Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 3 - May / June of 2011
Vol. 44 nº 3 - May / June of 2011
|
ORIGINAL ARTICLE
|
|
Contribution of ultrasonography to the diagnosis of chronic hepatitis C histopathological changes, with emphasis on hepatic steatosis – Part I |
|
|
Autho(rs): Marcia Wang Matsuoka1; Ilka Regina Souza de Oliveira2; Azzo Widman3; Arnaldo Zanoto4; Sérgio Keidi Kodaira5; Leonardo Ellery Marinho6; Wilson Jacob Filho7; Giovanni Guido Cerri8 |
|
|
Keywords: Ultrasonography; Chronic hepatitis C virus infection; Hepatic steatosis; Liver biopsy. |
|
|
Abstract: INTRODUCTION
Ultrasonography is an imaging method of first choice because of its noninvasiveness, wide availability and for practicity of application(1—3). In the liver, the following aspects are evaluated: biometry, shape, contours, intrahepatic vessels distribution, and the echographic characteristics of the parenchyma: echotexture, echogenicity and attenuation. At ultrasonography, the normal hepatic parenchyma presents homogeneous echotexture and intermediate echogenicity, usually iso- or hyperechogenic in relation to the renal cortex and hypoechogenic in relation to the splenic tissue. The attenuation of the acoustic beam is subtle, allowing a good identification of intrahepatic vessels and of the diaphragm in the posterior region of the liver(4—6). In inflammatory liver diseases, the sonographic findings vary according to the stage of the disease, being usually normal at the acute stage. At the chronic stage, with the onset of cirrhosis, irregularities in the hepatic contours, as well as changes in the characteristics of parenchymal tissues may be observed(7,8). Among the different types of hepatitis, the one caused by the C virus has been object of clinical and sonographic investigation, given its high prevalence in the population as a whole(9—11). Such a disorder that affects 170 million people around the world, may present a variable progression: 30% of the patients will develop mild and stable chronic hepatitis for decades; 40% will present different degrees of fibrosis without the development of cirrhosis along the disease progression; and 30% will present a severe progression of the disease, with development of cirrhosis(12). Among the patients who develop cirrhosis, 20% will present complications caused by portal hypertension with the disease progression, and 1% to 7% may develop hepatocellular carcinoma(10,11,13,14). Histopathological signs indicative of hepatitis C include architectural changes in the hepatic lobe, necroinflammation components and hepatic steatosis (HS), defined as a frequently reversible metabolic disorder characterized by fatty liver infiltration resulting from accumulation of triglycerides in within the hepatocytes(7,15). In patients with hepatitis C, necropsy studies have demonstrated HS incidence in 31% to 72% of cases, and liver biopsies have demonstrated the presence of HS in approximately 50% of the cases(16). However, the role of HS in the onset, physiopathology and progression of the hepatic disease is not well established yet, with the relationship between HS, necroinflammatory activity and development of fibrosis being described(17—20). Hepatic biopsy is considered as the “gold standard” for the diagnosis and staging of hepatitis C and HS, and is also relevant for therapeutic guidance in such disorders(11,21,22). The evaluation of histopathological aspects of hepatitis C and HS can be performed by means of ultrasonography in a limited manner. As regards HS, both the echographic characteristics of the parenchyma and the liver biometry are usually taken into consideration. Considering the echographic characteristics of the hepatic parenchyma, the diagnosis of HS is based on a gradual increase in echogenicity and in attenuation of the acoustic beam. Textural changes, when present, are subtle and of minor relevance. However, such signs may also be present in cases of fibrosis and/or hepatic inflammatory processes, thus limiting the performance of the sonographic method for the diagnosis of HS(7,23—35). Additionally, the analysis of echographic aspects of the hepatic parenchyma presents a subjective component, obtaining conflicting results with respect to the specific value of such method for the diagnosis of HS, with sensitivity rates ranging between 55% and 95%(25,26,36). The present study was developed with a view on the controversial results of the HS diagnosis by ultrasonography. Initially, the results obtained exclusively by means of the analysis of echographic changes of the hepatic parenchyma will be presented (Part I). Sequentially, the results obtained by means of the joint analysis of the above mentioned echographic criteria and the biometric data regarding both the liver and the subcutaneous fat layer at the right hypochondrium will be presented (Part II). MATERIALS AND METHODS The present study was approved by the Committee for Ethics in Research (CAPPesq) of the Board of Clinical Directors of Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. The study sample comprised 192 consecutive patients with clinical and laboratory diagnosis of exclusively chronic C virus hepatitis referred to the Day Hospital of the institution for US-guided liver biopsy in the period between July of 2002 and May of 2003. In the studied population, the arithmetic mean age and respective standard deviation was 43.22 ± 13.21 years. According to the Kolmogorov-Smirnov test, the age distribution was normal, with sample homogeneity being observed, allowing the comparison between groups. With the purpose of correlating the sonographic findings and histopathological changes in the liver in chronic hepatitis C, the patients were divided into two groups: a) patients with sonographic changes; b) patients without sonographic changes. The means and standard deviations of ages in the two groups were, respectively, 45.03 ± 12.57 and 42.42 ± 13.46 years, with no statistically significant difference between both groups (unpaired t = 1.27; p = 0.207050). Among the 192 patients, 91 (47.4%) were men with 43.05 ± 12.95 years of age and 101 (52.6%) were women with 43.38 ± 13.51 years of age. There was no statistically significant difference between the proportion of both genders in the two groups (χ2c = 0.02; p = 0.88454) and between the age means (unpaired t = 0.17; p = 0.86693), demonstrating sample homogeneity and thus allowing the comparison between them. Sonographic studies and liver biopsies were performed, each one by a same specialist. In the present study, HS was sonographically classified as follows: — mild: hepatic parenchyma with subtle increase in echogenicity and sound beam attenuation, with subtle decrease in the visualization of the diaphragm and intrahepatic vascularization; — moderate: hepatic parenchyma with moderate increase in echogenicity and sound beam attenuation, with moderate decrease in the visualization of the diaphragm and intrahepatic vascularization; — severe: hepatic parenchyma with a great in echogenicity and sound beam attenuation, with a marked or complete loss of the visualization of the diaphragm and of the intrahepatic vascularization(5,7); The liver parenchyma echotexture was also evaluated, being classified as homogeneous or heterogeneous. The group of patients with altered sonographic pattern of the liver parenchyma was defined by the simultaneous presence of at least two of the analyzed parameters: a) increased echogenicity (subtle, moderate or marked); b) heterogeneous echotexture; c) increased attenuation of the acoustic beam (subtle, moderate or marked). Previously to the liver biopsy, the patients were submitted to ultrasonography with the purpose of localizing the best site for puncture. Ultrasonography studies were performed in a Toshiba equipment model SSA-240A® (Toshiba; Tokyo, Japan) with a 3.5 MHz convex transducer. The study protocol was the following: a) total gain: adjusted in such a way that the liquid contents of the gallbladder and the blood in the inferior vena cava were non-echogenic. Gain curve adjusted to the neutral position; b) patient positioning: horizontal dorsal decubitus; c) transducer scan performed on the right hypochondrium in the longitudinal, transverse and oblique planes. The patients with characteristics of focal steatosis were not included in the study sample. The liver biopsy specimens were analyzed according to the criteria of the 1999 Brazilian Pathology Consensus of Sociedade Brasileira de Patologia (Brazilian Pathology Society). Such Consensus evaluates chronic hepatitis by means of the staging of present architectural changes, grades the activity of the ongoing condition by means of the necroinflammatory activity evaluation, and describes concomitant changes such as HS, lymphoid infiltrate, ductal aggression and iron deposition. Moreover, according to the classification adopted by the Brazilian Pathology Consensus of 2002, the hepatic involvement by the C virus is classified as reactive liver, chronic hepatitis itself, and cirrhosis(15). In order to allow the statistical analysis, the groups corresponding to the necroinflammatory activity (portal activity, periportal activity and parenchymal activity) usually graded from 0 to 4 separately, were subdivided according to the sum of the grading for each one of such factors attributed by pathological anatomy, establishing 13 subgroups (0 to 12). Subsequently, such subgroups were rearranged into four groups, in order to allow the comparison of necroinflammatory activity, HS and architectural changes according to a single scale. The presence of HS was also graded as 0, 1, 2, 3, and 4, corresponding to increasing intensity of infiltration of fat particles in the liver, from mild to severe. For the purpose of statistical analysis, 5% (α = 0.05) was adopted as significance level. RESULTS Among the 192 patients, 59 (30.7%) presented an altered sonographic pattern, and 133 (69.3%), presented unaltered sonographic pattern. Histopathological patterns The groups with and without sonographic changes were compared as regards histopathological patterns (architectural changes, necroinflammatory activity and HS). Statistically significant differences were observed between such groups for architectural changes and HS, and not for necroinflammation (Mann-Whitney nonparametric test). 1. Architectural changes (structural) The quantification of the structural histopathological changes in the groups with and without sonographic changes is shown on Table 1. 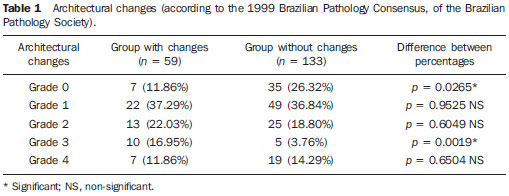 The chi-square test (χ2) was performed for analysis of joint variation in proportions (0, 1, 2, 3, 4) between the two groups (χ2 = 13.40; p = 0.00949*). Proportions for each quantification between the groups with and without sonographic changes were analyzed by the test of difference between proportions, with a statistically significant difference observed at grade 0 (normal) and grade 3 (pre-cirrhosis). No difference was observed in the quantification 1 and 2 and also on 4, which corresponds to cirrhosis. 2. Necroinflammation The means of necroinflammatory changes were analyzed, with no statistically significant difference in the quantification of necroinflammatory activity being found between the groups with and without sonographic changes (Mann-Whitney non-parametric test). 3. Steatosis Of the 192 patients, 81 (42.2%) presented steatosis at the histopathological study, while 111 (57.8%) did not. The present casuistry demonstrated a reduced number of patients classified at each one of the HS grades (0, 1, 2, 3 and 4). The results demonstrated a predominance of mild grade HS in both patient groups (with and without sonographic changes), an HS was prevalent in the group without sonographic changes, with an estimated prevalence of 95.5%. Considering the above mentioned results, which characterize the difficulty of the method for diagnosing mild grade HS, and, with the objective of allowing the statistical analysis, the different HS grades resulting from the histopathological analyses of the present casuistry were divided into two subgroups: I) grades 0 and 1; II) grades 2, 3 and 4 (Table 2). 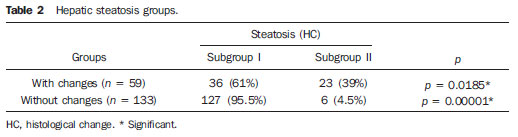 Thus, as presence of HS in grades 2, 3, and 4 (moderate and severe) is considered, the analysis of the sample demonstrates a statistically significant difference between the groups with and without sonographic changes, with such difference being greater in the group with changes. A statistically significant difference was observed between the HS proportions in the groups with and without sonographic changes and between the HS proportions in subgroups I and II (χ2c = 35.23; p = 0.00001*), with sensitivity of 79.3%, specificity of 77.9%, positive predictive value of 39.0%, negative predictive value of 95.5%, rate of agreement of 78.1% and Cohen kappa coefficient (κ) = 0.4015, with a regular agreement. Sonographic parameters Among the three sonographic parameters (echotexture, echogenicity and acoustic beam attenuation), attenuation presented greater correlation with HS, as compared with the joint analysis of the same parameters by means of the non-parametric Spearman’s rank correlation (Table 3). 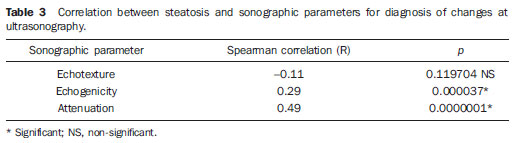 Figures 1, 2 and 3 illustrate the different HS grades observed at ultrasonography. 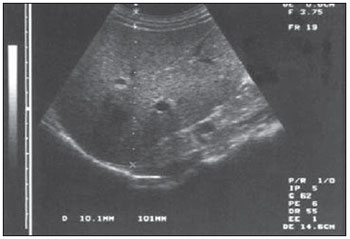 Figure 1. Mild hepatic steatosis: ultrasonography of the right hepatic lobe with signs of subtle increase in echogenicity and attenuation of the acoustic beam; homogeneous texture. 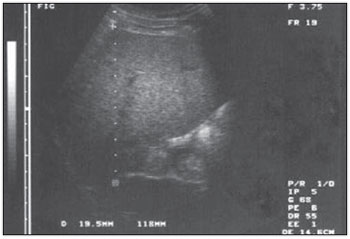 Figure 2. Moderate hepatic steatosis: ultrasonography of the right hepatic lobe with moderate increase in echogenicity and attenuation of the acoustic beam; finely heterogeneous texture. 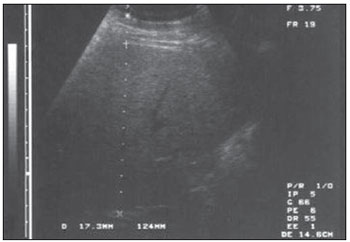 Figure 3. Severe hepatic steatosis: ultrasonography of the right hepatic lobe with marked increase in echogenicity and attenuation of the acoustic beam; impaired texture evaluation. DISCUSSION The literature has presented conflicting references with respect to the correlation between sonographic findings and histopathological findings of cirrhosis and HS. The development of the present study was favored by the possibility of comparing sonographic findings with histopathological findings, during US-guided percutaneous liver biopsy, in a population of hepatitis C patients. Between the two established patient groups (patients with and without sonographic changes), a statistically significant difference was observed between the architectural changes and HS, and non‑statistically significant difference as regards necroinflammatory activity. In the literature review, no study was found reporting separate correlation between such method and necroinflammation. As architectural changes are considered, the patients group with sonographic changes and the group without sonographic changes presented statistically significant differences in fibrosis grades 0 and 3. No statistically significant difference was observed in grades 1, 2, and 4 of architectural changes. A comprehensive comparison between such results and those reported in the literature could not be undertaken because of the absence of other systematized studies on sonographic and histopathological correlation with respect to architectural changes and their different grades. However, considering exclusively grade 4 architectural changes (cirrhosis), the obtained results are in agreement with data reported in the literature, with respect to the non-existence of statistically significant sonographic difference in this grade of architectural change(23,25,26,29,34,35,37—39). Thus, the present study demonstrated that the characterization of different grades of architectural changes of the hepatic parenchyma poses limitations to ultrasonography. As regards HS, the histopathological analysis demonstrated its presence in 42.2% of the patients, in agreement with data in the literature that report its presence in approximately 50% of the cases of chronic hepatitis C(19,20,39). A statistically significant difference was observed between the groups with and without sonographic changes, exclusively regarding the proportion of moderate and severe HS that was greater in the group with sonographic changes, demonstrating the capability of the method in identifying such steatosis grades (grades 2, 3 and 4). The difficulty of ultrasonography in diagnosing mild grade HS was demonstrated in the present study by the predominance of the mild grade HS both in the group with sonographic changes as well as in the group without sonographic changes. The results in the present study are in agreement with other authors who report the high sensitivity of ultrasonography in the diagnosis of moderate and severe grades HS, and reduced sensitivity for the mild grades(7,24—33). However, other studies report that it is not possible to diagnose HS by means of ultrasonography, differently from the obtained results(25,32,35). It is important to highlight that, among the evaluated sonographic criteria, acoustic beam attenuation was the criterion that presented the highest correlation with HS. Echogenicity, on its turn, presented correlation with HS, although less significantly, while echotexture did not present any correlation with HS (Table 3). In the literature, data related to echogenicity in the diagnosis of HS are conflicting. Some authors associate the increase in echogenicity with the diagnosis of this disorder(40,41), while others affirm that there is correlation between hyperechogenicity and fibrosis or necroinflammation(32,35). As regards attenuation, some authors consider that such parameter would be a good criterion for the diagnosis of HS(22,38,42). Finally, it is observed that the result of the utilization of ultrasonography in the diagnosis of HS may vary according to the performance of each one of the utilized parameters: echotexture, echogenicity and attenuation. In the present study, attenuation was the most relevant parameter in the diagnosis of HS. CONCLUSIONS The results of the present study demonstrated that, considering the histopathological changes that are present in hepatitis C, ultrasonography was not capable of differentiating necroinflammation, and presented limitations in the diagnosis of architectural changes. As regards HS, the statistical analysis demonstrated a regular agreement with the presence of HS observed at the histopathological analysis. The capability of the method to demonstrate the probability of inexistence of HS should be highlighted, considering the specificity of 77.9% and, mainly, the negative predictive value of 95.5%. REFERENCES 1. Meire H, Cosgovre D, Dewbury K, et al. Abdominal and general utrasound. 2nd ed. London: Churchill Livingstone; 2001. 2. Kodaira SK. Física. In: Cerri GG, editor. Ultra-sonografia abdominal. Rio de Janeiro, RJ: Revinter; 2002. p. 1—30. 3. Joy D, Thava VR, Scott BB. Diagnosis of fatty liver disease: is biopsy necessary? Eur J Gastroenterol Hepatol. 2003;15:539—43. 4. Palmer PE. Manual de diagnóstico em ultra-sonografia. Rio de Janeiro, RJ: Revinter; 1999. 5. Withers CE, Wilson SR. O fígado. In: Rumack CM. Tratado de ultra-sonografia diagnóstica. Rio de Janeiro, RJ: Guanabara Koogan; 1998. p.73—130. 6. Rodrigues MB, Amaro Jr E, Kodaira SK. Anatomia e ultra-sonografia do abdome. In: Cerri GG, editor. Ultra-sonografia abdominal. Rio de Janeiro, RJ: Revinter; 2002. p. 31—53. 7. Machado MM, Rosa AC, Cerri GG. Doenças hepáticas difusas, hipertensão portal e transplante de fígado. In: Cerri GG, editor. Ultra-sonografia abdominal. Rio de Janeiro, RJ: Revinter; 2002. p. 55—124. 8. Ralls PW, Jeffrey RB Jr, Kane RA, et al. Ultrasonography. Gastroenterol Clin North Am. 2002;31:801—25. 9. Seeff LB. The natural history of chronic hepatitis C virus infection. Clin Liver Dis. 1997;1:587—602. 10. Poynard T, Ratziu V, Benmanov Y, et al. Fibrosis in patients with chronic hepatitis C: detection and significance. Semin Liver Dis. 2000;20:47—55. 11. Dove LM. A general approach to the management of chronic hepatitis C. Gastroenterol Clin North Am. 2004;33:463—77. 12. Seeff LB. Natural history of hepatitis C. In: Schiff ER, Hoofnagle JH, editors. Update on viral hepatitis. AASLD postgraduate course 2000. p. 112—8. 13. Jármay K, Karácsony G, Ozsvár Z, et al. Assessment of histological features in chronic hepatitis C. Hepatogastroenterology. 2002;49:239—43. 14. Zheng RQ, Wang QH, Lu MD, et al. Liver fibrosis in chronic viral hepatitis: an ultrasonographic study. World J Gastroenterol. 2003;9:2484—9. 15. Gayotto LC, Comitê SBP/SBH. Visão histórica e consenso nacional sobre a classificação das hepatites crônicas. GED. 2002;19:137—40. 16. Yoon EJ, Hu KQ. Hepatitis C virus (HCV) infection and hepatic steatosis. Int J Med Sci. 2006;3:53—6. 17. Adinolfi LE, Gambardella M, Andreana A, et al. Steatosis accelerates the progression of liver damage of chronic hepatitis C patients and correlates with specific HCV genotype and visceral obesity. Hepatology. 2001;33:1358—64. 18. Patton HM, Patel K, Behling C, et al. The impact of steatosis on disease progression and early and sustained treatment response in chronic hepatitis C patients. J Hepatol. 2004;40:484—90. 19. Wyatt J, Baker H, Prasad P, et al. Steatosis and fibrosis in patients with chronic hepatitis C. J Clin Pathol. 2004;57:402—6. 20. Negro F. Mechanisms and significance of liver steatosis in hepatitis C virus infection. World J Gastroenterol. 2006;12:6756—65. 21. Dao T, Lecointe I, Galateau F, et al. Contribution of liver biopsy and serology of hepatitis C virus to the diagnosis of a moderate and prolonged elevation of aminotransferases. Gastroenterol Clin Biol. 1993;17:37—43. 22. Fontana RJ, Lok AS. Noninvasive monitoring of patients with chronic hepatitis C. Hepatology. 2002;36(5Suppl1):S57—64. 23. Foster KJ, Dewbury KC, Griffith AH, et al. The accuracy of ultrasound in the detection of fatty infiltration of the liver. Br J Radiol. 1980;53:440—2. 24. Joseph AE, Dewbury KC, McGuire PG. Ultrasound in the detection of chronic liver disease (the “bright liver”). Br J Radiol. 1979;52:184—8. 25. Celle G, Savarino V, Picciotto A, et al. Is hepatic ultrassonography a valid alternative tool to liver biopsy? Report on 507 cases studied with both techniques. Dig Dis Sci. 1988;33:467—71. 26. Needleman L, Kurtz AB, Rifkin MD, et al. Sonography of diffuse benign liver disease: accuracy of pattern recognition and grading. AJR Am J Roentgenol. 1986;146:1011—5. 27. Zwiebel WJ. Sonographic diagnosis of diffuse liver disease. Semin Ultrasound CT MR. 1995;16:8—15. 28. Andrade RJ, García-Escaño MD. Hepatic steatosis. Med Clin (Barc). 2000;114:574—6. 29. Ros PR, Mortele KJ. Diffuse liver disease. Clin Liver Dis. 2002;6:181—201. 30. Hamaguchi M, Kojima T, Itoh Y, et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102:2708—15. 31. Hirche TO, Ignee A, Hirche H, et al. Evaluation of hepatic steatosis by ultrasound in patients with chronic hepatitis C virus infection. Liver Int. 2007;27:748—57. 32. Perez NE, Siddiqui FA, Mutchnick MG, et al. Ultrasound diagnosis of fatty liver in patients with chronic liver disease: a retrospective observational study. J Clin Gastroenterol. 2007;41:624—9. 33. van Werven JR, Marsman HA, Nederveen AJ, et al. Assessment of hepatic steatosis in patients undergoing liver resection: comparison of US, CT, T1-weighted dual-echo MR imaging, and point-resolved 1H MR spectroscopy. Radiology. 2010;256:159—68. 34. Taylor KJ, Riely CA, Hammers L, et al. Quantitative US attenuation in normal liver and in patients with diffuse liver disease: importance of fat. Radiology. 1986;160:65—71. 35. Hepburn MJ, Vos JA, Fillman EP, et al. The accuracy of the report of hepatic steatosis on ultrasonography in patients infected with hepatitis C in a clinical setting: a retrospective observational study. BMC Gastroenterol. 2005;5:14. 36. Lupsor M, Badea R. Imaging diagnosis and quantification of hepatic steatosis: is it an accepted alternative to needle biopsy? Rom J Gastroenterol. 2005;14:419—25. 37. Kutcher R, Smith GS, Sen F, et al. Comparison of sonograms and liver histologic findings in patients with chronic hepatitis C virus infection. J Ultrasound Med. 1998;17:321—5. 38. Lu ZF, Zagzebski JA, Lee FT. Ultrasound backscatter and attenuation in human liver with diffuse disease. Ultrasound Med Biol. 1999;25:1047—54. 39. Matos CA, Perez RM, Pacheco MS, et al. Steatosis in chronic hepatitis C: relationship to the virus and host risk factors. J Gastroenterol Hepatol. 2006;21:1236—9. 40. Tchelepi H, Ralls PW, Radin R, et al. Sonography of diffuse liver disease. J Ultrasound Med. 2002;21:1023—32. 41. Palmentieri B, de Sio I, La Mura V, et al. The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Dig Liver Dis. 2006;38:485—9. 42. Gaitini D, Baruch Y, Ghersin E, et al. Feasibility study of ultrasonic fatty liver biopsy: texture vs. attenuation and backscatter. Ultrasound Med Biol. 2004;30:1321—7. 1. PhD, MD, Physician Assistant at Instituto da Criança (ICr) do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. 2. PhD, MD, Docent at Department of Radiology, Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil. 3. PhD, MD, Supervising Physician Assistant at Division of Digestive System Surgery II, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. 4. Senior Assistant Professor, Division of Surgical Technique and Experimental Surgery, Department of Surgery, Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil. 5. PhD, MD, Physician Assistant at Instituto de Radiologia (InRad), Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. 6. MD, Specialist in Imaging Diagnosis of the Center of Computed Tomography at Hospital Samaritano, São Paulo, SP, Brazil. 7. Titular Professor, Director for the Unit of Geriatrics, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. 8. Titular Professor, Department of Radiology, Faculdade de Medicina da Universidade de São Paulo (FMUSP), General Director, Instituto do Câncer do Estado de São Paulo (Icesp), São Paulo, SP, Brazil. Mailing Address: Dra. Marcia Wang Matsuoka Avenida Engenheiro Luiz Gomes Cardim Sangirardi, 770, ap. 101, Vila Mariana. São Paulo, SP, Brazil, 04112-080 E-mail: mwmatsuoka@yahoo.com.br Received November 29, 2010. Accepted after revision May 17, 2011. Study developed at Instituto de Radiologia (InRad) do Hospital das Clínicas (HC) da Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554