Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 1 - Jan. /Feb. of 2011
Vol. 44 nº 1 - Jan. /Feb. of 2011
|
WHICH IS YOUR DIAGNOSIS?
|
|
WHICH IS YOUR DIAGNOSIS? |
|
|
Autho(rs): Roberto Paulo Rabelo Barcelos1; Pedro Paulo Teixeira e Silva Torres2; Pedro José de Santana Júnior1; Maria Auxiliadora Carmo Moreira3; Marcelo Eustáquio Montandon Júnior2; Kim-Ir-Sen Santos Teixeira4 |
|
|
Male, 67-year-old patient complaining of progressive dyspnea and cough for five years. At clinical examination the patient presented bibasilar velcro-like crepitation. Chest radiography (Figure 1) and highresolution computed tomography (HRCT) (Figure 2) were performed. Two months after the diagnosis and initiation of treatment, the patient complained of a considerable accentuation of the dyspnea over the last 15 days, presenting a significant worsening of the imaging pattern at HRCT (Figure 3).
 Figure 1. Chest radiography - anteroposterior view. 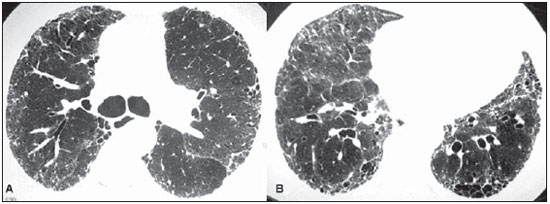 Figure 2. Axial HRCT images at the level of the carina (A) and pulmonary bases (B). Initial study. 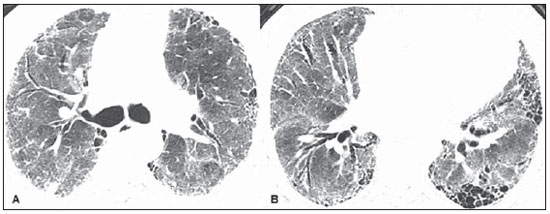 Figure 3. Axial HRCT images at the level of the carina (A) and lung bases (B). Follow-up study performed two months later. Images description Figure 1. Chest radiography - anteroposterior view demonstrating predominantly basilar and peripheral gross reticular opacities. Figure 2. Axial HRCT images at the level of the carina (A) and lung bases (B). Initial study characterizing subpleural, intralobular interstitial thickening, traction bronchiectasis and honeycombing. Figure 3. Axial HRCT images at the level of the carina (A) and lung bases (B). Follow-up study performed two months later, after subacute worsening of the symptoms, demonstrating the same previous findings added of a superimposed pattern of diffuse ground-glass attenuation. Diagnosis: Acute exacerbation of idiopathic pulmonary fibrosis. COMMENTS The natural progression of idiopathic pulmonary fibrosis is well characterized, with a foreseeable, gradual respiratory function decline over time. On the other hand, some patients present a severe clinical course, with acute worsening of the respiratory function status, without a defined etiology, denominated "acute exacerbations of idiopathic pulmonary fibrosis"(1). In spite of the actual incidence of acute exacerbations of idiopathic pulmonary fibrosis is still to be known, such abnormality has been recognized as common events, causing significant mortality of up to 78% in some series(1,2). Histopathological findings in patients submitted to lung biopsy disclose diffuse alveolar damage superimposed on underlying usual interstitial pneumonia and, in some cases, association with the pattern of organizing pneumonia(3). No consensus has been achieved on the diagnostic approach of acute exacerbation, but the diagnostic criteria proposed by a study published by the American Thoracic Society include: 1) diagnosis of idiopathic pulmonary fibrosis; 2) worsening of the clinical pattern with no defined cause within 30 days; 3) "new" ground-glass opacity pattern superimposed on the pattern of usual interstitial pneumonia observed at HRCT; 4) absence of infection documented by endotracheal tube aspirate or bronchoalveolar lavage; 5) exclusion of other causes of decompensation such as left ventricular failure, pulmonary embolism or other causes of diffuse alveolar damage(1). High-resolution computed tomography is an essential tool in the diagnosis of both usual interstitial pneumonia and acute exacerbation and, in this group of patients, demonstrates an increase in pulmonary opacity, with the patterns of ground-glass attenuation and/or bilateral consolidations superimposed on the pattern of usual interstitial pneumonia. The distribution of HRCT findings in patients with acute exacerbation has been related to the prognosis, and the diffuse, multifocal and peripheral patterns are described, the first two ones being associated with a worse disease progression and histologically linked to diffuse alveolar damage(1-5). The authors present the case of a patient with diagnosis of idiopathic pulmonary fibrosis, with a rapid worsening of his respiratory pattern characterized by hypoxemia with a decrease > 10 mmHg in PaO2 (from 71 to 58). After his clinical worsening, the patient was submitted to HRCT that demonstrated diffuse ground-glass attenuation superimposed on the pattern of usual interstitial pneumonia. The hypothesis of cardiovascular decompensation was ruled out by clinical examination and imaging findings and chest angio-CT was negative for pulmonary thromboembolism. Some evidences demonstrated the improbability of an infectious cause: early in the respiratory decompensation, wide-ranging antibiotic therapy did not lead to any clinical or radiological improvement, the tomographic findings did not suggest any association with infectious process and, during intensive care unit stay, endotracheal tube aspiration was performed and the culture was negative for both bacterial agents and fungi. Because of the severe status of respiratory failure, lung biopsy could not be performed, but the patient met all the five proposed criteria(1) for the noninvasive diagnosis of acute exacerbation of idiopathic pulmonary fibrosis, hence the presumptive diagnosis of this entity. REFERENCES 1. Collard HR, Moore BB, Flaherty KR, et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176:636-43. 2. Akira M, Kozuka T, Yamamoto S, et al. Computed tomography findings in acute exacerbation of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2008;178:372-8. 3. Hyzy R, Huang S, Myers J, et al. Acute exacerbation of idiopathic pulmonary fibrosis. Chest. 2007;132;1652-8. 4. Akira M, Hamada H, Sakatani M, et al. CT findings during phase of accelerated deterioration in patients with idiopathic pulmonary fibrosis. AJR Am J Roentgenol. 1997;168:79-83. 5. Souza CA, Müller NL, Flint J, et al. Idiopathic pulmonary fibrosis: spectrum of high-resolution CT findings. AJR Am J Roentgenol. 2005;185: 1531-9. 1. MDs, Residents at Hospital das Clínicas da Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. 2. MDs, Radiologists, Clínica Multimagem Diagnósticos, Goiânia, GO, Brazil. 3. Master, Associate Professor, Faculdade de Medicina da Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. 4. PhD, Associate Professor and Coordinator for the Program of Residency in Radiology, Hospital das Clínicas da Universidade Federal de Goiás (UFG), Goiânia. GO, Brazil. Mailing Address: Dr. Roberto Paulo Rabelo Barcelos Universidade Federal de Goiás Departamento de Radiologia e Diagnóstico por Imagem Avenida Primeira Avenida, s/nº, Setor Leste Universitário Goiânia, GO, Brazil, 74605-020 E-mail: robertoprb@gmail.com Study developed at Department of Radiology and Imaging Diagnosis - Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554