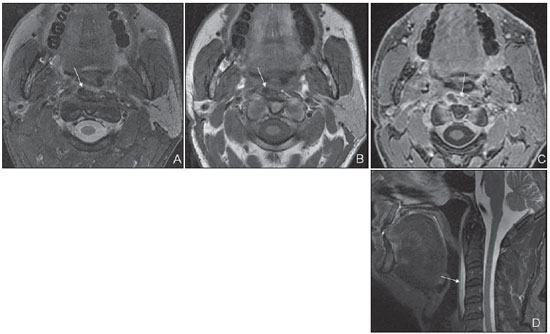
Figure 4. Axial MRI of the neck, T2-weighted images with fat saturation (A), T1-weighted (B), post-gadolinium T1-weighted (C), and sagittal T2-weighted image with fat saturation (D). Note calcification in the longus colli muscle at right (arrows on A and B), contrast enhancement of adjacent soft tissues (arrow on C) and presence of fluid in the retropharyngeal space (arrows on D).
Longus colli muscle tendinitis occurs predominantly in individuals in the age range between 30 and 60 years, and is one of the least frequent presentations of calcium hydroxyapatite crystal deposition disease(5,6).
Clinical manifestations generally include acute neck pain and/or odynophagia. At clinical examination there may be pain on palpation and decreased neck movements amplitude(3,4,7).
As regards imaging diagnosis, the findings at lateral neck radiograph are considered as being pathognomonic, consisting in presence of prevertebral calcifications at C1-C2 level with adjacent soft parts edema(2,7,8).
The prevertebral soft tissues swelling may extend from C1 to C4 and may be as much as 1.5- to 2.0-cm thick(9).
The higher contrast resolution of CT provides it with higher sensitivity as compared with plain radiography in the detection of prevertebral calcification and soft parts (tissue) edema. Additionally, it allows the identification of retropharyngeal edema, whenever it is present(8).
Magnetic resonance imaging has lower sensitivity in the identification of prevertebral calcification, which presents low signal intensity on T1- and T2-weighted images(6). Magnetic resonance imaging T2*-weighted gradient echo sequence may be utilized to increase the sensitivity in the detection of calcification, which presents with marked hyposignal.
Thanks to its higher contrast resolution, magnetic resonance imaging is more accurate in the characterization of soft tissues and retropharyngeal edema(6).
In calcific prevertebral tendinitis, fluid collections may be detected in the retropharyngeal space at imaging studies. Such a finding may be confused with retropharyngeal abscess of infectious origin. In order to differentiate such conditions, it is important to observe that, in retropharyngeal infection, a severe infectious condition is found, with peripheral contrast enhancement of the retropharyngeal space on post-contrast images, while in calcific prevertebral tendinitis there are neither clinical signs of infection, nor retropharyngeal contrast enhancement(4).
If left untreated, calcific tendinitis will spontaneously resolve in some weeks. However, early diagnosis and symptomatic treatment are very important, as the pain is debilitating in the period without treatment(5).
The treatment consists in anti-inflammatory medication for two weeks, usually with symptoms resolution within 72 hours(5).
The authors conclude that the knowledge of the imaging findings in prevertebral tendinitis is very important, since the correct diagnosis allows timely symptomatic treatment, avoiding unnecessary interventions in patients who present good response to a conservative approach.
REFERENCES
1. Hartley J. Acute cervical pain associated with retropharyngeal calcium deposit: a case report. J Bone Joint Surg Am. 1964;46:1753–4.
2. Ring D, Vaccaro AR, Scuderi G, et al. Acute calcific retropharyngeal tendinitis. Clinical presentation and pathological characterization. J Bone Joint Surg Am. 1994;76:1636–42.
3. Razon RVB, Nasir A, Wu GS, et al. Retropharyngeal calcific tendonitis: report of two cases. J Am Board Fam Med. 2009;22:84–8.
4. Eastwood JD, Hudgins PA, Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. AJNR Am J Neuroradiol. 1998;19:1789–92.
5. Hayes CW, Conway WF. Calcium hydroxyapatite deposition disease. Radiographics. 1990;10:1031–48.
6. Mihmanli I, Karaarslan E, Kanberoglu K. Inflammation of vertebral bone associated with acute calcific tendinitis of the longus colli muscle. Neuroradiology. 2001;43:1098–101.
7. Kaplan MJ, Eavey RD. Calcific tendinitis of the longus colli muscle. Ann Otol Rhinol Laryngol. 1984;93(3 Pt 1):215–9.
8. Artenian DJ, Lipman JK, Scidmore GKI, et al. Acute neck pain due to tendonitis of the longus colli: CT and MRI findings. Neuroradiology. 1989;31:166–9.
9. Haun CL. Retropharyngeal tendinitis. AJR Am J Roentgenol. 1978;130:1137–40.
1. MDs, Residents, Imaging Department – Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
2. MD, Radiologist, Imaging Department – Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
3. PhDs, MDs, Radiologists, Imaging Department Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
4. PhD, MD, Radiologist, Coordinator for the Imaging Department – Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
Mailing Address:
Dr. Caio Giometti Grassi
Hospital Israelita Albert Einstein – Departamento de Imagem, Sala de Laudos
Avenida Albert Einstein, 627, 4º andar, Bloco D, Morumbi
São Paulo, SP, Brazil, 05652-901
E-mail: caiograssi@hotmail.com
Received September 10, 2010.
Accepted after revision June 20, 2011
Study developed at Imaging Department – Hospital Israelita Albert Einstein, São Paulo, SP, Brazil.
 Vol. 44 nº 5 - Sep. / Oct. of 2011
Vol. 44 nº 5 - Sep. / Oct. of 2011