Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011
|
ORIGINAL ARTICLES
|
|
Digitalization of X-ray films with image stitching |
|
|
Autho(rs): Jaime Grande Vela1; Amit Bhaya2; Alexandra Maria Vieira Monteiro3; Leonardo Valente Ferreira4; Alair Augusto Sarmet Moreira Damas dos Santos5; Maria Lucia Santos5; Paulo Bahia6; Elise Tonomura7 |
|
|
Keywords: Digital radiology; Teleradiology; Image stitching. |
|
|
Abstract: INTRODUCTION
The original concept of digital radiology was introduced in the late 1970’s and early 1980’s, but this technology was not totally mature until the 1st International Conference and Workshop on Picture Archiving and Communication Systems (PACS), held in Newport Beach, California, in January 1982(1). With the introduction of digital imaging, a new era was launched in the field of radiology: the utilization of digital files in lieu of conventional films has brought new conveniences for manipulation, transmission, storage and viewing of radiographs. The digital representation of radiographs provides a number of advantages for the Brazilian health system, such as the proven efficiency of the second opinion systems over the internet(2) and even the utilization of such digital material in teaching and training processes(3). In order to make full use of the advantages of the digital representation of a radiograph, in addition to digital radiography (DR) itself, whose implementation cost is considerably higher than conventional radiography’s, one may resort to digitization of conventional radiographic films(4). There are currently two methods for the digitization of radiographic films: one of them is the utilization of digital photography, and the other is by means of the utilization of a transparency scanner(5,6). The Brazilian reality as country of continent wide extent and limited resources makes it practically impossible to replace all existing conventional radiography equipments by DR equipments or even the large scale acquisition of computed radiography (CR) equipments. On the other hand, the small number of radiologists available in geographically remote areas besides the prevalence of pulmonary disorders, makes the low cost digitization solutions for general radiology become essential as a means for teleradiology between remote locations and excellence centers, thus reducing geographic barriers, patient travels and costs for the national health system. Digitization by means of digital cameras has been utilized, but with limitations regarding technical requirements for image acquisition, such as: a) need for a dark room for images capture; b) utilization of a negatoscope; c) previous adjustments of the camera’s parameters; d) utilization of a tripod to prevent movements of the camera during image acquisition; e) post-edition (cutting, rotation, grayscale, etc.) of captured images(4). For this very reason, the objective of the present study has been to develop a reproducible, user friendly and low cost process to digitize radiographic films, most specifically chest radiographs on account of their high demand, by utilizing a transparency scanner associated with an image stitching software specially developed by the present project team, by means of which parts of an image are automatically combined. The present investigation was developed with the financial support of Financiadora de Estudos e Projetos (FINEP) (the Brazilian Agency for Research and Project Financing), at Núcleo de Atendimento em Computação de Alto Desempenho (NACAD/COPPE) (Center for Assistance in High Performance Computation). MATERIALS AND METHODS The operation of a common or desktop scanner is based on the capture, by a sensor, of the light reflected over a media placed on the scanner’s tray. Such a process is continuously performed and the final result is a digital representation of the scanned image(7). This process is practically the same in all scanner models, but in transparency scanners, the light source is placed behind the image and not before, as in the case of common scanners. For that reason, for radiographic films, a transparency scanner is utilized. The most common transparency scanners available in the market are geared for the A4 (21 × 29.7 cm) format, but such type of scanner is not capable of digitizing most radiographic films utilized in the clinical radiology practice, on account of their limited area of imaging. On the A3 format (29.7 × 42 cm) scanners, it is possible to almost completely digitize all the evaluated films, but the high cost of such equipment (up to six times the cost of an A4 scanner) makes its utilization prohibitive in terms of cost(8). Thus, in order to achieve the cost objectives, the authors opted for the use of an A-4 transparency scanner (ScanMaker i800; Microtek, Hsinchu, Taiwan), whose market price is approximately R$ 2,000.00 (US$ 1,266.00), overcoming the spatial limitation of the imaging area by means of the utilization of an image stitching software known as scanRX, specially developed by the team involved in the present project, by means of which parts of an image are automatically combined to form a complete image with no sign of the stitching(9,10). The generation of a complete image from parts of this same image is a common problem occurring with image processing techniques, and several solutions to this problem have already been proposed(9—11). In this process, each digitized image will be treated as a matrix or two-dimensional table, where each element or pixel has a specific coordinate or specific position in the ij plane with a value representing its luminous intensity, which may range from 0 (completely black) to 255 (completely white). Thus, each digital image is defined as a m × n matrix (m columns and n lines) composed by elements with their position defined by i,j coordinates within the matrix, and a luminous intensity value which is a natural number between 0 and 255. For the stitching process, the definition of an overlap area (superimposition) is indispensable, i.e., a common region between two images that comprise part of a larger image(11). In the specific case of image stitching under analysis in the present article, a same film is positioned on the scanner in such a way to generate partial images, i.e., with common or repeated parts. The task performed by the stitching algorithm is exactly the utilization of the data associated with the physical scanning process to calculate a reference point that allows the combination of two images that belong to larger image, superimposing the equal parts(12). Figure 1 shows an example of an overlap area between two images. 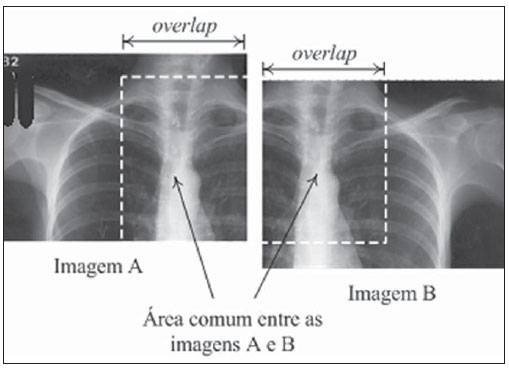 Figure 1. Images overlapping areas. Once the overlap areas are identified on the images obtained from a same film, the next step in the image stitching process is the selection of a sub-image, within the overlap area of image A, called “matching area”(12,13), that will serve the purpose of locating the correct position for the images stitching or fusion. One observes that such a matching area is contained in both sub-image A (hereinafter CA) and sub-image B (hereinafter CB). Therefore, the positioning of CA exactly over CB implies the accurate fusion or stitching of the two sub-images A and B. Figure 2 depicts a representation of what a matching area located within the overlap area of image A would be. 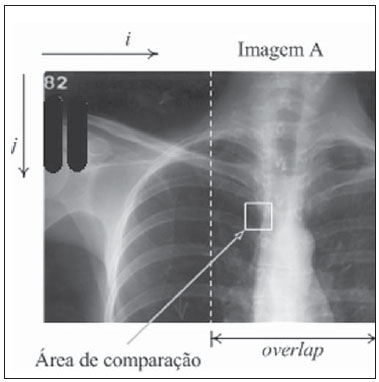 Figure 2. Images matching area. The number of elements or pixels of this sub-image, called “matching area”, is a key factor in the algorithm’s processing time, as the greater the number of pixels is in the matching area, the greater will be the computational effort (processing time)(13). On the other hand, the greater the number of pixels in the matching area, the greater will be the chances of finding this same area contained in the other sub-image, and consequently, of a successful image stitching. Considering that radiographs of lung fields commonly present large areas with the same gray levels, it is necessary to perform a careful selection of the matching area based on the greater dispersion of gray levels contained in such an area, so that there is enough relevant data to facilitate a successful images stitching(14). In order to accelerate the above briefly described stitching process, a “reduced search area” is defined, based on the assumption that the images acquisition is ideally performed, i.e., the partial images are completely aligned, without any vertical displacement among them. Such an ideal image acquisition is in fact feasible, by utilizing the data on the films and imaging area sizes, and the number of pixels per resolution inch in the scanner, besides the physical characteristics of the scanner itself, as detailed by Vela(13). With accurate data on overlap area and dimensions of the partial images (in pixels), it is possible to calculate the accurate matching area coordinates. Figure 3 shows a reduced search area on image B. 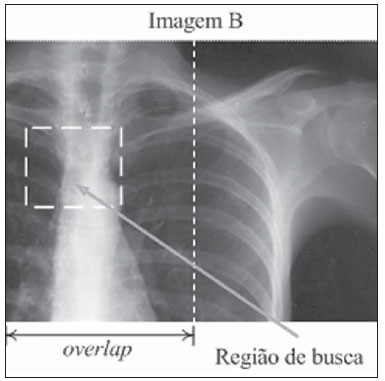 Figure 3. Search region on the image. Once the optimum matching area and the reduced search area are defined, the images matching process is initiated. Such a process consists in calculating the degree of similarity between the matching area on sub-image A and all the areas of the same size and format on sub-image B, exhaustively going through the reduced search area on B. In order to quantify the degree of similarity utilized in the images matching, the authors have opted to calculate the root of the grayscale average difference (RGAD)(12,13), which is defined as the average of the sum of the difference between two corresponding pixels on the images being matched. In a simpler way, the lower the RGAD value, more similar are the images in terms of differences of the values of pixels with equal coordinates. Figure 4 depicts an example of two elements (pixels) with the same coordinates on corresponding images. 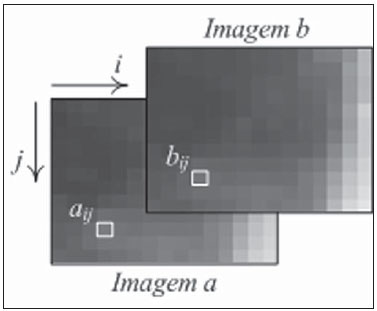 Figure 4. Pixels with the equal coordinates on two corresponding images. The algorithm performs a line by line, and column by column scan: for each point of the matrix of the reduced search area, RGAD is calculated and stored for later determination of the coordinates that correspond to the lowest RGAD. Such a process is represented on Figure 5. 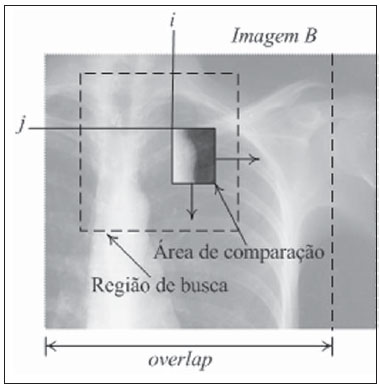 Figure 5. Search region scanning. The coordinates (i,j) of the point corresponding to the highest degree of similarity are utilized to overlap the images containing the matching area (A) over the image that contains the search region (B). Such a process results in a single image that is larger the two previous images, and is comprised by partial images A and B. The stitching process does not consist only of the mere superimposition of the sub-images, but also takes care of the fusion of the pixels values in the overlap region(9,13), in such a manner that the human eye is unable to distinguish any traces of the stitching process (such as a stitching line, for example). The result is depicted on Figure 6. 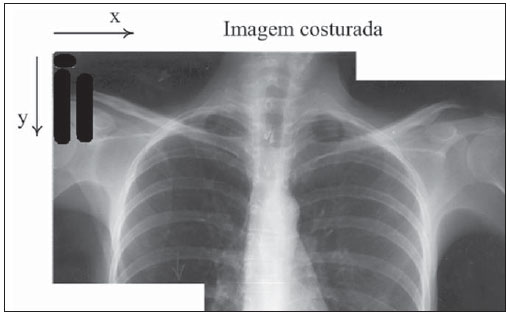 Figure 6. Two images stitching. For radiographic films of adult patients, for whom chest radiography (PA) would normally be made on a 35 cm × 43 cm film, the whole process of film digitization comprises four scanning routines for parts of the film, as well as three stitching and formatting routines, automatically performed by the scanRX software. RESULTS All the performance tests developed with the above described digitization process were carried out on an ordinary microcomputer equipped with an AMD 3800, 2.4 GHz microprocessor and 1 GB RAM. The total time spent in the digitization process was considered as being the sum of the time of scanning of parts of the film and the time required by the scanRX software to perform the image stitching process. For 35 cm × 43 cm radiographic films, the mean time for the (automatic) routine performed by the scanRX software was 8.15 seconds, and the mean acquisition time for the four sub-images corresponded to approximately four minutes (one minute per sub-image). It is important to highlight that the scanning is an electro-mechanical process performed by the A4 scanner, with no possibility of external control, and the time required by the software includes the routines of recognition, images stitching and later output file formatting, which is available in the standard format (DICOM) for medical images. The images acquired with this process (example on Figure 7) were analyzed by radiologists with more than 15 years of experience, at Hospital Universitário Pedro Ernesto of Universidade do Estado do Rio de Janeiro, at Hospital Universitário Antônio Pedro of Universidade Federal Fluminense, and at Hospital Universitário Clementino Fraga Filho of Universidade Federal do Rio de Janeiro. Approximately 280 radiographs were digitized and classified according to: a) image quality; b) certainty in the identification of the lesion (s), with sensitivity and specificity of 94% and 95%, respectively. 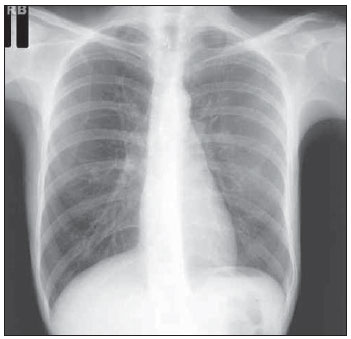 Figure 7. Result from digitization of a 35 cm x 35 cm film. DISCUSSION Previous studies demonstrated the possibility of utilization, in radiology, of images obtained by means of digital cameras(5,6,15). Such studies have reported the absence of significant differences between the original film and its compressed digital image (JPEG format), for the diagnosis of lung lesions caused by pulmonary tuberculosis. Later studies have reported better results in the digitization of films with desktop scanners equipped with transparency adapter(16,17), and in such studies the utilization of scanners demonstrated improvements of 5% to 13% in the diagnostic accuracy as when compared with the utilization of images acquired with digital cameras. The total digitization time utilizing image stitching is mostly taken by the sub-image capture process; such a process is performed by the user with the assistance of the graphic interface of the scanRX software; and, considering that user friendly graphic interface displays the whole procedure in detail, interactively and on a step-by-step basis, no basic IT knowledge is required to operate the system. The time required by the stitching and edition processes which are automatically performed by the software, is much shorter (3.3%) than the time spent by the operator in the acquisition of scanned sub-images. Thus, it is possible to affirm that the swiftness of the procedure is determined by the scanner speed and not by the time required by the software in the images processing. Currently such method is being implemented as a pilot trial in eight low cost teleradiology units in the State of Rio de Janeiro, in a partnership with the Programa Nacional de Telessaúde (Nationwide Telehealth program)(18). CONCLUSION The method for films digitization utilizing image stitching has achieved the proposed objectives of easy utilization, results reproducibility and high quality of final images. The low cost objective remained compromised, as the cost of the necessary equipment (A4 transparency scanner) is higher than the cost of a digital photographic camera. However, the appropriate result of the digital photography method depends on certain conditions and resources. The utilization of a scanner and specific software provides this method with independence from ambient lighting, from a negatoscope and from operators’ IT knowledge, besides the advantage of providing final images in an appropriate format for medical images (DICOM). Acknowledgments To FINEP — Financiadora de Estudos e Projetos, for the financial support. REFERENCES 1. Huang HK. PACS and imaging informatics: basic principles and applications. 2nd ed. Hoboken, NJ: Wiley-Liss; 2004. 2. Neira RAQ, Puchnick A, Cohrs FM, et al. Avaliação de um sistema de segunda opinião em radiologia. Radiol Bras. 2010;43:179-83. 3. Elias S, Pires SR, Patrocinio AC, et al. Uso de software como ferramenta pedagógica no processo de ensino-aprendizagem da mamografia digital. Radiol Bras. 2009;42:115-20. 4. Samei E. Acquisition of digital chest images for pneumoconiosis classification: methods, procedures, and hardware. Proc. NIOSH/ILO Scientific Workshop on Pneumoconiosis, Washington, DC, March 2008. 5. Logeswaran R, Choong MK, Bister M. Diagnostic quality of X-ray films digitised using conventional digital cameras. The Imaging Science Journal. 2009;57:1-7. 6. Szot A, Jacobson FL, Munn S, et al. Diagnostic accuracy of chest X-rays acquired using a digital camera for low-cost teleradiology. Int J Med Inform. 2004;73:65-73. 7. Tyson J. How scanners work. [cited 2010 Dec 28]. Available from: http://computer.howstuffworks.com/scanner.htm 8. Fast Scan Service. Filmes / fotos / transparências. [cited 2010 Dec 28]. Available from: http://www.fastscan.com.br/cms/cmsms/index.php/portugues/equipamentos/filmes-fotos-transparencias 9. Zomet A, Levin A, Peleg S, et al. Seamless image stitching by minimizing false edges. IEEE Trans Image Process. 2006;15:969-77. 10. Li Y, Ma L. A fast and robust image stitching algorithm. Proc 6th World Congress on Intelligent Control and Automation; 2006 June 21-23; Dalian, China. 11. Gramer M, Bohlken W, Lundt B, et al. An algorithm for automatic stitching of CR X-ray images. Advances in Medical Engineering. 2007;114(PtII):193-8. 12. Wang X, Zhao Z. High-precision image mosaic method in big frame measurement. Proc 1st International Symposium on Systems and Control in Aerospace and Astronautics; 2006 Jan 19-21; Harbin, China. 13. Vela JG. Digitalização de filmes radiográficos utilizando costura de imagens [dissertação]. Rio de Janeiro, RJ: Universidade Federal do Rio de Janeiro; 2010. 14. Gonzalez RC, Woods RE. Digital image processing. 3rd ed. New Jersey: Prentice Hall; 2008. 15. Sistrom CL, Gay SB. Digital cameras for reproducing radiologic images: evaluation of three cameras. AJR Am J Roentgenol. 1998;170:279-84. 16. Bassignani MJ, Bubash-Faust L, Ciambotti J, et al. Conversion of teaching file cases from film to digital format: a comparison between use of a diagnostic-quality digitizer and use of a flatbed scanner with transparency adapter. Acad Radiol. 2003;10:536-42. 17. Ruess L, Uyehara CFT, Shiels KC, et al. Digitizing pediatric chest radiographs: comparison of low-cost, commercial off-the-shelf technologies. Pediatr Radiol. 2001;31:841-7. 18. Núcleo de Telessaúde do Estado do Rio de Janeiro. Programa Telessaude Brasil. [cited 2010 Oct 23]. Available from: http://www.telessauderj.uerj.br/ 1. Master, Level II Scholar of Industrial Technology Development, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), NACAD/COPPE-UFRJ, Rio de Janeiro, RJ, Brazil. 2. PhD, Professor, COPPE-UFRJ, Rio de Janeiro, RJ, Brazil. 3. PhD, Associate Professor of Radiology, Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brazil. 4. PhD, Researcher, NACAD/COPPE-UFRJ, Rio de Janeiro, RJ, Brazil. 5. PhDs, Associate Professors of Radiology, Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil. 6. PhD, Associate Professor of Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. 7. Master, Assistant Professor of Radiology, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. Mailing Address: Eng. Jaime Grande Vela Cidade Universitária – Centro de Tecnologia Bloco I, Sala I-248, Ilha do Fundão Rio de Janeiro, RJ, Brazil, 21941-972. Caixa Postal 68516 E-mail: jaimegvela@yahoo.com.br Received Jan 13, 2011. Accepted after revision May 30, 2011. Study developed at Núcleo de Atendimento em Computação de Alto Desempenho (NACAD) (Center for Assistance in High Performance Computing) of COPPE-UFRJ, Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554