INTRODUCTION
Radiotherapy is an important oncologic treatment technique(1). In such a treatment modality, ionizing radiation is directly applied to the tumor in order to at least retard its growth. Approximately 50% of all cancer patients will be submitted to radiotherapy, which may be used as a single treatment or in association with other treatment modalities.
The Monte Carlo method is applied to reproduce a statistical process similar to the interaction of nuclear particles with human tissues. Such a technique is of particular interest in solving complex problems that cannot be modeled by deterministic computational methods. In the transport of nuclear particles, the Monte Carlo technique follows up each one of the many primary or secondary particles generated by a radioactive source, during its lifetime up to its total withdrawal at any terminal event such as: absorption, scattering, escape from the system, among others(2). The three-dimensional simulation of nuclear particles transport plays a relevant role in the improvement of quality in radiotherapy procedures( 3). Such type of computational planning was created with the purpose of eliminating the deficiencies of the 2D planning( 4). Kijewski et al.(5) have demonstrated that the models applied in such simulations must be personalized in order to obtain an effective treatment protocol, generating an absorbed dose sufficient to achieve control of the tumor growth while minimizing the dose at healthy adjacent tissues.
The present study describes a technique for conversion of computed tomography (CT) or magnetic resonance (MRI) images into three-dimensional voxel model for dosimetry purposes. Voxels are the equivalent to pixels (image elements) in a three-dimensional space. Such model may be a personalized representation of the patient, which is applied to the simulation of the particle transport phenomenon, for example by means of the MCNP (Monte Carlo N-Particle) code. The SISCODES (a computational system for neutron/photons dosimetry based on stochastic methods) is utilized in the implementation of such voxel model generation technique and performs dosimetric calculations. The system was developed for Linux in C++, PHP, Python and SQL, and has had its registration filed at Instituto Nacional de Propriedade Intelectual (INPI) (National Intellectual Property Institute) by the Committee for Innovation and Technology Transfer (Comissão de Inovação e Transferência Tecnológica – CITT) of Universidade Federal de Minas Gerais (UFMG). Such system has been utilized by the Núcleo de Radiações Ionizantes/Conselho Nacional de Desenvolvimento Científico e Tecnológico (NRI/CNPq)(6) (Center of Ionizing Radiations/National Council for Scientific and Technological Development) for the development of anthropomorphic and anthropometric voxel models that can be inserted into the MCNP code for the modeling of brachytherapy and teletherapy applied to lung, pelvis, spine, head and neck tumors, among others(7,8). The SISCODES provides a fast method to create personalized voxel models of any patient. The already developed SISCODES modules are shown with examples of cases of radiotherapy planning.
MATERIALS AND METHODS
The computational system known as SISCODES is a tool for three dimensional computational planning of radiotherapy or radiological procedures, providing friendly interfaces that allow health professionals to operate the system. Based on tomographic images of the patient, the treatment plan is modeled and simulated. Then, the SISCODES shows the absorbed doses by means of isodose curves superimposed on the model.
The SISCODES couples the 3D model with the MCNP5 code, simulating the protocol of exposure to ionizing radiation. The system presents a client/server architecture, running in three distinct environments: the workstation; the Internet; and the server. The server may be a supercomputer or a cluster of microcomputers, and is utilized for the stochastic calculations, management and storage of the nuclear data in the databank. Internet allows the server to be accessed from workstations virtually anywhere in the world. And the client/server architecture allows the required hardware to be shared amongst various research groups, thus sharing the costs and making the system even more accessible.
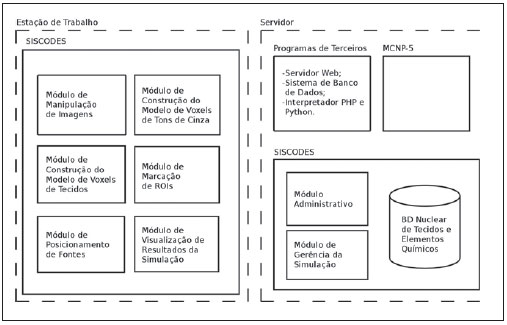
The SISCODES is developed in modules or sub-systems, with each module running independently and has been in use for research in radiotherapy planning since 2003.The system architecture is shown on Figure 1.
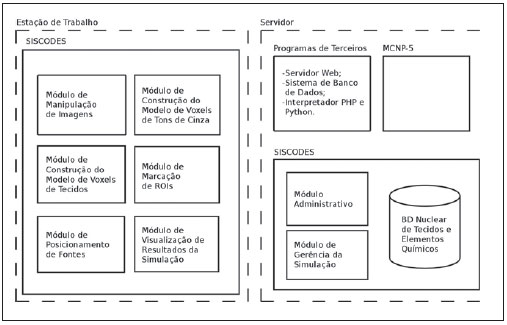
Figure 1. Simplified SISCODES architecture showing the modules that are executed in the server and those that are executed directly at the workstations.
Two different methods are utilized to develop the patient model to be utilized in simulations. Firstly, an analytical phantom with the patient’s biometry must be generated by a computational code coupled with SISCODES. Such code utilizes anatomical measurements of the patient to develop a standard phantom, in such a way that it matches the patient’s biometry(9). A SISCODES interface assists the user in the process of selecting and entering the patient’s data. The generated analytical model is an anatomical representation of the whole patient’s body. A three-dimensional voxel model is generated for the region of interest. Such model is a 3D matrix, in which each element represents a tissue equivalent to the corresponding biological tissue. Such model faithfully resembles the patient’s anatomy in the region of interest. The construction of the patient’s voxel model is done in four steps:
1. Digitization of tomographic images: DICOM CT or MRI images are selected or if necessary digitized from radiological images.
2. Images treatment: the selected images are processed and cut down to be limited to the region of interest. The SISCODES module called “Trata Imagem” (image processing) is utilized in this step.
3. Conversion of the patient’s images selection into a three dimensional matrix based on grayscale images: a voxel model based on the grayscale images of the patient is automatically generated. The SISCODES module called “Gera Modelo de Cinza” (gray model generator) performs this task, in which each element in the matrix is attributed a value between 0 and 255 based on the image grayscale.
4. Conversion of the grayscale model into a voxel model based on tissues: the SISCODES module called “Gera Modelo de Tecidos” (tissue model generator) allows the user to perform the conversion of the model obtained from step 3 (grayscale voxel model) into a tissue voxel model, in which each voxel stores the information on the patient’s tissue.
The SISCODES implements and supports a databank comprising nuclear data on tissues, which runs independently from the generation of the voxel model, even though it is utilized for such generation. The SISCODES module called “Administrativo” (administrative module) allows the management of the data from each tissue, such as color of the representation, elementary chemical composition, photons and neutrons kerma, the value of relative biological effectiveness (RBE), and other weighting factors, as well as a of a link to the nuclear library of photons and neutrons – Evaluated Nuclear Data File Bank-Edition 7 (ENDFB-7), utilized at the MCNP.
The SISCODES´ module called “Gera ROIs” (ROIs generator) allows the selection of the voxels in which required information (fluence, dose or dose rate) is of interest for the simulation. Such module also allows the conversion of the files according to the SISCODES standard into the file format required for entering the MCNP. The voxels model and the analytical phantom must be coupled to allowing the MCNP to complete the simulation. Once the simulation is completed, the user executes the SISCODES module “Gera Saída” (output generator). Such module converts the neutron or photon fluence into dose by multiplying the kerma
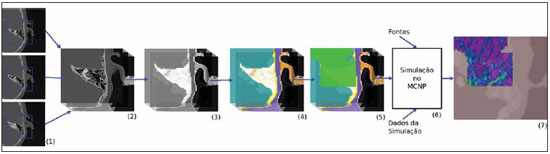
versus fluence coefficients and shows isodose curves plotted over the patient’s voxel model. A summary of the process for the simulation of a radiotherapy planning is shown on Figure 2.
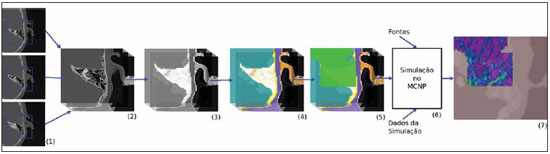
Figure 2. Simplified process of the voxel model construction and simulation of the radiotherapy treatment at SISCODES: tomographic images are digitized (1), converted into a layered model (2), converted into a grayscale voxel model (3) and into tissue voxel model (4). The ROIs are marked on the model (5). This model is combined with the parametric phantom and with the information from the radioactive sources. The resulting file is simulated at MCNP (6). After the simulation is completed, the user can visualize the isodoses curves with the spatial distribution of the absorbed dose (7).
Image processing module – On this module the user uploads the patient’s tomographic images (CT or MRI) and, by manipulating such images, builds a layered model that is actually a collection of the set of images whose resolution has been standardized. The images must be obtained with a suitable resolution which allows the development of the image faithfully reproducing the tomography and preserving the visibility to the user. The image resolution may be around 100 or 200 DPI (dots per inch).
Grayscale voxel model generator module – In this module the user uploads the previous layered model. The user also defines the size of each voxel, the number of planes in the voxel model and, by adjusting, the images placed on the layered model and the grasped area on the image corresponding to the model, builds a grayscale voxel model.
The layered model images may have been digitized either in colors or in grayscale. When a color image is utilized, the grayscale stored in a voxel will be the arithmetic mean of the color channels (RGB- red, green, blue) of the pixels chosen to represent that voxel. Studies have been undertaken in an attempt to identify the algorithm that best represents a given voxel. However, as the grayscale model is used only as a reference for the construction of the tissues model, one opted to utilize the grayscale of the central pixel of the area on the image that represents the voxel, thus making the algorithm of choice computationally efficient.
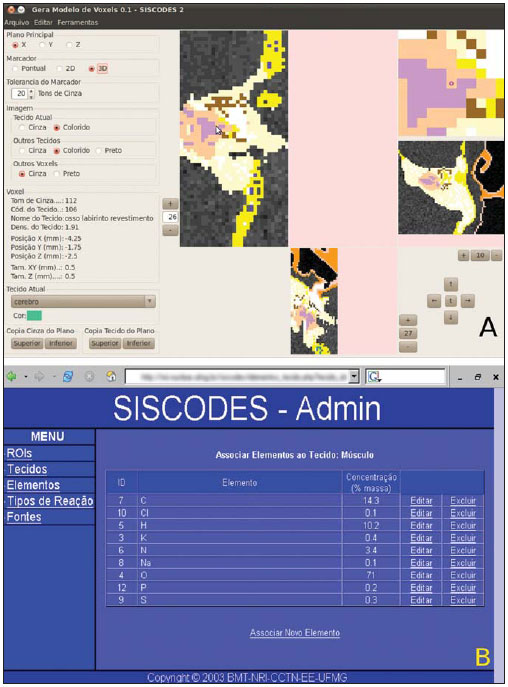
Tissue voxel model generator module – The interface that generates the voxel model based on tissues is shown on Figure 3A. The user uploads the grayscale model from the gray scale voxel model generator module and by means of a coloring tool changes the color in each individual voxel or in groups of voxels, that may be selected individually or in both 2D and 3D groups. The group selection is based on the similarity of gray tones, whose variation tolerance may be adjusted. The user helps in this process by associating a tissue from the databank to each voxel of the model, identifying the organs and tissues of interest.
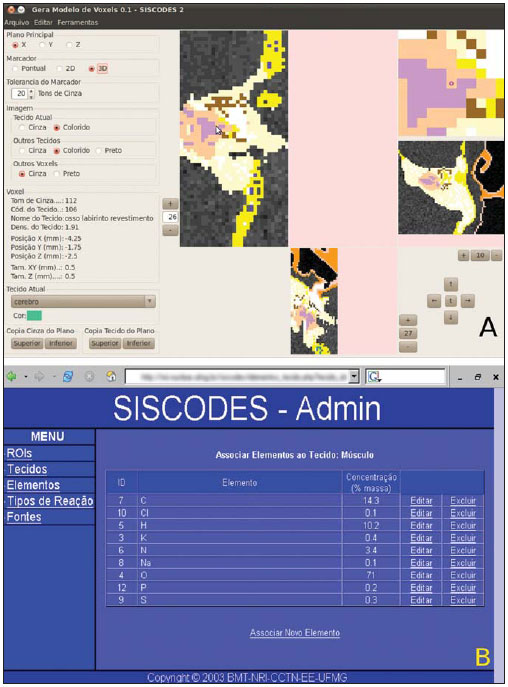
Figure 3. A: Interface of the tissue voxel model generating module showing the construction of the voxel model of the ear region. B: Web interface of the administrative module showing the page where it is possible to edit the chemical composition of tissues and materials.
The same procedure can be utilized in previously built models, in order to make changes in parts of such models.
The tissues are previously entered into the SISCODES databank by using the administrative module. The voxel filled with a tissue receives the color associated with that particular tissue, allowing the user to easily differentiate the voxels that have already been associated with a tissue from those that are yet to receive one.
ROIs generator module – Such module runs similarly to the previous one, however the user selects on which voxels the neutrons or photons fluence will be evaluated. Such step is critical, as in case the fluence is evaluated in all voxels of the model, the time required for the simulation of the radiotherapy planning will be unacceptable. Up to the present moment, by utilizing this module, the user can generate fragments of the MCNP input files, which represent the voxel model, the chemical composition of the tissues, the utilized libraries and the output requests. Such files must be concatenated together with the analytical model, the sources and what is executed at MCNP. After execution, SISCODES can process the generated output.
Management module – Such module, shown on Figure 3B, was written in PHP language (PHP Html Preprocessor) and must be accessed by means of an Internet browser. The administrator user can include tissues in the SISCODES databank, along with their chemical composition and mass density. The administrator user may also include individual chemical elements in the SISCODES databank. Each chemical element has its kerma conversion coefficients for neutrons and photons filed for a wide spectrum of energy (0.0025 eV to 20 MeV). RBE coefficients for specific nuclear reactions may also be filed. Such module makes the interpolation of kerma coefficients for each chemical element, dividing the spectrum at small and regular intervals. For this purpose, the equation below is applied. By utilizing the kerma coefficients of the chemical elements and the elementary composition by weight of the tissues, such module calculates the kerma of each filed tissue or organ, by considering the kerma coefficient of the element weighted by percentage of mass of such element in the tissue. In order to make the dose calculation easier, only the fluence is evaluated in the MCNP simulation; thus the effect of dose-enhancing agents can be quickly calculated according to the type of particles or type of tissue radiosensitivity and the application of RBE coefficients on the applied dose.
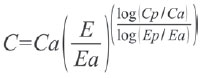
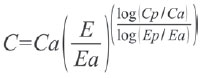
Such equation is utilized in the interpolation of kerma coefficients, where: C – kerma coefficient to be calculated; Ca – previous kerma coefficient: the known coefficient with the highest energy, immediately inferior to the one to be calculated; Cp – later kerma coefficient: the known coefficient with the lowest energy immediately subsequent to the one to be calculated; E – energy of the kerma coefficient to be calculated; Ea – energy of the previous kerma coefficient; Ep – energy of the later kerma coefficient.
SISCODES also allows the register of radioactive brachytherapy or teletherapy sources. The radioactive spectrum of radionuclides or from
Bremsstrahlung interactions can be included in the SISCODES databank, with the possibility of being associated with an external or an internal source.
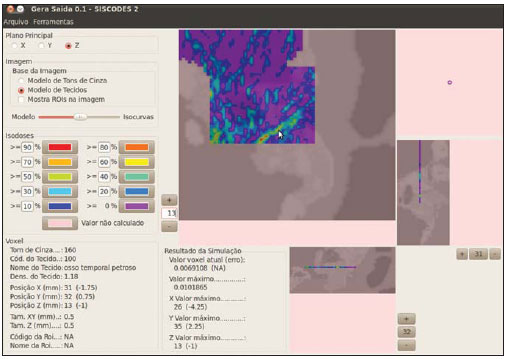
Output visualization module – This module that is shown on Figure 4 reads the MCNP output file, the tissue voxel model and the files with the ROIs; and shows the isodose curves superimposed over the voxels model. The fluence in each voxel obtained from the MCNP simulation, and the kerma coefficients are utilized in the calculation of the absorbed dose (see item 3). In order to allow a good visualization of the isodoses on the voxel model, it is magnified by means of a bicubic interpolation and the isodoses are calculated on this new model by means of an isotropic interpolation. The user can control the transparency level of the isodoses representation, selecting the one that provides the best visualization.
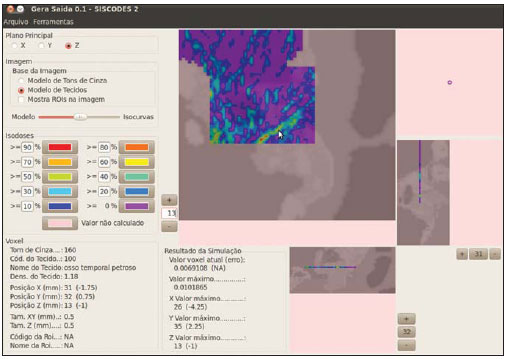
Figure 4. Interface of the output visualization module, showing the obtained curves as a result of simulation on the model of the ear region. Such module reads the voxel model and the output from MCNP and draws the isodoses curves over the patient’s images reconstruction.
Sources positioning module – This module allows the user, by means of a graphic interface, to select and position the radioactive sources utilized in the simulation. In this interface, both the brachytherapy and teletherapy sources are positioned. The position is given by an arbitrary point on the model (defined by values on the X, Y and Z axes) and by an also arbitrary orientation (defined by alpha – XY and beta – XZ angles). For teletherapy sources, the distance between the source and the reference point as well as the window dimensions must also be informed.
Simulation management module – This model allows the user to assemble a complete MCNP input file and to manage the simulation execution. The user selects the files required for the simulation, creating a group of files. Subsequently, the module assembles the MCNP input file, sends such file for running and receives the results after its execution.
3. Calculation of doses at SISCODES
SISCODES runs as an interface for the MCNP code. MCNP is a nuclear code based on stochastic processes, in which the trajectory of each generated radioactive particle is tracked, forecasting the interaction of such particles with matter. The history of each particle is then memorized. At SISCODES, the voxel model is converted into a MCNP input file, which then simulates the interaction of nuclear particles with the chemical elements that are present in the tissues associated to each voxel.
The MCNP returns to SISCODES the number of incident particles per area unit for each voxel (fluence), normalized by the number of particles emitted by the source. The fluence generated at the MCNP simulation is transformed into absorbed dose that is multiplied by the appropriate fluence-kerma conversion coefficients, by the source upwelling (number of particles emitted by time unit) and by the exposure time. Thus, SISCODES can calculate the absorbed dose in each voxel and, if necessary, apply to such dose the RBE coefficients, obtaining a biologically weighted dose. The RBE is defined for each tissue and each nuclear reaction, and is recorded at the SISCODES databank by means of the administrative module.
The MCNP can directly calculate the absorbed dose or dose rate and transfer such values to the SISCODES. However, the SISCODES operates with the fluence and converts it into absorbed dose or biologically weighted dose, according to the user’s interest. This is due to the fact that radioprotectors or radio-potentiators can affect the absorbed dose, but do not affect the fluence. Boron neutron capture therapy (BNCT) may be mentioned as an example of evaluation that involves the need for potentiators. By applying a fluence-dose conversion process, the system can quickly calculate the impact of the utilization of such protectors/potentiators, as the MCNP is run only once.
RESULTS
The SISCODES has been in use by the NRI research group at the Nuclear Engineering Department of UFMG (DEN/ UFMG) for the construction of several voxels models representing anatomic regions of human beings and of small animals. Some of these models have been applied in the simulation of brachytherapy or teletherapy procedures. In this section, some of these models are described and some simulations results are reported.
Human female thorax
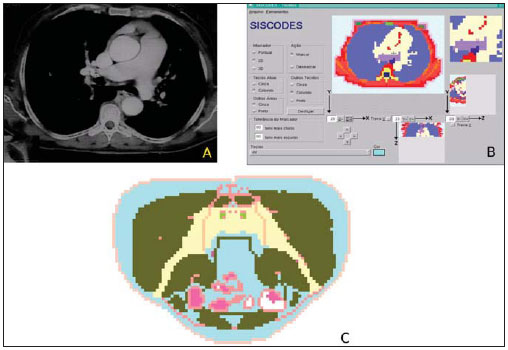
This model was constructed at NRI and is shown on Figures 5A and 5B(10). It was developed side by side with an actual anthropometric and anthropomorphic phantom in order to investigate treatments for breast, esophagus and lung cancers. Such phantom can be very useful in the evaluation of the SISCODES accuracy by means of the comparison between absorbed doses evaluated in experiments with the actual phantom and those obtained through computational simulation.
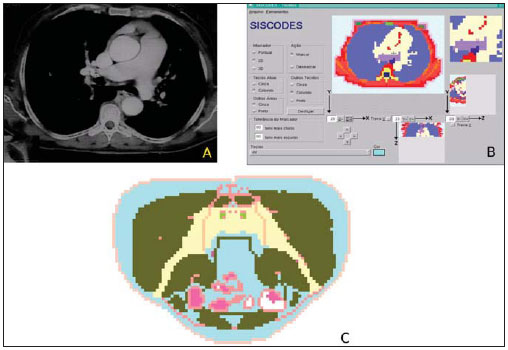
Figure 5. Creation of the thorax voxel model. A: Digitized CT image of the thorax. B: older interface version of the tissue voxel model of SISCODES, showing the model at the same plane of the image. C: Voxel model of a male pelvis.
Breast cancer is particularly difficult to irradiate because of its proximity with the lungs, which are very radio-sensitive. Such model may be useful in the development of better protocols for breast cancer radiotherapy, allowing the selection of those that produce lower doses to the lungs and higher doses to the tumor.
Human male pelvis
This model was developed at SISCODES in order to allow studies about prostate cancer(7). As in the case of the female thorax model, this model has its actual equivalent, allowing its use in the evaluation of the SISCODES accuracy. The voxels model was developed from images of the Visible Human Project(11), which were also the basis for the actual phantom built from tissue-equivalent material. Prostate cancer is one of the most common cancers in men. Such model may be utilized in the simulation of teletherapy and radiotherapy protocols. A section of this model is shown on Figure 5C.
Human ear
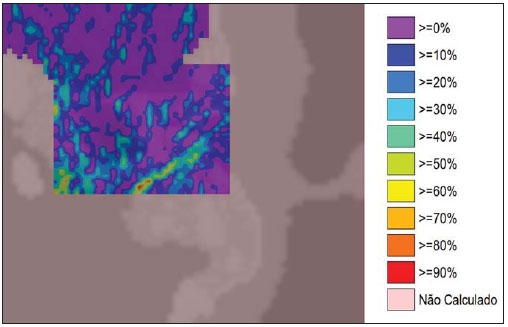
This model represents the human ear region, as shown on Figure 6. It was developed in a master’s research project with the purpose of studying side-effects after head and neck teletherapy(12). The knowledge of actual absorbed dose is relevant because of two factors: a) to know what dose level causes side-effects in the ears; b) to assist in the choice of the best protocol for each irradiation window, avoiding exposure of the ear. Two treatment protocols were simulated, and presented great heterogeneity of dose in the petrous bone, that may be associated with the tissue heterogeneity and with photon scattering. The observed dose heterogeneity cannot be modeled in the water phantoms utilized in radiotherapy centers for calibration of isodoses curves. The application of homogeneous methods for dose calculation may result in either over- or under estimation of the dose in the ear structure.
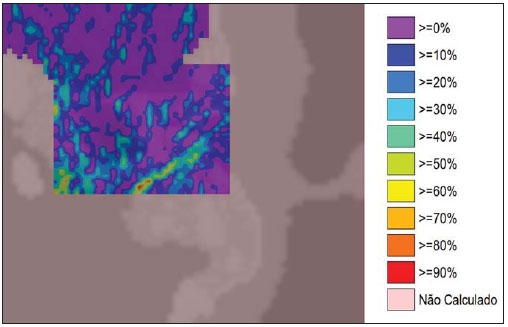
Figure 6. Isodoses curves of the ear region, with the respective scale. The shown doses are absorbed due to a protocol of ear irradiation. Notice the wide heterogeneity of the dose as compared with the evenly distributed doses in a water phantom.
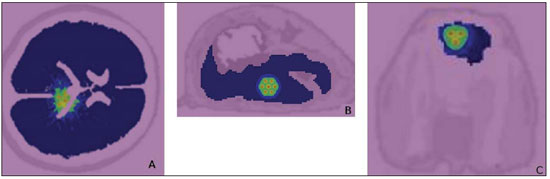
This model was built for the study of brachytherapy implants of I-125 seeds or bioactive glass seeds with Sm-153 or Ho- 166 (this type of implant may be an alternative to I-125 implants)(13,14). The isodose curves shown on Figure 7A represent the doses produced by gamma rays emitted by Sm-153 implanted seeds.
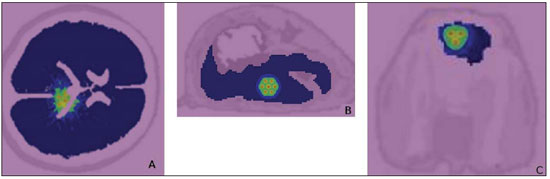
Figure 7. A: Isodoses curves obtained from the simulation of bioglass seeds with Sm-153 implants in a child’s brain. B: Isodoses curves generated by ceramic
seeds implants in a rabbit liver. C: Isodose curves generated by bioglass seeds implants in a rabbit brain.
Models of parts of small animals, such as rabbit brain and abdomen were developed at NRI(15,16). Such models allow experimental and computational dosimetry in studies with small animals. In this case, the computational model is useful to reduce the number of animals utilized in experiments. The dosimetric evaluation in this case was aimed at estimating the spatial distribution of beta and gamma particles energies, produced by brachytherapy sources (radioactive ceramic seeds). For such a study, a voxel model of the thorax and abdomen of a rabbit was developed and simulations of radioactive implants were performed. The respective isodoses curves are shown on Figure 7B.
Rabbit brain
A voxel model of a rabbit head was built by Costa in order to study bioglass implants in the brain(17). The implants comprise 15 Ca-Si bioglass seeds with Sm-153(18–21). A voxel model was built at SISCODES based on CT images of the animal. In this study, the simulation demonstrates the spatial distribution of dose rate in the rabbit brain as a consequence of the bioglass Sm-153 implants. The respective isodoses curves are shown on Figure 7C.
DISCUSSION
The presented computational system has been in use by the NRI research group in the development of computational anthropomorphic and anthropometric phantoms based on voxel models and in the simulation of radiotherapy treatments. The system is being applied in the study of nuclear particles transport in the treatment of breast, lung, uterine cervix, prostate, spine, and head and neck cancers, among others.
The graphic interface provided by SISCODES allows the utilization of the MCNP by professionals that otherwise would not be able to use such code, considering the complexity of its input file syntax and the output visualization module capability to extract the results from the simulation and to represent such results on images.
The developed models and data stored in the databank, together with SISCODES, comprise the basis for radiotherapy simulations. Such basis allows the development of studies on radiotherapy treatment with efficiency in terms of research swiftness, which is much higher than one can achieve without its use, and with the dosimetric accuracy achieved by the utilization of the MCNP.
The treatment simulation results demonstrate that the absorbed dose presents a great spatial heterogeneity in regions of the body presenting great variations in mass or density, such as bones, air cavities and lowdensity tissues such as inflated lungs, possibly diverging from the values obtained in homogeneous water phantoms and even from dose values found by complex analytical methods. Such dose heterogeneity can only be obtained by simulations utilizing the MCNP, as the analytical methods are not capable of correctly dealing with variations found in human tissues, particularly in interface regions(22,23).
CONCLUSIONS
The system allows the construction of personalized voxel model of a patient in a relatively short time, making the radiotherapy planning more accurate whenever stochastic codes such as MCNP are utilized. The biometric representation of the patient together with the irradiation region faithfully represented by the voxel model makes the simulation more specific and personalized. The combination of MCNP simulation with a personalized patient’s model provides great improvements in dosimetry of radiotherapy treatments, contributing to the increase in treatment effectiveness with reduction in the morbidity rates. The authors expect this study to be a contribution to the enhancement and improvement of dosimetric evaluation procedures present in radiotherapy and radiology.
Acknowledgements
The authors wish to express their gratitude to the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Capes) and to Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), by the support and assistance to research at Ionizing Radiations Center of Universidade Federal de Minas Gerais (NRI-UFMG).
REFERENCES
1. Emami B. Oral cavity. In: Perez CA, Brady L, editors. Principles and practice of radiation oncology. 3rd ed. Philadelphia, PA: Lippincott- Raven; 1998. p. 981–1002.
2. MCNP – X-5 Monte Carlo Team. A general Monte Carlo N-particle transport code manual, version 5. Los Alamos, NM: Los Alamos National Laboratory, 2003.
3. Purdy JA. Three-dimensional physics and treatment planning. In: Perez CA, Brady LW, editors. Principles and practice of radiation oncology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 1998. p. 343–70.
4. Emami B, Graham MV, Michalski JM, et al. Three-dimensional conformal radiation therapy: clinical aspects. In: Perez CA, Brady LW, editors. Principles and practice of radiation oncology. 3rd ed. Philadelphia, PA: Lippincott-Raven; 1998. p. 371–86.
5. Kijewski P. Three-dimensional treatment planning. In: Mauch PM, Loeffler JS, editors. Radiation oncology: technology and biology. Philadelphia, PA: Saunders; 1994. p. 10–33.
6. NRI – Núcleo de Radiações Ionizantes. Página inicial. [acessado em 1º de fevereiro de 2011]. Disponível em: http://nri.nuclear.ufmg.br
7. Silva CHT, Campos TPR. Fantoma computacional de voxel, associado a fantoma real antropomórfico antropométrico, para dosimetria. In: International Nuclear Atlantic Conference; 2000; Rio de Janeiro, RJ, Brasil. ABEN – Associação Brasileira de Energia Nuclear. Anais. 2000. p. 1– 7.
8. Silveira MF, Campos TPR. Implantação de compostos radioativos para controle de tumores ósseos nos membros. In: 4º Congresso Latino-Americano de Órgãos Artificiais e Biomateriais; 2006; Caxambu, MG, Brasil. Anais. 2006. p. 1–7.
9. Mata PHC, Trindade BM, Campos TPR. Fantoma parametrizado com órgãos em voxels inseridos para oncologia. In: 3º Congresso Latino Americano de Órgãos Artificiais e Biomateriais; 2004; Campinas, SP, Brasil. Anais. 2006. p. 1–6.
10. Maia M. Fantoma antropomórfico antropométrico de tórax para fins de radioproteção e dosimetria [dissertação]. Belo Horizonte, MG: Universidade Federal de Minas Gerais; 2004.
11. VHP. The Visible Human Project Overview. [acessado em 14 de setembro de 2010]. Disponível em: http://www.nlm.nih.gov/research/visible/ visible_human.html
12. Trindade DFM. Efeitos deletérios induzidos por exposição indireta do aparelho auditivo durante radioterapia de cabeça e pescoço – correlacionamento dosimétrico [dissertação]. Belo Horizonte, MG: Universidade Federal de Minas Gerais; 2006.
13. Duarte IL, Campos TPR. Avaliação dosimétrica clínica de Implantes de biovidros incorporando Sm-153 para tratamento de tumores cerebrais. In: 4º Congresso Latino Americano de Órgãos Artificiais e Biomateriais; 2006; Caxambu, MG, Brasil. Anais. 2006. p. 1–6.
14. Thompson L, Campos TPR. Fantoma real de cabeça e pescoço desenvolvido para avaliações radiodosimétricas. In: 4º Congresso Latino Americano de Órgãos Artificiais e Biomateriais; 2006; Caxambu, MG, Brasil. Anais. 2006. p. 1–8.
15. Andrade JPL, Campos TPR. Avaliação da energia específica absorvida gerada de biovidros radioativos implantados em fígado em modelo animal. In: 4º Congresso Latino Americano de Órgãos Artificiais e Biomateriais; 2006; Caxambu, MG, Brasil. Anais. 2006. p. 1–10.
16. Campos TPR, Andrade JPL, Costa IT, et al. Estudo preliminar da degradação de sementes de Sm-153 aplicadas e implantes de fígado de coelho. In: 4º Congresso Latino Americano de Órgãos Artificiais e Biomateriais; 2006; Caxambu, MG, Brasil. Anais. 2006. p. 1–6.
17. Costa IT, Campos TPR. Resposta radiodosimétrica de implantes de sementes de biovidros radioativos no cérebro de coelhos. In: 4º Congresso Latino Americano de Órgãos Artificiais e Biomateriais; 2006; Caxambu, MG, Brasil. Anais. 2006. p. 1–7.
18. Mendes BM, Campos TPR. Investigation of the specific energy deposition form radionuclidehydroxyapatite macroaggregate in brain interstitial implants. Key Engineering Materials. 2004; 254:83–6.
19. Mendes BM, Campos TPR. Ecogenic response and dosimetric evaluation of hydroxyapatite macroaggregates implants. In: COBEM 2005 – 18th International Congress of Mechanical Engineering; 2005; Rio de Janeiro, RJ, Brasil. Anais. 2005. p. 1–8.
20. Roberto WS, Pereira MM, Campos TPR. Analysis of bioactive glasses obtained by sol-gel processing for radioactive implants. Materials Research. 2003;6:123–7.
21. Roberto WS, Pereira MM, Campos TPR. Structure and dosimetric analysis of biodegradable glasses for prostate cancer treatment. Artif Organs. 2003;27:432–6.
22. Van Esch A, Tillikainen L, Pyykkonen J, et al. Testing of the analytical anisotropic algorithm for photon dose calculation. Med Phys. 2006;33: 4130–48.
23. Carrasco P, Jornet N, Duch MA, et al. Comparison of dose calculation algorithms in slab phantoms with cortical bone equivalent heterogeneities. Med Phys. 2007;34:3323–33.
1. Master, Fellow PhD degree of Sciences and Nuclear Techniques – Program of Post-Graduation in Sciences and Nuclear Techniques, Universidade Federal de Minas Gerais (UFMG), Professor at Centro Universitário Una, Belo Horizonte, MG, Brazil.
2. PhD of Nuclear Engineering, Associate Professor III, Course of Post-Graduation in Sciences and Nuclear Techniques, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil.
Mailing Address:
Dr. Tarcisio Passos Ribeiro de Campos
Avenida Antonio Carlos, 6627, prédio PCA1, sala 2285, Campus Pampulha
Belo Horizonte, MG, Brazil, 31270-901
E-mail: campos@nuclear.ufmg.br
Received September 29, 2010.
Accepted after revision February 17, 2011.
Study developed at the Engineering School of Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil.
 Vol. 44 nº 2 - Mar. / Apr. of 2011
Vol. 44 nº 2 - Mar. / Apr. of 2011