INTRODUCTION
In contrast with colonic diverticular disease, non colonic diverticula are much rarer. Reports in the literature indicate an incidence of these findings in less than 1% of autopsies(1–5). Small bowel diverticulosis is many times asymptomatic and may be incidentally found on imaging studies, either on contrast-enhanced series of the upper digestive tract or computed tomography (CT), surgeries and autopsies(3,4). As the disease becomes symptomatic, acute presentation of diverticulitis is observed in the greatest majority of cases. Jejunal diverticulitis is a rare condition but should always be considered in cases of elderly patients with abdominal pain. Men are most frequently affected than women (2:1 ratio) at the 6th and 7th decades of life(1,4,6–8).
In the present report, the authors describe a case of jejunal diverticulitis with intestinal obstruction, highlighting the most typical imaging findings and possible complications of this condition.
CASE REPORT
A male, 70-year-old patient was admitted to the emergency service with a threeday history of diffuse abdominal pain, with interrupted fecal and gaseous elimination. At clinical examination, the patient presented fever, prostration, with diffuse abdominal pain at palpation. Complete blood count demonstrated leukocytosis. Previous surgical history: appendectomy and transurethral prostatectomy for benign prostatic hyperplasia. The patient reported to be diabetic and smoker.
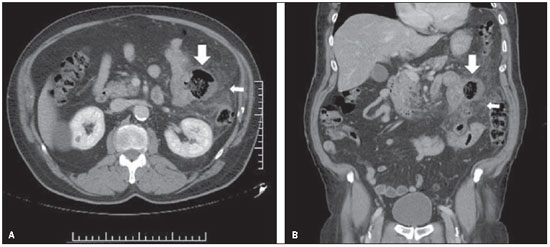
Whole abdomen CT scan was requested by the emergency medical team and was performed in 16-channel multidetector-row CT equipment in two phases: pre- and postintravenous contrast (venous phase at 90 seconds). The following tomographic findings were observed: parietal thickening of the proximal jejunal loop and saccular image with a gaseous content corresponding to jejunal diverticulum associated with extensive densification of the adjacent mesenteric fat (Figure 1).
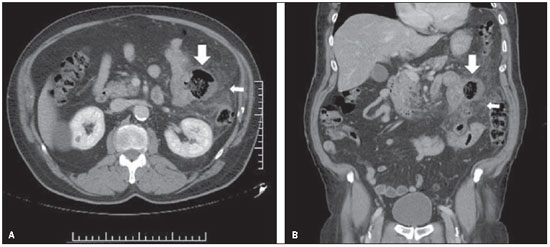
Figure 1. A: Contrast-enhanced axial CT image demonstrating a diverticulum at the mesenteric border of jejunal loop (downwards arrow) and extensive densification of the adjacent fat (leftwards arrow), signs of acute diverticulitis. B: Reconstruction of contrast-enhanced, coronal, whole abdomen CT image. Proximal jejunum diverticulum with signs of acute diverticulitis. Saccular image with gaseous content in the jejunal loop (downwards arrow) associated with extensive densification of the adjacent fat (leftwards arrow).
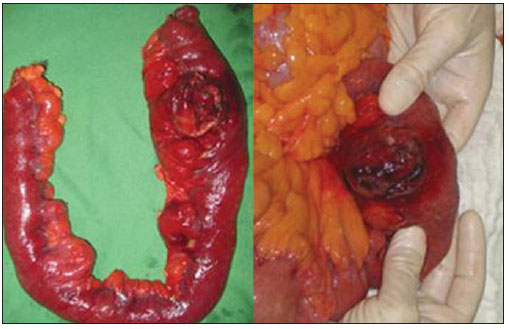
The patient was submitted to exploratory laparotomy for resection of the diverticulum and of the affected loop (Figure 2), that confirmed the diagnosis of jejunal diverticulitis.
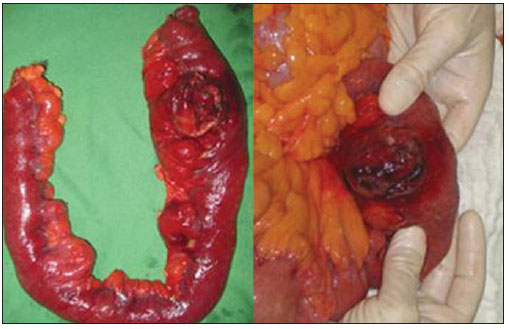
Figure 2. Images of surgical specimen: jejunal diverticulum complicated with diverticulitis, demonstrating inflammatory process and obstructed perforation.
Jejunal diverticula are constituted of a thin mucosal wall herniated through a muscular layer(4). They affect only the mucosal, submucosal and serous layers, hence the denomination pseudodiverticula, and occur adjacent to the mesenteric border(1,4). Its etiology still remains unclear, but it is known that changes in peristalsis, intraluminal pressure and intestinal dyskinesia are included in this entity pathogenesis. Jejunal diverticula tend to be larger, with a higher number of them occurring in the proximal jejunum, with its frequency progressively decreasing towards the distal jejunum, except for the terminal ileum region where multiple diverticula may be found(1–5). Association with colonic diverticular disease occurs in 35–75% of cases(5–9). Clinical symptoms and signs are vague and nonspecific and, considering the rarity of this condition, the diagnosis is always delayed and difficult to be achieved(1–5,9). In many cases, CT is essential for defining the diagnosis. Diverticulosis complications are rare, with incidence of 6–13%(4). Acute diverticulitis, pseudo-intestinal obstruction and chronic diverticulitis with development of diverticulum are the most frequent complications(6).
Tomographic findings of jejunal diverticulitis are similar to the ones of colonic diverticulitis: inflammatory mass containing gas and/or fecal residues, wall thickening in the affected segment (increased contrast uptake), with distension and edema of adjacent tissues (densification of the fascia and mesenteric fat)(4,6,7). In the present case, the imaging findings are compatible with the ones described in the literature and considered as typical signs of disease by many authors(5,7,10).
Among the possible complications of acute jejunal diverticulitis the most severe one is perforation followed by peritonitis, with a risk for mortality > 40%, and possible development of abscesses, bleeding, adhesions and fistulas(1,4,6).
Because of its rarity and the nonspecificity of symptoms, acute jejunal diverticulitis is rarely considered in the clinical differential diagnosis with other more prevalent conditions. In this context, CT becomes fundamental for determining its diagnosis, complications, and for ruling out other causes of acute abdomen.
REFERENCES
1. Peters R, Grust A, Gerharz CD, et al. Perforated jejunal diverticulitis as a rare cause of acute abdomen. Eur Radiol. 1999;9:1426–8.
2. Furtado E, Machado BFF. Divertículo intraluminal do duodeno: relato de caso. Radiol Bras. 2003;36:389–90.
3. Setubal R, Souza RP, Endo E, et al. Intussuscepção jejunojejunal em adulto – relato de um caso e revisão da literatura. Radiol Bras. 1996;29: 331–4.
4. Coulier B, Maldague P, Bourgeois A, et al. Diverticulitis of the small bowel: CT diagnosis. Abdom Imaging. 2007;32:228–33.
5. Graña L, Pedraja I, Mendez R, et al. Jejuno-ileal diverticulitis with localized perforation: CT and US findings. Eur J Radiol. 2009;71:318–23.
6. Spiegel RM, Schultz RW, Casarella WJ, et al. Massive hemorrhage from jejunal diverticula. Radiology. 1982;143:367–71.
7. Gliustra PE, Killoran PJ, Root JA, et al. Jejunal diverticulitis. Radiology. 1977;125:609–11.
8. Ramos AM, Piantá CD, Alves JM, et al. Diverticulite de intestino delgado em paciente idoso. Revista AMRIGS. 2005;49:41–3.
9. Nacif MS, Rocha VMB, Mello RAF, et al. Análise retrospectiva do trânsito do delgado em um serviço de radiologia de hospital geral. Radiol Bras. 2004;37:179–83.
10. Veen M, Hornstra BJ, Clemens CHM, et al. Small bowel diverticulitis as a cause of acute abdomen. Eur J Gastroenterol Hepatol. 2009;21:123–5.
1. MDs, Trainees in Radiology at Centro Radiológico Campinas – Hospital Vera Cruz, Campinas, SP, Brazil.
2. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist at Centro Radiológico Campinas – Hospital Vera Cruz, Physician Assistant, Department of Radiology, Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil.
3. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Head of the Department of Radiology, Centro Radiológico Campinas – Hospital Vera Cruz, Campinas, SP, Brazil.
Mailing Address:
Dra. Beatriz Lavras Costallat
Rua Ezequiel Magalhães, 26, Jardim das Paineiras
Campinas, SP, Brazil, 13092-522
E-mail: biacostallat@hotmail.com
Received June 20, 2010.
Accepted after revision November 19, 2010.
Study developed at Centro Radiológico Campinas – Hospital Vera Cruz, Campinas, SP, Brazil.
 Vol. 44 nº 2 - Mar. / Apr. of 2011
Vol. 44 nº 2 - Mar. / Apr. of 2011