Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011
|
ORIGINAL ARTICLE
|
|
Sensitivity of upper gastrointestinal series in the diagnosis of gastroesophageal reflux in premature infants |
|
|
Autho(rs): Beatriz Regina Alvares1; Osmar Henrique Della Torre2; Maria Aparecida Mezzacappa3 |
|
|
Keywords: Gastroesophageal reflux disease; Upper gastrointestinal series; 24-h esophageal pH monitoring; Preterm newborns. |
|
|
Abstract: INTRODUCTION
Gastroesophageal reflux disease (GERD) is defined as a disorder of the distal esophagus, with frequent return of the gastric contents into the esophagus, associated with digestive and extra-digestive symptoms such as frequent regurgitation and vomiting episodes in association with low weight gain, anemia, esophagitis or respiratory complications(1,2). Over the past two decades more studies about this disease in the neonatal period have been undertaken; however many aspects still remain to be clarified(3). At the neonatal period, the investigation for GERD is of significant relevance, as such this entity can cause severe symptoms in neonates, particularly in preterm newborns, such as episodes of apnea, bradycardia, cyanosis and vomiting. Gastroesophageal reflux disease has also been associated with apparently life-threatening complications such as aspiration pneumonias and apnea, significantly extending the hospital stay of such neonates(2,4-13). Although the long-term esophageal pH monitoring is still considered as the gold standard for the diagnosis of GERD, it presents the disadvantages of an invasive and expensive procedure, besides demanding specialized personnel and equipment, and for these very reasons the method is not being used in many services(14,15). On the other hand, upper gastrointestinal (UGI) series is a low-cost, less invasive well tolerated and it is available at most medical/clinical assistance centers. Additionally, UGI series can detect anatomical abnormalities associated with the present symptoms in the upper gastrointestinal tract, and is the conventional imaging method for the study of GERD(14,15). The early diagnosis of GERD and associated complications in preterm newborns is of utmost importance as it allows better approaches for the treatment of such an entity, potentially shortening hospital stay length and reducing morbidity. The purpose of this study was to evaluate the sensitivity of UGI series for the diagnosis of GERD in preterm newborns, with clinical manifestations and esophageal pH monitoring highly suggestive of the disease, as well as describing the presence of congenital upper gastrointestinal tract malformations detectable at the radiological exam. MATERIALS AND METHODS The research project was approved by the Committee for Ethics in Research on humans of the institution and the neonates were included in the study after a term of free and informed consent was signed by family members. A prospective descriptive study was developed with 41 preterm neonates admitted to a tertiary neonatal care unit, with symptoms suggestive of GERD. Amongst the neonates, 22 (53.7%) were boys and 19 (46,3%) were girls, with gestational age < 37 weeks, all of them weighting < 2,500 g at birth, with weight ranging between 655 g and 2,450 g. The symptoms of GERD presented by the neonates considered as indications for long-term distal esophageal pH monitoring were: xanthine resistant apnea and/or bradycardia, frequent vomiting and/or regurgitation associated with poor weight gain (< 20-30 g/day), apparent life-threatening apnea, multiple atelectasis or pneumonias, need for long-term oxygen therapy and unexplained worsening of respiratory conditions. Prolonged (18 to 24-hours) distal esophageal pH monitoring was performed by one of the investigators, at the discretion of the unit’s medical team, and only neonates whose pH monitoring results were abnormal (reflux index > 10%) were chosen to participate in the study(16). The equipment utilized for documenting and recording of the exam was a Digitrapper MkIII (Medtronic Inc.; Shoreview, MN, USA), using antimony electrodes (Medtronic Inc., Shoreview, MN, USA) positioned at the distal third of the esophagus, at the level of the T6-T7 vertebral bodies. In all of the exams, the electrode position was confirmed by means of chest X-ray. The software utilized for results analysis was the EsopHogram version 5.60C4 (Gastrosoft Inc.; Irving, TX, USA). During the exams, the neonates remained on horizontal dorsal decubitus, receiving dietary intake of 120-130 ml/kg/day every four hours by means of a gastric feeding tube. The neonates were kept without medications such as antacids, H2 blockers, xanthines or corticosteroids that could affect the exam’s results for at least 48-72 hours before the examination. The UGI series was performed as soon as the infants’ clinical conditions were considered sufficiently stable, with low frequency of apnea or oxygen desaturation and with appropriate body temperature control in open cribs, thus involving low risk for transportation of the neonate to the radiology center. The neonates that could not be transported for radiological investigation for being under assisted ventilation and preterm neonates with disorders which contraindicated enteral feeding were excluded from the study. The radiological investigation included plain chest X-ray and abdominal films and UGI series. The investigation of reflux episodes under fluoroscopic control was performed after oral ingestion of barium diluted in glucose solution or milk, administered by a bottle or by a gastric tube. The maximum amount of contrast medium was equivalent to that which the neonate would swallow in a breastfeeding, with upper digestive tract morphology and motility being studied. The quantitative evaluation of reflux by contrast-enhanced radiological study was performed with the neonate positioned on dorsal decubitus, and results were considered as abnormal in cases where more than three reflux episodes were observed in patients up to six weeks of life and more than two reflux episodes in patients above seven weeks of life(17). For the qualitative evaluation of reflux, it was considered the height reached by the refluxate in the oesophagus. The degree of the reflux was then graded as small if below the lower third of the oesophagus, moderate if in the middle third and significant if above the middle third of the oesophagus. The quantitative assessment of reflux episodes by means of intermittent fluoroscopy occurred over a maximum period of 5 minutes. The radioscopy flashes did not exceed 20 seconds(17). The following descriptive variables were studied: gestational age in weeks; birth weight in grams; postnatal age in days at the moment of pH monitoring and at the day the UGI series was performed; and the results of the quantitative evaluation of reflux by pH monitoring, namely: total number of reflux episodes, duration of the longest episode, number of episodes lasting longer than five minutes, and percentage of total examination time with esophageal pH < 4, also called reflux index (RI). Abnormal results corresponded to RI > 10%, at the research period(16). The study sample size was based on the prevalence of symptoms (vomiting, apnea, decreased oxygen saturation, bradycardia, bronchospasm, oxygen dependence) identified in 18 neonates, establishing a sampling error of 15%. It was established that 41 cases would be necessary, considering that such a figure reflected the appropriate sample size for the set of symptoms. Descriptive analyses of the sample variables were performed by calculating mean and standard deviation, minimum and maximum values, establishing sensitivity value and confidence interval of 95% (CI 95%) for the UGI series. The Student’s t-test was utilized at the comparison between the radiological severity and RI. The Wilcoxon test was utilized at the comparison between days of life in which both examinations were performed. The Statistical Analysis System (SAS) version 8.2 was utilized for statistical data analysis. RESULTS Among the symptoms observed during the neonates’ hospital stay, decreased oxygen saturation was the most prevalent one, being found in 33 cases (80.5%). Other symptoms (more than one symptom/sign per neonate) were apnea, in 22 cases (53.7%), vomiting episodes in 17 cases (41.5%), cyanosis in 15 cases (36.6%), bradycardia in 11 cases (26.8%) and lastly, bronchospasm, present in three cases (7.3%). The mean RI was 24.4% ± 12.1%, ranging between 11.3% and 60.9%. The description of the pH monitoring parameters is shown on Table 1. 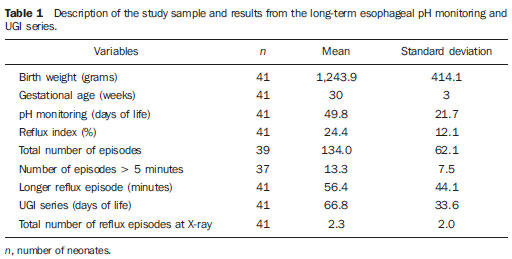 On average, the radiological examination was performed at 66.8 days of life, versus 49.7 days at the pH monitoring, being this difference, between the two values, statistically significant (p = 0.007). Therefore, the mean interval between examinations was 17.1 days. The sensitivity of the UGI series was 56.1% with CI 95% between 39.9% and 71.2% (Table 2). As regards the qualitative evaluation of pathological reflux episodes, 41.5% (12 cases) presented significant reflux, while 44.8% (13 cases) presented moderate reflux and 13.8% (4 cases) presented with mild reflux. 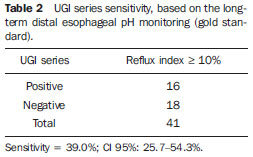 Among all performed radiological examinations, 18 cases were considered as physiological reflux, with a mean of 1.33 ± 0.55 episodes, being the minimum of 1 and maximum of 2 episodes. On the other hand, results of 23 radiological studies were considered as abnormal, with 3.78 ± 1.44 episodes, ranging between 2 and 7. Table 3 presents the description of the mean RI values according to the qualitative radiological assessment of pathological reflux episodes. No significant difference was observed in RI according to the UGI series severity levels. 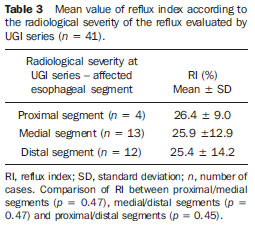 In the present sample, UGI series found sliding hiatus hernia in one neonate at 65 days of life. In this case, six significant reflux episodes were demonstrated, besides gastric emptying time greater than five minutes (Figure 1). At 56 days of life, pH monitoring demonstrated RI = 35.8%, with 24 episodes, all of them longer than 5 minutes, with the longest episode lasting 144 minutes.  Figure 1. UGI image of a 65-day old neonate, demonstrating significant gastroesophageal reflux, in association with sliding hiatus hernia. DISCUSSION Upper gastrointestinal series presented low sensitivity in the diagnosis of GERD in a sample of preterm neonates, considering the esophageal pH monitoring as the gold standard; however it identified anatomic abnormality of the upper digestive tract in one neonate. Several authors(15,18-21) have demonstrated higher sensitivity and specificity of pH monitoring in the diagnosis of GERD as compared with other complementary studies currently available. However few studies exclusively evaluating newborns are found in the literature. Studies conducted in infants below one year of age, with samples between 21 and 61 neonates, demonstrated radiography sensitivity ranging between 29% and 40%(15,21). The lower sensitivity of the radiological study, as compared with esophageal pH monitoring can be explained, among other factors, by the short fluoroscopy time (5 intermittent minutes) and by the higher density of the barium contrast medium, as compared with a normal gastric contents(15). In the present study, sensitivity of 39.0% (CI 95% of 25.7–54.3%) was found, similar to that reported in the literature. However, considering that the present study evaluated exclusively preterm neonates, the authors could not establish an accurate sensitivity comparison. Few studies were found in the literature describing contrast-enhanced radiological examination of the esophagus, stomach and duodenum exclusively in preterm neonates admitted to a neonatal unit. The study developed by Ozelame et al.(22), which included 12 neonates in their series, has emphasized the relevance of the standardization of the radiological technique and of the radiologist’s experience for the method sensitivity. In the present study, a relevant factor to be taken into consideration was the significant difference at the moment of the two examinations performance (mean of 17 days). No data was found in the literature on the acceptable time interval, considering the necessity of stable clinical conditions of the neonate, such as weight > 2,000 g and thermal stability, for the performance of the radiological exam. Such conditions are not required for the esophageal pH monitoring, so it characterizes an advantage of this method. The two-week time difference might, in some neonates, be sufficient to promote maturation of the function of the lower esophageal sphincter and the whole digestive tube. and, as a consequence, it may cause a significant reduction in reflux episodes. By itself, such factor may be accountable for the loss of sensitivity of the radiological method in this sample. A superficial analysis demonstrates that esophageal pH monitoring presents as disadvantages the invasive characteristic of this method and the expensiveness, besides requiring an appropriately trained physician, factors which impair its utilization in many hospitals(15). On the other hand, UGI series is a low-cost method that is well tolerated and is able to detect anatomical abnormalities and complications such as hiatus hernia, intestinal obstruction and intestinal malrotation, as well as motility disorders(9,19,21), being available at most hospital medical centers (15). Studies highlight the indication of UGI series for children with symptoms of GERD to identify anatomic abnormalities in the esophagus, stomach and duodenum, but not all of them report the percentage of malformations found(7,9,15,19,20). Al-Khawari et al.(15), in a retrospective study with 169 patients comparing UGI series and esophageal pH monitoring, have found a predominance of anatomic abnormalities in the age group < 1 year, including 9 patients with intestinal malrotation, 9 with hiatus hernia, and 15 with other changes in the gastroduodenal junction. In the present study sample, only one case of hiatus hernia was found, with no other anatomic abnormally being found in the upper digestive tract, a fact that may be explained by the small sample size (41 individuals) and by the fact that only neonates were studied, an age group which was not specified in the study developed by Al-Khawari et al.(15). No data was found in the literature establishing association between RI, evaluated by esophageal pH monitoring, and the number of reflux episodes in the UGI series. Such an association was not observed in the present study, and may be an interesting aspect to be analyzed in further studies. Recently, by means of a new method for GERD evaluation - multiple intraluminal esophageal impedance - a significant association could be observed between reflux episodes extent and the acid clearance time with the presence of symptoms/signs of GERD in preterm newborns(23). In this study, the occurrence and frequency of the symptoms depended on the most proximal extent of the reflux and the esophageal clearance time(23). Thus, the authors conclude that UGI series demonstrated low sensitivity for GERD in preterm newborns, and it did not associate with the reflux severity as compared with the esophageal pH monitoring. However, it is useful in the detection of anatomical abnormalities in the upper gastrointestinal tract. REFERENCES 1. Herbst JJ. Gastroesophageal reflux. J Pediatr. 1981;98:859-70. 2. Herbst JJ, Meyers WF. Gastroesophageal reflux in children. Adv Pediatr. 1981;28:159-86. 3. Molloy EJ, Di Fiore JM, Martin RJ. Does gastroesophageal reflux cause apnea in preterm infants? Biol Neonate. 2005;87:254-61. 4. Orenstein SR. Controversies in pediatric gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 1992;14:338-48. 5. Corvaglia L, Zama D, Gualdi S, et al. Gastro-oesophageal reflux increases the number of apnoeas in very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2009;94:188-92. 6. Farhath S, Aghai ZH, Nakhla T, et al. Pepsin, a reliable marker of gastric aspiration, is frequently detected in tracheal aspirates from premature ventilated neonates: relationship with feeding and methylxanthine therapy. J Pediatr Gastroenterol Nutr. 2006;43:336-41. 7. Carmona-Sánchez R, Santos-Díaz MA, Rentería-Cárdenas A. Enfermedad por reflujo gastroesofágico. Bol Med Hosp Infant Mex. 1992;49:259-66. 8. Milla PJ. Reflux vomiting. Arch Dis Child. 1990;65:996-9. 9. Jung AD. Gastroesophageal reflux in infants and children. Am Fam Physician. 2001;64:1853-60. 10. Hebra A, Hoffman MA. Gastroesophageal reflux in children. Pediatr Clin North Am. 1993;40:1233-51. 11. Gomes H, Lallemand PH. Infant apnea and gastroesophageal reflux. Pediatr Radiol. 1992;22:8-11. 12. Naik DR, Moore DJ. Ultrasound diagnosis of gastro-oesophageal reflux. Arch Dis Child. 1984;59:366-7. 13. Frakaloss G, Burke G, Sanders MR. Impact of gastroesophageal reflux on growth and hospital stay in premature infants. J Pediatr Gastroenterol Nutr. 1998;26:146-50. 14. Jadcherla SR. Gastroesophageal reflux in the neonate. Clin Perinatol. 2002;29:135-58. 15. Al-Khawari HA, Sinan TS, Seymour H. Diagnosis of gastro-oesophageal reflux in children. Comparison between oesophageal pH and barium examinations. Pediatr Radiol. 2002;32:765-70. 16. Vandenplas Y, Goyvaerts H, Helven R, et al. Gastroesophageal reflux, as measured by 24-hour pH monitoring, in 509 healthy infants screened for risk of sudden infant death syndrome. Pediatrics. 1991;88:834-40. 17. Andrade MR. Refluxo gastro-esofagiano na infância: padronização da metodologia e interpretação do estudo radiológico. Rev Paul Pediatr. 1988;6:33-4. 18. Gomes H, Menanteau B. Gastro-esophageal reflux: comparative study between sonography and pH monitoring. Pediatr Radiol. 1991;21:168-74. 19. Norton RC, Penna FJ. Refluxo gastroesofágico. J Pediatr. 2000;76:S218-24. 20. Da Dalt L, Mazzoleni S, Montini G, et al. Diagnostic accuracy of pH monitoring in gastro-oesophageal reflux. Arch Dis Child. 1989;64:1421-6. 21. Aksglaede K, Pedersen JB, Lange A, et al. Gastro-esophageal reflux demonstrated by radiography in infants less than 1 year of age. Comparison with pH monitoring. Acta Radiol. 2003;44:136-8. 22. Ozelame VJ, Schoeller C, Capella MR. Refluxo gastroesofágico na criança. J Pediatr. 1988;64:19-28. 23. Jadcherla SR, Gupta A, Fernandez S, et al. Spatiotemporal characteristics of acid refluxate and relationship to symptoms in premature and term infants with chronic lung disease. Am J Gastroenterol. 2008;103:720-8. 1. PhD of Radiology, Professor, Department of Radiology at Faculdade de Medicina da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. 2. MD, Resident at Hospital das Clínicas da Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil. 3. PhD of Pediatrics, Professor, Faculdade de Medicina da Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. Mailing Address: Dra. Beatriz Regina Alvares Rua Alberto de Salvo, 238, Barão Geraldo Campinas, SP, Brazil, 13084-759 E-mail: alvaresb@terra.com.br Received May 3, 2011. Accepted after revision June 22, 2011. Study developed at Hospital da Mulher Prof. Dr. José Aristodemo Pinotti – Centro de Atenção Integral à Saúde da Mulher (CAISM), Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554