Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 5 - Sep. / Oct. of 2010
Vol. 43 nº 5 - Sep. / Oct. of 2010
|
ORIGINAL ARTICLE
|
|
Analysis of the Breast Cancer Control Program Information System (SISMAMA), with review of 1,000 mammograms in the cities of Barra Mansa and Volta Redonda |
|
|
Autho(rs): Sissy Bullos Lins dos Santos1; Hilton Augusto Koch2 |
|
|
Keywords: SISMAMA; SISMAMA analysis; SISMAMA review. |
|
|
Abstract: INTRODUCTION
Breast cancer control is a priority in the Brazilian health policy and has been included as one of the targets of the “Pacto pela Saúde (2006)” (Health Covenant), a program aimed at strengthening, integrating and promoting resoluteness of the Sistema Único de Saúde – SUS (the Brazilian unified health system). Since the disclosure in 2004 of the “Controle do Câncer de Mama: Documento de Consenso” (Consensus Document on Breast Cancer Control)( 1), governmental actions have been targeted at providing the population with the access to procedures for early detection of this disease, also called screening procedures or screening mammography, with yearly clinical examination of the breast for all women above 40 years of age, mammography for women in the age range between 50 and 69 years at a maximum two-year interval between examinations, and yearly clinical examination and mammography for women above 35 years of age at high risk for developing breast cancer. Still, there are situations in which routine mammography is also recommended, such as before starting hormone replacement therapy, prior to plastic surgery and in the postoperative follow-up of mastectomy , for the study of the contralateral breast, or after conservative surgery, and the so called diagnostic mammography performed in women with signs or symptoms of breast cancer. For the year of 2010, 49,240 new cases of breast cancer are expected. Breast cancer is the second most frequent type of cancer in the world, and the most frequent among women. Every year 22% of the new cases of cancer are breast cancer(1). With the objective of acting in a more practical and effective manner, based on data on breast cancer that could be regularly, safely and quickly evaluated, an electronic information system was developed, the “Sistema de Informação do Controle do Câncer de Mama” (SISMAMA)(Breast Cancer Information and Control System), aimed at creating a national databank aimed at gathering data from the different regions of the country on the disease through the standardization of mammography requisition forms e respective reports. The SISMAMA started operating in 2009, after the previous capacitation of the professionals involved in this process both at regional and municipal levels, promoted in 2008 by the State Health Secretariats. The SISMAMA system was jointly developed by the Instituto Nacional de Câncer and DATASUS/MS as from 2000 and, after an interruption, its development was resumed between 2005 and 2006, with the objective of obtaining data on breast cancer screening in the country. SISMAMA is a subsystem of the SUS outpatient billing system, in which the collected data are utilized for the billing of mammography, cytopathology and histopathology services and for the management of actions for breast cancer screening by the program coordination at municipal, regional and state levels. The SISMAMA relied on the collaboration of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR) in the matters related to mammography(2). This system automatically reproduces the Breast Imaging Reporting and Data System (BI-RADS®) categories, according to mammographic findings, allowing a reliable reporting of such findings within their respective categories, since the system excludes antagonistic information. This is an essential tool in the management of the disease control. MATERIALS AND METHODS This was a retrospective study, developed means of the analysis of mammography request forms and respective results records issued by SUS in the cities participating in the present study between August and October of 2009. Data were collected in a clinic located in the city of Barra Mansa, and in another in the city of Volta Redonda, RJ, Brazil. Both clinics are duly accredited and qualified by SUS, utilize the SISMAMA since 2009 and receive part of the patients in the region to be submitted to mammography. The data collection was carried out through the analysis of the information included in the requisition forms (filled in by the patient’s assisting physician or nurse in the original health service) and in the mammography results records (filled immediately after the examination, in part by the mammographers, and part by the radiologist responsible for the preparation of the mammographic report). The first phase of the study comprised the analysis of the mammography request forms (Figure 1) including the patient´s personal data such as name, address, age, ethnicity, schooling, and anamnesis data such as breast nodule, high risk for breast cancer, previous breast evaluation by a health professional and previous mammogram. Finally, clinical indication, as follows: screening or diagnosis; in the case of diagnostic mammography, marking of the affected breast (left or right) and type of finding (papillary lesion, papillary discharge, nodule, thickening or palpable lymph node).  Figure 1. Mammography request form: front (A) and back (B). The second phase comprised the analysis of the mammography results record form (Figure 2) that is filled in, part by the mammographer with data regarding anamnesis, menstrual background, use of hormones, information on pregnancy, radiotherapy treatment (if applicable, date of treatment), previous breast surgery and year. The other part is filled in by the radiologist with information on the number of films, radiological findings, BI-RADS category and respective recommendation. It is important to mention that the mammography results records defined by SUS/ SISMAMA consider the left and right breasts separately, also separating them by BI-RADS category.  Figure 2. Mammography results record form: front (A) and back (B). For the purposes of the present study, the major category was always taken into consideration, following the appropriate recommendation for such category. The main problems faced in the daily activities by the involved professionals as regards the deployment of the system and eventual failures or absence of data considered as relevant by SISMAMA were evaluated through the analysis of both forms and the data digitization. It is important to note that both forms were designed and distributed by the Ministry of Health, in the case of the results record form, with the collaboration of CBR; and in none of them changes were made by the authors in the course of the present study. It should also be mentioned that, in the results of the present study, some of the data were not taken into consideration, either for not representing relevant information, or for not being statistically significant. RESULTS The absence of any type o information in one of the 1,000 forms analyzed was the main issue in the present study (Figures 3 and 4). It can be observed that, on the results record form, the higher number of omissions were related to previous surgeries, generating antagonist data in the System and problems in the conclusion about category and data forwarding. Among such omissions, 267 occurred in Volta Redonda, and 35 in Barra Mansa, totaling 302 omissions (30.2%) (Figure 5). This item directly reflected on the final BI-RADS category in the diagnosis. In some situations disagreement was observed between the System and BIRADS, like that observed in the characterization of microcalcifications shape. This occurred whenever microcalcifications where characterized as punctate, independently from their distribution and recommendation for radiological follow-up of lesion classified as category 3, because the System considered them as category 4, recommending biopsy, and leading the reporting radiologist to characterize them as round instead of punctate. Among the 1% of reported cases with microcalcifications, 0.6%, i.e., more than half of this total, were punctate microcalcifications described as rounded, so that biopsy was not recommended. The inappropriateness or lack of any item on the forms designed by the Ministry of Health generated “adaptations” by the reporting radiologists. The lack of space (restriction in the number of characters) in the field for remarks was also a factor causing shortcoming on the reports, particularly in cases of unforeseen situations on the forms. Omissions on the mammography request form (Figure 3) 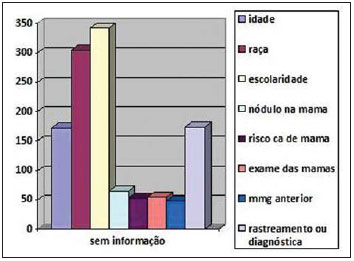 Figure 3. Omissions related to request form. Figure 3, regarding the first analysis phase, shows that the three major figures on omissions refer to schooling (342 patients), ethnicity (305), purpose of the study – screening or diagnosis (174), age (172), presence of a mass or lump in the breast (65), risk for breast cancer (53), previous clinical examination of the breast by a health professional (54) and, finally, information on a previous mammography (48). Among the reported figures on omissions, the one causing greatest impact on the final conclusion of the examinations by the SISMAMA was the information regarding the reason for performing the mammography, whether screening or diagnosis. Lesions previously classified as BI-RADS category 3 were not duly followed-up, besides complaints and clinical findings that could not be duly evaluated by the reporting radiologist. Additionally, the absence of data regarding other items generated undernotification. Omissions on the mammography results record form (Figure 4) 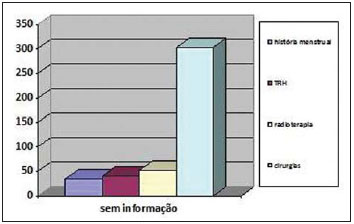 Figure 4. Omissions related to results record form. At the second analysis phase, the results record forms were evaluated, with the number of omissions shown on Figure 4. One observed in this phase of the study that the item with the highest number of omissions refers to information on previous breast surgery (302 omissions), followed by radiotherapy (52), hormone replacement therapy (41) and finally, menstrual background (35). The high number of omissions in the item regarding previous breast surgeries ended in error in the final version of the mammography reports, as the System excluded antagonistic data(2). This means that if a patient has undergone unilateral mastectomy, and such information is inappropriately omitted, the radiologist will have to report on the two breasts, as the System interprets such omission as if the patient still had both breasts, making it impossible to correctly complete the reporting. The correct filling of this item in particular was of paramount importance in the data input into the SISMAMA, and not filling it or doing it incorrectly, generates conflicting results and hinders the report completion. Data regarding previous breast surgeries (Figure 5) 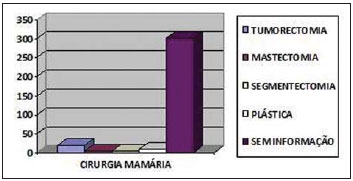 Figure 5. Data regarding previous breast surgery. On this Figure, a comparison is made, within the item regarding previous breast surgeries, demonstrating the most documented types of surgeries. Nevertheless, the omissions represented the greatest part of the cases (302), followed by tumorectomy (23), plastic surgeries (9) mastectomy and segmentectomy (both with 4 cases). Other types of surgery were not found in the studied sample. DISCUSSION BI-RADS is a system that classifies mammographic findings into categories and proposes clinical approaches according to each category. This system was developed by the American College of Radiology, with the objective of minimizing the differences in approaches inherent to due to interobserver variability (or disagreement)(3–6). SISMAMA was deployed to standardize mammographic reports and avoid deviations in images interpretation, and for that reason it adopts the BI-RADS, making data forwarding from SUS to the Ministry of Health, faster, easier and most reliable. Considering its recent implementation, it is important to analyze and document eventual occurrences that may be negatively impact the data forwarding process, not only as a result of the necessity of adjustments in the System itself, but also because of incorrect filling or failure in filling out the forms by the involved professionals. Omission of surgical data or inappropriate filling On the mammography results record form, the 11th subitem (regarding data of the anamnesis), there is question on previous breast surgeries and year, including different surgery modalities options (tumorectomy, segmentectomy, etc.). Obviously, it is appropriate that all patients’ data be accurately collected. However most of times the patients are unable to accurately report the procedure they were submitted to, so the professional performing the anamnesis must deduct the required information and hence the importance of a trained professional for the data collection. Most of times, the data collection is performed on the day of the examination by the mammographer. In the present study, this was the item with the highest number of omissions of data, totaling 302 (30.2% of the sample). This omission was also the one with greatest impact on the final result of the reports, as the reporting radiologist many times does not know that the System requires preliminary data to confirm what is described on the report. If the mammographer responsible for the anamnesis does not report a previous surgery, a postoperative architectural distortion, for example, considered as BI-RADS category 2 by the physician, will be taken as category 4 by the System, as there is no record on previous surgery. Likewise, skin thickening or retraction and architectural distortion will always be interpreted as a pathological finding if no data on previous surgery is available. Hence the importance of knowing the system and working in conjunction to use it properly. Another problem regarding the item on previous surgery is related to patients that underwent mastectomy and breast reconstruction. In spite of the two options being comprised in the item, one observed the recurrence of certain situations: cases of breast reconstruction where the mammographers report that the reconstruction was performed, but do not perform mammography for that side, generating the opening of a report for both breasts; or cases where in spite of the reconstruction, they only report mastectomy, performing bilateral mammography. In these cases, the System opens only the report for the preserved breast, disregarding the opening of the report for the reconstructed breast since it was not reported on the appropriate item. Among the four mastectomies reported in the sample, one had reconstruction without mammography of the reconstructed breast, with the System being fed only with the data regarding mastectomy, so that reporting on the reconstructed breast was not required, for which mammography was not performed, again causing wrong information to be entered into the System. The above described situations clearly demonstrate that the absence of correct information in the filling of anamnesis data is responsible for the greatest majority of errors in the interpretation of data by the System, and consequential failure in the data forwarding to the Ministry of Health. Postoperative architectural distortion, surgical sequels and actinic lesions In spite of the options for normal skin, skin thickening, and skin retraction (the two later ones being very common in cases of conservative surgery and actinic lesions) under sub-item “skin”, if one opts for skin retraction or skin thickening, and the field “anamnesis data” is not correctly filled out by the mammographer (as regards previous surgery), the system will automatically go to BI-RADS category 4, with the consequential recommendation for histopathological study for typical sequel. On the other hand, as the sub-item “previous surgeries” is correctly filled out, categories 2 or 3 will be accepted. There is no sub-item covering the typical breast volume reduction, a certain outcome in cases of conservative surgery. Parenchymal distortion under the surgical bed is a frequent occurrence, and most times it disappears within the first postoperative year. Only 3% of all mammograms demonstrate some degree of architectural distortion two or three years after biopsy of benign lesions(7). For breasts with distortion areas, the system provides two possibilities: a) the first one refers to focal distortion and its location. Its selection leads the System to automatically select a biopsy category (BI-RADS 4), independently of previous breast surgery reporting. This subitem was certainly created to anticipate situations with distortion not related to surgical procedures and with accurate indication for biopsy; b) the second one refers to postoperative architectural distortion, in which there is no possibility of localizing the lesion. In none of the two sub-items postoperatively observed focal parenchymal distortion is applied: the first one, for only comprising lesion susceptible to biopsy, and the second one, for the impossibility of localizing a distortion caused by a surgical sequel. Comparison with previous studies and mammographic follow-up for lesions classified as BI-RADS category 3 The comparison with previous images is indispensable in cases of mammographic follow-up for lesions classified as category 3. On the back of the mammography request form there is item 5-diagnostic mammography, which breaks down into 5-b radiological follow-up for category 3, and the professional responsible for filling in the form (nurse, assisting physician or duly trained personnel) is expected to provide such information. Certain confusion is observed in the forms, as many times a single mammography was indicated as for diagnostic and screening purposes, without any justification in cases where the study was diagnostic. In cases where the item radiological follow-up for category 3 is filled out, the System will only make the breast in question available for reporting. Nevertheless, the majority of such cases with incorrect filling of clinical indication in cases of follow- up of microcalcifications and nodules were not performed as follow-up, with repeated bilateral mammography in the first follow-up after six months (2.4%), generating unnecessary expenses with films and unnecessary radiation exposure for the patient. Aguillar et al., in their description of mammographic reports according to BIRADS, corroborate the recommendation for approaching lesions classified as category 3, with follow-up after six months (unilateral, only the breast with alteration), and bilaterally after 12, 24 and 36 months(7). The mammography results record form does not include any provision for comparison with previous images, i.e., even in the case of previous information being accurate, a follow-up for an appropriate period of time must be provided for, filling out the date of the previous study, and informing the patient as the mammography request form is filled - in the case of lesions requiring radiological follow-up (category 3) – , that she should always take the previous studies with her on the date scheduled for the new mammographic study, leaving them for comparison by the radiologist, thus avoiding that the patient be left with inappropriate follow-up of the lesion, and without a forecast for the determination of its stability. Microcalcifications As the interpretation of the BI-RADS category by the System is concerned, it is automatically done based on certain data provided by the reporting radiologist, together with other data collected by the mammographer. In the presence of microcalcifications, there is the possibility of classifying them according to their location, shape and distribution. In what regards to location, the options for breast quadrants and axillary extension are available in the System, and these topics have no impact on category classification. Subsequently, the System requests the shape, with the following options: rounded, punctate, irregular and branching; the distribution is also requested with the following options: clustered, segmented and ductal. When the reporting radiologist characterizes the calcifications as rounded, the System automatically categorizes the findings as BI-RADS category 3; when the microcalcifications are described as punctate, the System categorizes the finding as BI-RADS category 4, and consequently recommending histopathological study. Clustered, rounded or punctate calcifications (clustered calcifications in a circular or ovoid arrangement, suggestive of lobular origin) are classified as category 3, and clustered, monomorphic, predominantly punctate or rounded calcifications; if absent in previous study, are classified as BI-RADS category 4a(7). According to Kopans, very rounded, punctuate, regular calcifications are rarely associated with breast cancer. However, if they include, or are associated with calcifications whose shapes are not rounded or smooth, but rather heterogeneous, they should be considered as suspicious(8). In the present sample, 0.6% of all the microcalcifications, in spite of being actually punctuate, were reported as rounded in order to avoid categorization for biopsy in findings with characteristics of benignity, again generating a distortion in the data forwarding. Enlarged axillary lymph nodes BI-RADS does not contemplate lymph node alterations. This is a controversial point for radiologists, as an occult carcinoma may present with lymph node alteration as its single manifestation. For this reason, some radiologists consider biopsy in the presence of such alterations, as does the SISMAMA, considering any lymph node alteration (enlargement, density alteration and confluence) as category 4, with indication for biopsy. Aguillar et al.(7) consider as probable that the BI-RADS committee, on the next issue, will adopt the following classification for axillary adenopathy: if related to rheumatoid arthritis or sarcoidosis – category 2; related to lesion requiring further investigation with other imaging method (ultrasonography, magnetic resonance imaging) – category 0; related to a lesion requiring biopsy – category 4; and, if related to other known disease (lymphoma, leukemia) – category 6. Restricted space for general observations In certain cases, the radiologist faces unusual situations that require a justification for the report or even information to the assisting physician. In the case of SUS patients, accessing the requesting physician may be very difficult or not feasible at all because of the number of studies to be reported. So the space left in the field for general observations may be the single form of contact between the professionals. In seven cases of the present sample the space in the field for general observations was simply not enough to clarify points of the reports; five of these cases were from Barra Mansa, and two from Volta Redonda. Unforeseen situations and findings Findings observed outside the breast parenchyma – During the forms analysis, difficulty in the completion of some reports was observed, most of times because of disagreement in data being fed into the System, and in other cases because the findings were not foreseen by the System. Such was the case, for example, of a patient submitted to quadrantectomy and radiotherapy sessions in 2007, with histopathological diagnosis of infiltrating ductal breast carcinoma affecting the skin, classified as BI-RADS category 5. Follow-up mammography was performed in August 2009, on which three small skin nodules were found and confirmed at clinical examination. The nodules were located on the skin next to the surgical scar, and the need for biopsy could not be ruled out because of the previous histopathological result, which reported extension to the skin, with high probability for local recurrence. The System does not comprise the presence of skin nodules, only in the breasts. As a nodule and its location are identified, the possible options comprise quadrants, retroareolar region, and axillary extension, implying that that all mentioned nodular lesions are within the breast. In the subitem “general observations”, it would not be possible to report the case because of the limited number of characters. In this specific case, a telephone call was made to the assisting physician, explaining that the limitations inherent to the System did not allow an appropriate description of the case. In the present sample, this occurred with a single case (0.1%). Steatonecrosis – Another common postoperative finding refers to steatonecrosis. This is a common benign condition that may be asymptomatic or may be present as a palpable mass, with pain or associated findings, such as skin thickening or nipple retraction. Steatonecrosis may present with different mammographic appearances. Radiotransparent well-circumscribed masses, mixed fat densities and soft tissue with or without calcified rim, known as lipid cysts constitute common and typical findings(9). These findings may be observed after any trauma in the breast, including surgery. Steatonecrosis is commonly seen after a nodule resection and radiotherapy for breast carcinoma and after an extensive surgery; however such finding is not covered by the System. No report on these findings was observed in the sample. Accessory breasts – Other unforeseen situations of lesser relevance are the relatively common cases of accessory breasts. There is no mention of such alteration in the item regarding “other findings”, in which it could be mentioned. Gynecomastia – Although the present study is about female patients because they are the vast majority of those being submitted to mammography, it is important to mention that cases of gynecomastia are not comprised by the System. CONCLUSION It is obvious that no available computer system can anticipate all the situations and variables involved in a process, which also depend on the subjective analysis of the reporting radiologist. Adjustments are necessary in the System, and even more important, appropriate training of the professionals involved in the process. Actually, what is intended is anticipating some relatively recurrent situations to improve the System with more accurate technical information. Undoubtedly, SISMAMA is a project that provides greater agility in the processing of data necessary for planning actions in health and better resources allocation. However, considering the short training time, the System is still underutilized by technicians, physicians and other involved professionals; not all of them know how it works and the importance of filling out the forms as accurately as possible to avoid the exclusion of antagonistic data. Physicians, technicians and those professionals responsible for the processing of such data should know the operation of the System to allow that the statistical data generated by the System be accurately forwarded to the Ministry of Health, reducing undernotification and erroneous notifications with consequential inappropriate allocation of financial resources. Reviews and adjustments in the System are in fact necessary, however proper training of involved professionals is the crucial point. REFERENCES 1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Controle do câncer de mama – documento de consenso. [acessado em 25 de maio de 2010]. Disponível em: www.inca.gov.br 2. SISMAMA Internet. [acessado em 10 de novembro de 2009]. Disponível em: www.datasus.gov.br/siscam/siscam.php 3. Althoff FP, Petrelli ASC. Correlação dos achados mamográficos com o sistema BI-RADS. [Monografia]. Rio de Janeiro, RJ: Curso de Pós-Graduação da Santa Casa de Misericórdia do Rio de Janeiro; 2005. 4. American College of Radiology. ACR BI-RADSMammography. 4th ed. In: ACR Breast Imaging Reporting and Data System, Breast Imaging Atlas. Reston, VA. American College of Radiology; 2003. 5. Berg WA, Campassi C, Langenberg P, et al. Breast Imaging Reporting and Data System: inter- and intraobserver variability in feature analysis and final assessment. AJR Am J Roentgenol. 2000;174:1769–77. 6. Godinho ER, Koch HA. Submissão às recomendações do BI-RADS por médicos e pacientes: análise preliminar de 3.000 exames realizados em uma clínica particular. Radiol Bras. 2004;37:21–3. 7. Aguillar V, Bauab S, Maranhão N. Relatório mamográfico e ultra-sonográfico segundo o BIRADS. Guia e dúvidas. In: Aguillar V, Bauab S, Maranhão N. Mama – diagnóstico por imagem. 1ª ed. Rio de Janeiro, RJ: Revinter; 2009. p. 301–4. 8. Kopans DB. Analisando a mamografia. In: Kopans DB, editor. Imagem da mama. 2ª ed. Rio de Janeiro, RJ: Medsi; 1998. p. 332. 9. Jackson VP, Jahan R, Fu YS. Lesões benignas da mama. In: Basset LW, Jackson VP, Jahan R, et al., editores. Doenças da mama. Diagnóstico e tratamento. 1ª ed. Rio de Janeiro, RJ. Revinter; 2000. p. 372–5. 1. MD, Post-graduate in Radiology and Imaging Diagnosis, Pontifícia Universidade Católica do Rio de Janeiro (PUC-Rio), Rio de Janeiro, RJ. 2. PhD, Head for the Unit of Radiology, Santa Casa da Misericórdia do Rio de Janeiro and Courses of Post-graduation at Pontifícia Universidade Católica do Rio de Janeiro (PUC-Rio), Rio de Janeiro, RJ, Brazil. Mailing address: Dra. Sissy Bullos Lins dos Santos Rua Cinco de Julho, 94/601, Copacabana Rio de Janeiro, RJ, Brazil, 22051-030 E-mail: sissybullos@yahoo.com Received May 25, 2010 Accepted after revision September 13, 2010 Study developed at the Unit of Radiology and Post-graduation Prof. Dr. Hilton Koch, Santa Casa da Misericórdia do Rio de Janeiro, RJ, Brazil. Data collection in private clinical centers under contract to the SUS (the Brazilian unified health system) in the cities participating in the present study |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554