Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 4 - July / Aug. of 2010
Vol. 43 nº 4 - July / Aug. of 2010
|
CASE REPORT
|
|
Madelung's disease: a case report and literature review |
|
|
Autho(rs): Maria da Graça Caminha Vidal1; Carlos Jesus Pereira Haygert2; André Rivas Zagoury3; Sâmia Braga Ramos Adaime4; Rodrigo Previdello Carrion5; Thizá Massaia Londero6 |
|
|
Keywords: Madelung's disease; Benign symmetric lipomatosis; Head and neck neoplasms; Computed tomography. |
|
|
Abstract: INTRODUCTION
Madelung's disease, also known as multiple symmetrical lipomatosis, benign symmetrical lipomatosis or Lanois-Bensaunde adenolipomatosis, is a rare benign entity of unknown etiology, clinically characterized by the presence of multiple and symmetric, non-encapsulated masses of fatty tissue, usually involving the neck and the upper region of the trunk(1). First reported by Benjamin Brodie in 1846, its classical horse collar pattern of cervical lipomas distribution was described by Otto W. Madelung in 1888. In 1898, Launois and Bensaude concluded the description of the syndrome, naming it "multiple symmetrical adenolipomatosis". About 200 cases of this disease are reported in the literature(1,2). CASE REPORT A male, white, 43-year-old patient, was referred to the Service of Head & Neck Surgery of Hospital Universitário de Santa Maria, with a ten-year history of an expansive cervical lesion. The neck tumors presented slow growth and progressive increase. Dyspnea, dysphagia or hoarseness were not reported. The current complaint was a "tightness" sensation in the infrahyoid region over the past five months. The patient was not obese, previously healthy and was alcoholic and smoker for fifteen years. At physical examination, the patient presented with good general condition, with poorly defined masses, firm at palpation, located in the subcutaneous tissue on the anterior and lateral cervical regions (Figure 1). A computed tomography (CT) study was requested and demonstrated extensive cervical lipomatosis, with the adjacent structures being preserved (Figure 2). Routine laboratorial tests were normal. 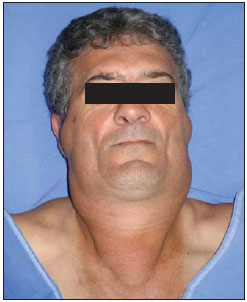 Figure 1. Preoperative appearance of a patient with Madelung’s disease. Presence of poorly defined, hardened subcutaneous masses in the anterior and lateral cervical regions. 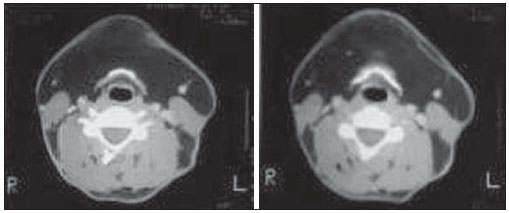 Figure 2. Computed tomography of the cervical region. Axial CT sections demonstrate extensive cervical lipomatosis and preserved adjacent structures. Once the diagnosis of Madelung's disease was established, the surgical treatment was defined with basis on the symptoms, physical deformity and the patient's will. The patient was submitted to exeresis of the lesion, with dissection of the tumor mass. The surgical specimen was sent for anatomopathological analysis, which revealed the presence of mature fatty tissue compatible with lipomatosis. The postoperative period was uneventful, with symptoms relief (Figure 3).  Figure 3. Anterior view of the patient after cervical lipoma resection. Satisfactory progression, with symptoms relief. DISCUSSION Madelung's disease is characterized by accumulation of non-encapsulated fatty tissues symmetrically distributed in the upper portion of the body. Lipomas develop in the cervical region (horse collar), deltoid region (pseudoathletic appearance) and on the back (pseudo-kyphosis or humpback). Eventually such lipomas may develop in more caudal portions of the body. In general, the face, hands and feet are not affected. The course of the disease is variable. It usually presents with a rapid initial growth for months or even years, followed by a long period of stabilization or slow progression of the disease. In advanced cases compression of the aerodigestive tract may be observed, causing dyspnea, stridor and dysphagia that are the most significant complications of the disease. The anterior and posterior cervical regions (100%), the retroauricular region (95%), the deltoid region (84%), the trunk (60%), the abdomen (58%), the inguinal region (42%) and the upper part of the lower limbs (42%) are the most affected regions(2-6). The disease predominantly affects white males (15 men:1 woman), with highest incidence amongst the Mediterranean population. The fat deposition occurs between the third and the fifth decades of life. Approximately 60% to 90% of the patients present a previous history of moderate to severe alcoholism(2). The diagnosis is based on the recognition of the unique clinical appearance and complementary studies in order to rule out other diseases. Usually, CT and/or magnetic resonance imaging (MRI) are requested. Currently, CT is considered as the method of choice for the diagnosis, preoperative staging and postoperative follow-up(1,2). The tomographic documentation provides identification of the most common findings, such as lipomatosis in typical sites, calcification or ossification within the lipomas, tracheal narrowing or deformity, venous stasis on chest walls and absence of masses in other sites such as the abdomen, retroperitoneum or the pericardium, besides allowing the ruling out the presence of other complications(4-8). The use of ultrasonography is discarded, as CT provides for a higher diagnostic fidelity. MRI findings overlap with those of CT, however one should consider that MRI is a much more expensive and less accessible method(3,4). The standard treatment is surgical resection, with absolute indication when there are evidences of aerodigestive compression and presence of esthetic deformities. The extremely infiltrative nature of these hardened masses make their surgical removal more difficult. Liposuction presents lower perioperative mortality rates compared with conventional surgery(1-3). Clinical therapy utilizing drugs, alcohol abstinence and weight loss do not result in reversion neither avoid progression of the disease(4-6). Lipomas recurrence is frequently observed. Because of their infiltrative nature, the prognosis is determined by size, location and extent of the lipomatous accumulation. The presence of peripheral neuropathy results in increased morbidity and worse prognosis(5). REFERENCES 1. Farias TP, Dias FL, Freitas EQ, et al. Tratamento cirúrgico da doença de Madelung: relato de caso. Rev Bras Cir Cabeça Pescoço. 2003;32:23-6. 2. Adamo C, Vescio G, Battaglia M, et al. Madelung's disease: case report and discussion of treatment options. Ann Plast Surg. 2001;46:43-5. 3. Souza RP, Paes Junior AJO, Rapoport A. Doença de Madelung (lipomatose cervical benigna simétrica): relato de dois casos. Radiol Bras. 2003;36:121-2. 4. Kohan D, Miller PJ, Rothstein SG, et al. Madelung's disease: case reports and literature review. Otolaryngol Head Neck Surg. 1993;108:156-9. 5. Vieira MV, Grazziotin RU, Abreu M, et al. Lipomatose simétrica múltipla (doença de Madelung): relato de um caso. Radiol Bras. 2001;34:119-21. 6. Argenta LC, McClatchey KD, Ferrell WJ, et al. Benign symmetrical lipomatosis (Madelung's disease). Head Neck Surg. 1981;3:240-3. 7. Smith PD, Stadelmann WK, Wassermann RJ, et al. Benign symmetric lipomatosis (Madelung's disease). Ann Plast Surg. 1998;41:671-3. 8. Feldman DR, Schabel SI. Multiple symmetrical lipomatosis: computed tomographic appearance. South Med J. 1995;88:681-2. 1. Specialization in Cancerology and Oncological Surgery, Assistant Professor, Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil 2. Medical Residence in Radiology and Imaging Diagnosis, Assistant Professor at Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil 3. MD, General Surgeon, Medical Residence in General Surgery at Hospital Universitário de Santa Maria (HUSM) - Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil 4. MD, Resident in General Surgery at Hospital Orêncio Freitas, Niterói, RJ, Brazil 5. MD, Resident in Ophthalmology at Hospital de Clínicas de Porto Alegre (HCPA), Porto Alegre, RS, Brazil 6. Graduate Student of Medicine, Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil Study developed at the Service of Head & Neck Surgery, Hospital Universitário de Santa Maria (HUSM) - Universidade Federal de Santa Maria (UFSM), Santa Maria, RS, Brazil Mailing address: Dra. Sâmia Adaime Rua Jornalista Moacir Padilha, 70, Bloco 1, ap. 1001, Centro 24020-350. Niterói, RJ, Brazil E-mail: sbra5@hotmail.com Received October 19, 2009 Accepted after revision February 5, 2010 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554