Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011
|
ORIGINAL ARTICLE
|
|
Contribution of PSA density in the prediction of prostate cancer in patients with PSA values between 2.6 and 10.0 ng/ml |
|
|
Autho(rs): Hugo Alexandre Sócrates de Castro1; Wagner Iared2; David Carlos Shigueoka3; José Eduardo Mourão4; Sérgio Ajzen5 |
|
|
Keywords: Prostate; Prostate biopsy; Prostate cancer; PSA density. |
|
|
Abstract: INTRODUCTION
According to the World Health Organization, prostate cancer is the second most common cancer in men, being the sixth most frequent cause of deaths among the male population worldwide. The Instituto Nacional de Câncer (INCA) (National Cancer Institute) forecasts 52,350 new cases in Brazil in 2010(1). Prostate cancer affects mostly patients above 50 years of age and preferably occurs in the prostate peripheral zone. Mortality rate is relatively low, particularly in early diagnosed cases(2). Digital rectal examination and serum prostate-specific antigen (PSA) test are the most utilized methods of prostate cancer screening. The digital rectal examination presents limitations in case of nonpalpable prostatic lesion (early stages), and whenever a change is detected, the differentiation between malignant and benign lesions is difficult. Serum PSA testing, in clinical use since 1986, is the most frequently utilized tumor marker for the screening of prostate cancer. It plays an important role in the early diagnosis of such cancer, with a considerable impact on the reduction of the disease morbidity and mortality(3). The epithelial cells in the transition zone are accountable for PSA serum levels and the increase in prostatic volume is directly related to the increased level of such antigen. A number of factors may affect the PSA levels, and should therefore be considered in the interpretation of tests results. The most common causes for the increase in PSA levels are prostatitis, benign prostatic hyperplasia and prostate cancer(4). The screening by means of PSA testing is aimed at detecting the highest possible number of cases. In spite of its high sensitivity, this test has a low specificity for prostate cancer, which means that in order to achieve acceptable diagnosis rates, many patients are submitted to unnecessary biopsies. There is a doubtful zone traditionally considered as the PSA range between 4.1 and 10.0 ng/ml within which all patients are considered to be under suspicion of prostate cancer. Most recently, such zone has been expanded to levels between 2.6 and 10.0 ng/ml(5), which further increases the number of suspected cases. Within this doubtful zone, PSA testing has a low specificity, with approximately 75% of the prostate biopsies being negative for neoplasia(6). For an improved screening of candidates for such a procedure, new parameters are being analyzed. Some studies suggest that among those parameters, PSA density (PSAD), which is the ratio between the absolute PSA value and the prostate volume, might increase the specificity of the PSA test(7). The Unit of Interventional Ultrasonography of the Department of Imaging Diagnosis Department of Universidade Federal de São Paulo (Unifesp) averagely performs 120 prostate biopsies per month; approximately 70% of such biopsies are negative for neoplasia. Taking such data into consideration, and in an attempt to reduce the number of unnecessary biopsies, the authors have proposed the present study to analyze the profile of patients with PSA values between 2.6 and 10.0 ng/ml and submitted to prostate biopsies, with the purpose of identifying variables which might increase the PSA specificity, and thus avoiding unnecessary procedures. MATERIALS AND METHODS In the period between 2007 and 2009, a cross-sectional study was carried out with male patients with PSA levels ranging between 2.6 and 10.0 ng/ml, referred to the Unit of Interventional Ultrasonography of Hospital São Paulo to undergo prostate biopsy. The patients were evaluated according to the following parameters: age, prostate volume, PSA level, anatomopathological study - whenever positive for cancer, affected zones and Gleason classification for malignancy. The patients who signed a Term of Free and Informed Consent were included in the study that was duly approved by the Committee for Ethics in Research of the institution. Those patients whose PSA levels, prostate volume or anatomopathological results could not be evaluated as well as those who otherwise did not agree in participating in the study, were excluded. The ultrasonography equipment utilized was an EnVisor model (Philips; Eindhoven, Netherlands), with a 9 MHz transducer. The endorectal approach was utilized for prostate evaluation. The calculation of the prostate volume was performed by means of the formula as follows: AP × CC × LL × 0.523 where: AP is the anteroposterior diameter, CC is the craniocaudal diameter, and LL is the latero-lateral diameter (Figure 1).  Figure 1. Transrectal ultrasonography study with volume measurement. The PSAD is the result of the division of PSA by the prostate volume(7). The biopsies were performed by acquiring 12 fragments from the peripheral zone with 18 G needles, being two specimens from each sextant, one lateral and one medial. The specimens were placed in individual labeled vials, each one with the identification of the sextant from which they were taken, and were separately evaluated by the pathologist. In the cases that were positive for prostate cancer, the Gleason grading system for malignancy was utilized(8,9). The patient’s age, PSA values and prostate volumes were correlated with the presence of cancer. In the presence of cancer, the lesion location and malignancy grade were also correlated. In addition, the accuracy of PSA density in predicting prostate cancer in patients with PSA levels between 2.6 and 10.0 ng/ml was evaluated. For comparisons between groups, the Student’s t test and the non-parametric Mann-Whitney test were utilized for normal and non-normal data, respectively. The capability of PSAD in differentiating cancer patients from those without the disease was evaluated by means of ROC curve, and measurements of sensitivity and specificity, positive and negative predictive values (PPV and NPV), as well as positive and negative likelihood ratios (respectively, LR+ and LR-). The adopted significance level was 0.05. The utilized softwares were SPSS for Windows, version 17.0 and the RevMan 5.20. RESULTS From the 1,384 patients recruited in the period between 2007 and 2009, 102 were excluded because of the absence of data regarding prostate volume, PSA levels or anatomopathological results. Thus 1,282 patients remained in the study. Among the 1,282 patients submitted to prostate biopsy, the prevalence of cancer was 28.6%. The remaining 71.4% presented negative results for prostate cancer. Mean patients’ age was 65 years, ranging from 43 to 93 years. The patients group whose biopsies did not confirm prostate cancer had a mean age of 64.6 years, while the group with prostate cancer had a mean age of 69.6 years (Table 1). 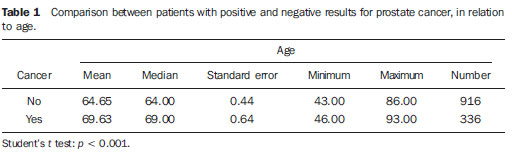 As the prostate volume was evaluated, the patients with positive results for prostate cancer presented a mean prostate volume of 41.4 cm3 while for those with negative results, the mean prostate volume was 56.9 cm3 (Table 2). 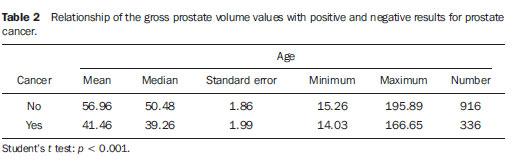 In the analysis of PSA levels, the patients with positive results for prostate cancer presented a mean value of 8.9 ng/ml, while those with negative results presented a mean value of 6.1 ng/ml. Mean PSA values for both groups were within the range of 2.6 to 10.0 ng/ml, which corresponded to the evaluated doubtful zone. As the PSA levels were broken-down into two ranges of incidence, from 2.6 to 4.0 ng/ml and from 4.1 to 10.0 ng/ml, one observed that in the first one there were 217 patients (17% of the total), 24 (11%) of them with cancer. In the second range of incidence there were 1,065 patients (83% of the total), 32.1% of them positive for cancer. As the PSAD was evaluated, it was observed that the patients with prostate cancer presented a mean value of 0.31 ng/ml/cc, while those with negative results presented a mean value of 0.10 ng/ml/cc (Table 3). 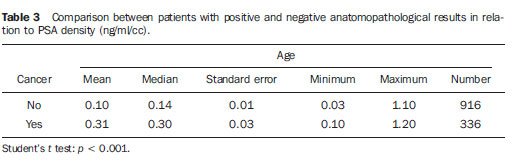 By utilizing the PSAD cutoff point of 0.15 ng/ml/cc as a cancer positivity criterion, as suggested by the literature(7), the area under the ROC curve was 0.720. For such value, a specificity of 74% was obtained (CI 95%: 71-77%) and sensitivity was 70% (CI 95%: 65-74%). When it comes to cancer detection, one should minimize the number of false positive results and prioritize sensitivity. In the present case, aiming at increasing sensitivity, it is necessary to reduce the cutoff point. With the value of 0.09 ng/ml/cc, a sensitivity of 84% was obtained (CI 95%: 80-87%), the specificity was 75% (CI 95%: 72-78%) and the area under the ROC curve was 0.794 (Figure 2). The LR’s were calculated for the two selected cutoff points. For the 0.15 ng/ml/cc criterion, a LR+ of 2.72 and a LR- of 0.41 were found. On the other hand, for the 0.09 ng/ml/cc criterion, the LR+ and LR- of 3.36 and 0.21 respectively, were found. 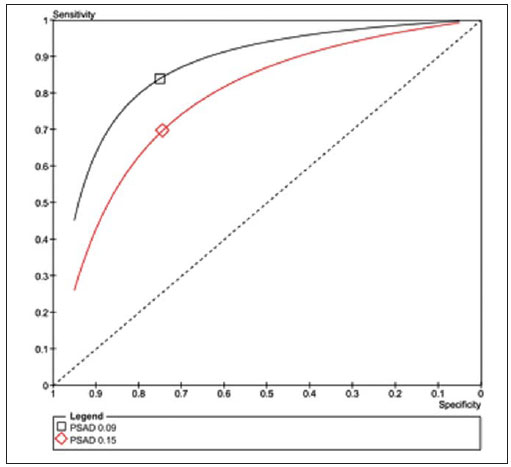 Figure 2. Comparison between the ROC curves for the 0.15 ng/ml/cc and 0.09 ng/ml/cc cutoff points. In order to evaluate the relation between the PSAD performance and age in the prediction of prostate cancer, the patients were divided into three subgroups according to the distribution tertiles, and the discrimination power of PSAD was evaluated by means of the area under the ROC curve. In all the analyses, the discrimination seemed to be better in the older patients, however with no statistical significance (Table 4). 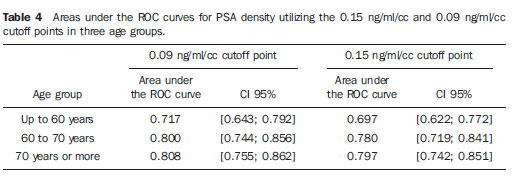 By analyzing the neoplasia location and the grading attributed by the pathologist according to the Gleason classification, a comparative analysis of such data could be carried out. The result is shown at a chart (Figure 3), in which one observes that no significant difference was found between the location of the neoplasia manifestation and its malignancy grade. 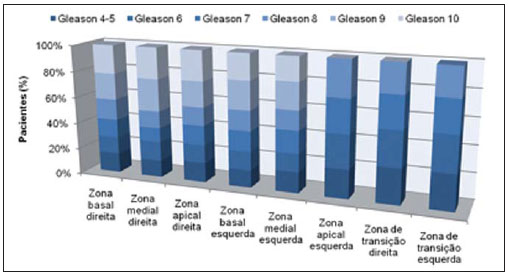 Figure 3. Chart with the Gleason classification at different prostate zones. DISCUSSION The present study evaluating the profile of patients submitted to prostate biopsies highlights the importance of PSAD and its impact on the reduction of the number of unnecessary prostate biopsies, with their consequential complications and costs. There is a widespread consensus that the PSA level testing is the best available method for prostate cancer screening. Its utilization increases the detection of prostate cancer in up to 81% as compared with digital rectal examination alone(3,4,10). In cases of increased PSA, it is difficult to differentiate cancer from benign prostatic hyperplasia, particularly in patients with intermediate levels between 2.6 and 10.0 ng/ml. In order to optimize the PSA effectiveness as a diagnostic test within that PSA range, several options were proposed with a view on increasing the specificity of the test and avoiding unnecessary biopsies, which occurs approximately 75% of the cases. In the present study, the profiles of patients submitted to prostate biopsy were outlined, identifying variables that, in association with PSA values ranging between 2.6 and 10.0 ng/ml, would increase its specificity. One observed that the prevalence of cancer proportionally increased with age. More than 65% of all prostate cancers will be diagnosed in men above 65 years of age(1,2), as observed in the present study, in which 72% of the patients with cancer were 65 years old or older. As prostate volume was analyzed, one could observe that, in patients with cancer, the prostate volumes (41.4 cm3) were, on average, smaller than in those patients with negative results for cancer (59.9 cm3). Such data is corroborated by studies in which prostates with small volume, suspicious at digital rectal examination and in patients with elevated or intermediate PSA levels, are significantly associated with anatomopathological evidences of adenocarcinoma(4,11). Prostate specific antigen (PSA) was first isolated by Wang in 1979(12). It is produced by both normal and neoplastic prostatic cells, and its serum concentration is significantly related to prostate cancer volume(3,6). The PSA levels are objective and easily reproducible(6). According to some studies, patients with PSA levels below 4.0 ng/ml are considered as at low risk for prostate adenocarcinoma(13,14). In this case, values < 4.0 ng/ml would be considered as normal and the interval between 4.1 and 10.0 ng/ml would be the doubtful or intermediate interval. In the present study, 17% of the patients presented PSA levels < 4.0 ng/ml, and of those patients, 11% presented results positive for cancer. Such values are similar to data reported in other studies(15,16), which have demonstrated a lower prevalence of cancer at the 2.6 to 4.0 ng/ml PSA level range. On the other hand, at the 4.1 to 10.0 ng/ml PSA level range, corresponding to 83% of the patients, the prevalence of cancer reached 32.1%. The authors observed that the mean PSA value in the individuals with cancer was 8.9 ng/ml, which is higher than 6.1 ng/ml found in the individuals with results negative for cancer. In spite of the fact that the present study comprised a range of results that can be considered as intermediate, in which all the patients are suspicious for cancer, a higher mean PSA concentration was observed in individuals with cancer, a fact corroborated by other studies(13,16). In 1992, Benson et al.(7) introduced the PSAD concept as a method to increase the PSA testing specificity, by dividing the total PSA value by the total prostate volume. In studying 127 male patients, that analysis proposed that, in spite of a group of patients with similar intermediate PSA levels, stratifying such values according to prostate volume, would lead to a more significant correlation with benign and malignant processes, consequently reducing the number of unnecessary biopsies, without compromising the cancer detection. Although some authors recognize the usefulness of PSAD in the differentiation between cancer and benign prostatic hyperplasia(11,17), others put its validity into question(18,19), since this method alone, with the recommended cutoff point of 0.15 ng/ml/cc(7), has a sensitivity of approximately 60%. Some years later, Catalona et al.(6), in a multicentric study with 773 men, suggested that the PSAD value be lowered to 0.078ng/ml/cc, a value at which 95% of the tumors would be detected. In the present study, the patients with positive results for cancer presented a mean PSAD value of 0.31 ng/ml/cc, while those with negative results presented a mean PSAD value of 0.10 ng/ml/cc. If a PSAD cutoff point of 0.15 ng/ml/cc was utilized, the test sensitivity would have been 65%, a low value for a screening test. On the other hand, by reducing such value to 0.09 ng/ml/cc, a sensitivity similar to the value of 83% obtained by Djavan et al.(20) would be found. The specificity with these two values would be similar. For a cancer screening test, the high sensitivity (83.8%) and PPV (92.0%) of the method should be prioritized. Thus, by choosing the cutoff point of 0.09 ng/ml/cc, the number of false negative results would be reduced. In the study with the PSA level between 2.6 and 10.0 ng/ml, the number of patients submitted to unnecessary biopsy corresponded to 71.4% of all procedures. With the utilization of PSAD, this percentage could be reduced to less than 30% for both cutoff points. As the LR was utilized, values for LR+ that indicate a moderate change in the probability of cancer at both cutoff points were found. However, for LR-, the authors found values indicating a small change in the probability of cancer for the cutoff point of 0.15 ng/ml/cc (0.40) and moderate change for the 0.09 ng/ml/cc (0.22) cutoff point. Taking this evaluation into consideration, the 0.09 ng/ml/cc cutoff point would be the most appropriate. The anatomopathological results positive for prostate cancer were analyzed by pathologists who utilized the Gleason classification for malignancy. For being an analysis that can be made in all fragments, it would be possible to find out where the more and less differentiated tumors occurred. In the present study, no significant difference was observed between the location of the neoplasias and their malignancy grading. In the present study, it was observed that the patients with prostate cancer were on average older, with higher PSA and PSAD values, and had a smaller prostate volume. The present data indicate a good PSAD accuracy in the prediction of prostate cancer, with the potential of substantially reducing the number of unnecessary biopsies. REFERENCES 1. Instituto Brasileiro de Geografia e Estatística; Ministério do Planejamento, Orçamento e Gestão. Estimativas populacionais 1980-2010: Brasil, regiões geográficas e unidades da federação [homepage na Internet]. Rio de Janeiro (Brasil): IBGE; 2010. [citado em 15 de junho de 2010]. Disponível em: http://www.ibge.gov.br 2. Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225-49. 3. Gomes R, Rebello LEFS, Araújo FC, et al. A prevenção do câncer de próstata: uma revisão da literatura. Rev CS Col. 2008;13:235-46. 4. Nickel JC. Inflammation and benign prostatic hyperplasia. Urol Clin North Am. 2008;35:109-15. 5. Catalona WJ, Smith DS, Ornstein DK. Prostate cancer detection in men with serum PSA concentrations of 2.6 to 4.0 ng/mL and benign prostate examination. Enhancement of specificity with free PSA measurements. JAMA. 1997;277:1452-5. 6. Catalona WJ, Southwick PC, Slawin KM, et al. Comparison of percent free PSA, PSA density, and age-specific PSA cutoffs for prostate cancer detection and staging. Urology. 2000;56:255-60. 7. Benson MC, Whang IS, Pantuck A, et al. Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer. J Urol. 1992;147(3Pt2):815-6. 8. Gleason DF. Classification of prostate carcinomas. Cancer Chemother Rep. 1966;50:125-8. 9. Sogani PC, Israel A, Lieberman PH, et al. Gleason grading of prostate cancer: a predictor of survival. Urology. 1985;25:223-7. 10. Catalona WJ, Richie JP, Ahmann FR, et al. Comparison of digital rectal examination and serum prostate specific antigen in the early detection of prostate cancer: results of a multicenter clinical trial of 6,630 men. J Urol. 1994;151:1283-90. 11. Babaian RJ, Fritsche HA, Evans RB. Prostate-specific antigen and the prostate gland volume: correlation and clinical application. J Clin Lab Anal. 1990;4:135-7. 12. Wang MC, Valenzuela LA, Murphy GP, et al. Purification of a human prostate specific antigen. 1979. J Urol. 2002;167(2Pt2):960-5. 13. Dennis LK, Resnick MI. Analysis of recent trends in prostate cancer incidence and mortality. Prostate. 2000;42:247-52. 14. Catalona WJ, Smith DS, Ratliff TL, et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med. 1991;324:1156-61. 15. Colberg JW, Smith DS, Catalona WJ. Prevalence and pathological extent of prostate cancer in men with prostate specific antigen levels of 2.9 to 4.0 ng/ml. J Urol. 1993;149:507-9. 16. Krumholtz JS, Carvalhal GF, Ramos CG, et al. Prostate specific antigen cutoff of 2.6 ng/mL for prostate cancer screening is associated with favorable pathologic tumor features. Urology. 2002;60:469-74. 17. Veneziano S, Pavlica P, Querzé R, et al. Correlation between prostate-specific antigen and prostate volume, evaluated by transrectal ultrasonography: usefulness in diagnosis of prostate cancer. J Urol. 1990;18:112-6. 18. Lookner DH, Crawford ED, Donohue RE, et al. Prostate-specific antigen and prostate-specific antigen density in cases of pathologically proven prostate cancer. J Urol. 1993;149:414A. 19. Brawer MK, Aramburu EA, Chen GL, et al. The inability of prostate specific antigen index to enhance the predictive the value of prostate specific antigen in the diagnosis of prostatic carcinoma. J Urol. 1993;150(2Pt1):369-73. 20. Djavan B, Zlotta AR, Byttebier G, et al. Prostate specific antigen density of the transition zone for early detenction of prostate cancer. J Urol. 1998;160:411-9. 1. Master, Head for Coordination of Unit of Non-Vascular Intervention, Department of Imaging Diagnosis at Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 2. PhD, Head for Coordination of Unit of Ultrasonography, Department of Imaging Diagnosis at Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 3. PhD, Affiliate Professor, Department of Imaging Diagnosis at Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 4. PhD, MD, Physician Assistant, Department of Imaging Diagnosis at Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 5. Titular Professor, Department of Imaging Diagnosis at Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. Mailing Address: Dr. Hugo Alexandre Sócrates de Castro Rua Caconde, 281, ap. 12, Jardim Paulista São Paulo, SP, Brazil, 01425-011 E-mail: halsoc@gmail.com Received May 2, 2011. Accepted after revision June 7, 2011. Study developed at Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554