Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 4 - July / Aug. of 2010
Vol. 43 nº 4 - July / Aug. of 2010
|
ICONOGRAPHIC ESSAY
|
|
Magnetic resonance imaging in the evaluation of periosteal reactions |
|
|
Autho(rs): Marcello Henrique Nogueira-Barbosa1; José Luiz de Sá2; Clóvis Simão Trad3; Rodrigo Cecílio Vieira de Oliveira4; Jorge Elias Júnior1; Edgard Eduard Enge4; Marcelo Novelino Simão6; Valdair Francisco Muglia1 |
|
|
Keywords: Periostitis; Bone neoplasm; Magnetic resonance imaging. |
|
|
Abstract: INTRODUCTION
The initial approach to bone lesions is based on the evaluation of conventional radiographic images. The classic radiological semiology of focal bone lesions includes the identification and characterization of periosteal reactions. Usually, periosteal reactions are classified into some classic subtypes and the identification of such subtypes may occasionally be useful and suggest the presence of a specific disease or neoplasm(1,2). Generally, processes involving intense activity or fast progression result in more aggressive periosteal reactions, and indolent processes result in non-aggressive presentations(1,2). Interrupted periosteal reactions indicate the presence of biologically aggressive processes. However, there is a considerable overlap of imaging findings and the simple classification of periosteal reaction does not sufficiently define the nature or aggressiveness of the lesion(3). Although magnetic resonance imaging (MRI) is considered as the best method for local staging of musculoskeletal lesions(4- 6), it is possible that the MRI capability of evaluating periosteal alterations is being underestimated. For example, a recent published review about periosteal reactions intended to education of medical residents in imaging diagnosis does not include a specific discussion on the evaluation of periosteal reactions by MRI(1). The present iconographic essay is aimed at stimulating a careful evaluation of periosteal reactions at MRI. Cases os periosteal reactions observed by MRI are illustrated and correlated with conventional radiography and other imaging diagnosis methods. PERIOSTEAL REACTION Figure 1 demonstrates a normal periosteum identified on MRI images. Frequently, the normal periosteum is not even individualized by MRI images. In the event of an insult that induces periosteal reaction, vascular proliferation and thickening of the normal periosteum are observed as a response to a triggering factor. The causes of periosteal reaction are extremely varied and a comprehensive list should include tumors, infection, trauma, drugs, venous stasis, congenital osteometabolic disorders and arthritis. 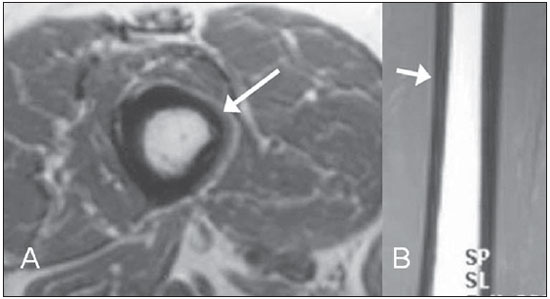 Figure 1. Magnetic resonance imaging demonstrating a thigh with a normal appearance. A: Axial, T1-weighted image demonstrates a thin concentric lamina with intermediate signal intensity on the periosteum (arrow). B: Coronal, T1- weighted image where an arrow also indicates the topography of a normal periosteum. The morphology of periosteal reaction reflects the intensity, duration and aggressiveness of the triggering agent(1,2). The periosteal reaction becomes visible at conventional radiography only in the presence of a certain degree of mineralization that takes about 10-21 days to be achieved(2). TYPES OF PERIOSTEAL REACTION Solid Solid periosteal reaction represents a continuous bone neoformation attached to the external cortical surface, typically occurring as a response to indolent and benign processes(1,2). Solid periosteal reaction can be thin (Figures 2 and 3) but, sporadically, chronic processes may cause thicker solid reactions (Figure 4). 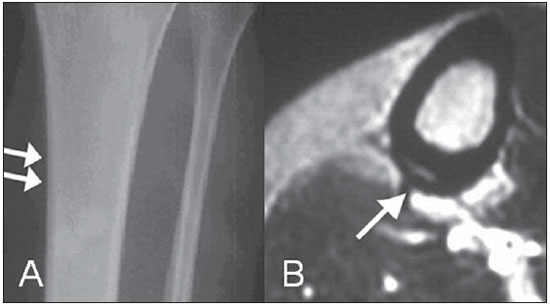 Figure 2. A: Lamellar periosteal reaction on the medial aspect of the tibial diaphysis in a case of stress fracture (arrows). B: Lamellar periosteal reaction on an axial MRI, T2-weighted image (arrow). Additionally, increased fluid signal can be observed at the adjacent soft tissues. 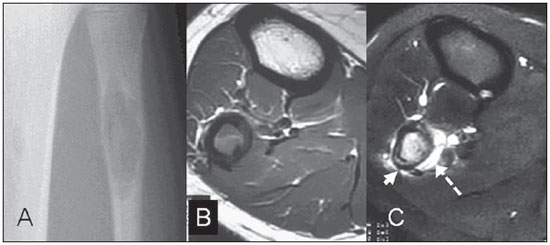 Figure 3. Lamellar periosteal reaction related to subtle pathological fracture of the fibular cortex in a fibroma non ossificans. A: Plain radiography demonstrates osteolytic lesion with geographic contour and slightly insufflative. B: Axial, T1- weighted image demonstrates decreased signal intensity in the fibular bone marrow and posterior cortical fracture. C: Axial T2-weighted image with fat saturation demonstrating increased intraosseous fluid signal and increased fluid signal at the adjacent soft tissues. The arrow indicates fracture- related periostitis. 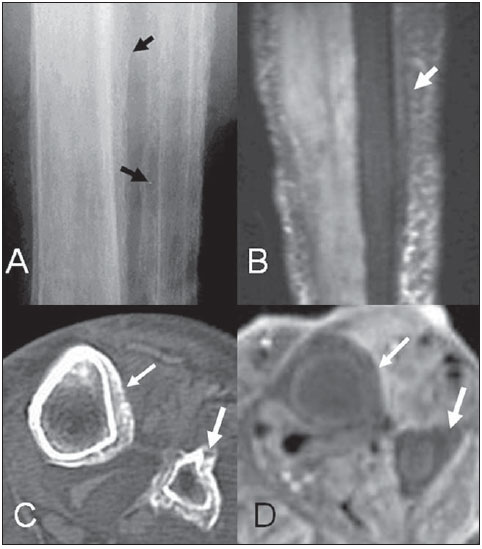 Figure 4. Solid periosteal reaction secondary to chronic venous stasis of lower extremity. A: Conventional radiography demonstrates periosteal reaction in the tibia and fibula (black arrows). B: MRI T2-weighted image with fat saturation also demonstrates periosteal reaction (white arrow). Axial computed tomography (C) and axial MRI T1- weighted image with fat saturation (D), both of them confirming the circumferential involvement of the periosteal reaction. Lamellar or multilamellar Multilamellar periosteal reaction (Figure 5), also denominated "onion skin" is caused by deposition of concentric, sheetlike layers of mineralized periosteal new bone, separated by vascular dilatation and loose connective tissue(1-3). In cases of association with malignant tumors, the spaces between the layers may become secondarily infiltrated by malignant cells. Possible associations include: Ewing sarcoma, osteosarcoma, osteomyelitis and aneurysmal bone cyst, among others(3). 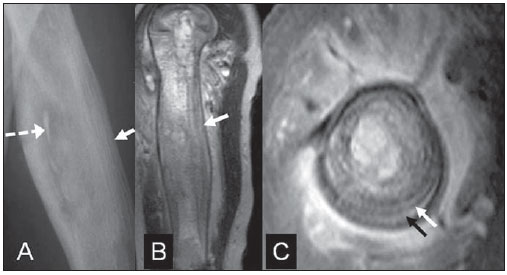 Figure 5. A: Multilamellar periosteal reaction (white arrow) with an “onion skin” pattern identified by plain radiography in the humeral diaphysis in a child aged approximately one year and eight months with surgically confirmed chronic osteomyelitis. Sequestrum is indicated by the dashed white arrow. B: Sagittal MRI T2-weighted image confirms the presence os multilamellar periosteal reaction (white arrow). C: Axial MRI T2-weighted image demonstrates multiple concentric lamellar depositions on the periosteum (arrows). Spiculated pattern, arising perpendicular to the bone cortex Spiculated periosteal reaction corresponds to thin spicules arranged perpendicular to the bone cortex (Figure 6). Such spicules are not neoplastic and originate from the ossification along periosteal vascular channels and fibrous bands (Shapey's fibers) stretched away from the bone cortex(1-3). The loose areolar tissue between spicules may be later replaced by a tumor or other tissues. 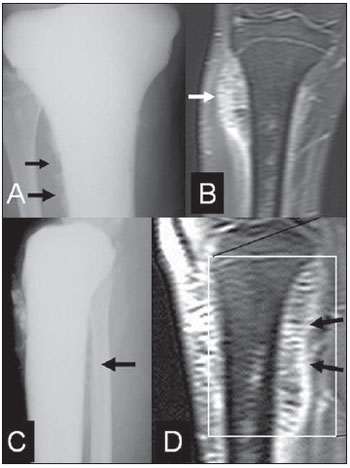 Figure 6. A,C: Tibial osteosarcoma presenting spiculate periosteal reaction perpendicular to the bone cortex surface (black arrow) identified at plain radiography respectively on anteroposterior and lateral views. B,D: Spicules with low signal intensity arranged perpendicular to the tibial axis demonstrated by MRI. In the present case, the periosteal reaction is more noticeable at MRI than at plain radiography. B: Coronal, gadolinium-enhanced MRI T1-weighted image with fat saturation. D: Sagittal MRI T2- weighted image with fat saturation. Sun ray pattern In the divergent spiculated or "sun ray" periosteal reaction, the spicules extend into an epicenter in the bone tissue (Figures 7 and 8). Sun ray periosteal reaction is generally perceived as a sign of malignancy and is frequently associated with osteosarcoma(1,3), although it may be observed in benign lesions such as osteoblastomas and hemangiomas(3). 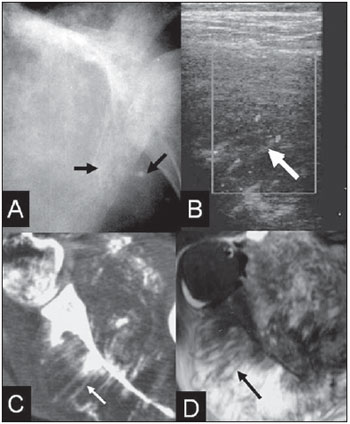 Figure 7. Spiculated “sun ray” periosteal reaction in an Ewing’s sarcoma of the scapula. A: Plain radiography with arrows indicating periosteal reaction with some divergent spicules. B: Doppler ultrasonography confirming the presence of spicules (arrow) and increased periosteal vascularization. C: Axial computed tomography image. The Arrow indicates one of the spicules of the periosteal reaction. D: The same appearance can be identified on axial MRI T1-weighted image acquired following intravenous contrast agent injection. The arrow indicates one of the periosteal spicules. 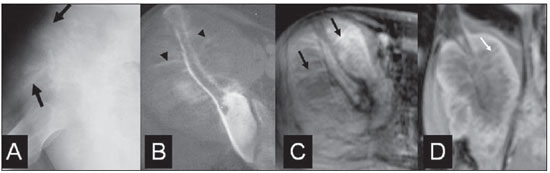 Figure 8. Divergent spiculated periosteal reaction indicated by arrows in a proved case of iliac osteosarcoma. A: Plain radiography. B: Axial computed tomography. C,D: Respectively, contrast-enhanced axial and coronal MRI T1-weighted images. Codman's triangle Codman's triangle is the interrupted version of the lamellar and multilamellar periosteal reaction (Figures 9 and 10). Generally, the region of the Codman's triangle is tumor-free, but may be secondarily infiltrated(7). This type of periosteal reaction was firstly described in cases of osteosarcoma, but it can be observed in other primary malignant tumors or bone metastases in osteomyelitis, in trauma, and in benign, but active tumors, such as aneurysmal bone cysts(1,3). 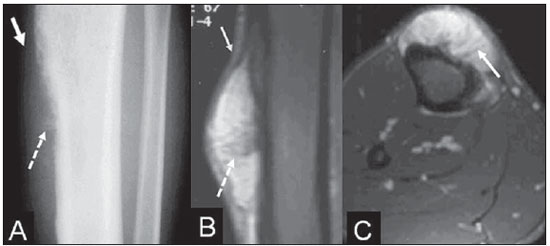 Figure 9. Periosteal osteosarcoma in the tibia. A: At radiography, one can identify interrupted (continuous arrow) and spiculated (dashed arrow) periosteal reactions. B: Coronal MRI T1- weighted image acquired following intravenous contrast injection demonstrating spiculated periosteal reaction (dashed arrow). On the same image, in the cranial region of the periosteal reaction, one can observe an area resembling the Codman’s triangle pattern traditionally described at radiography. C: Axial, contrast-enhanced MRI T1-weighted image with Arrow indicating spiculated periosteal reaction. 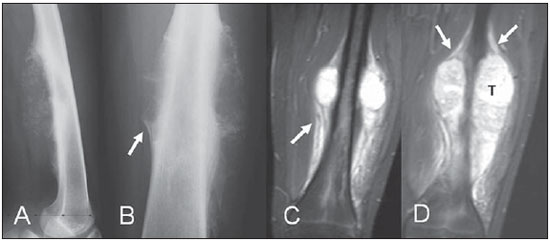 Figure 10. A,B: Plain radiography, orthogonal views of a femur in another case of osteosarcoma. Besides spiculated periosteal reaction, this case demonstrates a Codman’s triangle (arrow). C,D: Coronal MRI T2- weighted images confirm the presence of interrupted periosteal reaction similar to the Codman’s triangle observed at radiography. DISCUSSION The prevalence of the different types ofperiosteal reaction in each type of bone tumor is relatively poorly documented in the literature(3). Notwithstanding, the description of the above described periostealreaction subtypes is a usual practice in conventional radiological reports. Few descriptions are found in the literature about MRI in the study of periosteal reactions(8-10). An experimental study has evaluated the most effective method for identifying periostitis following induction of leg bone infection in rabbits, comparing conventional radiology, contrast-enhanced computed tomography and MRI, using histology as the gold standard(8). In such study, MRI was considered as the best method in the identification of periosteal elevation, being capable of identifying periostitis even in the absence of ossification. Two cases of false-positive result were observed with MRI. Another study has blindly compared conventional radiology and MRI as to the presence and classification of periosteal reactions in osteosarcomas, observing a good correlation between both methods(10). CONCLUSION The semiological patterns of periosteal reactions observed at conventional radiography can be extrapolated to magnetic resonance imaging. Considering the relevance of the findings, the identification and characterization of periosteal reaction at MRI should be stimulated. Acknowledgements To Fundação de Apoio ao Ensino, Pesquisa e Assistência (FAEPA) - Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo, for the financial support provided under Nbr.481/2009 for the development of the present study. REFERENCES 1. Rana RS, Wu JS, Eisenberg RL. Periosteal reaction. AJR Am J Roentgenol. 2009;193:W259-72. 2. Resnick D. Tumors and tumor-like lesions of bone: radiographic principles. In: Resnick D, editor. Diagnosis of bone and joint disorder. 3rd ed. Philadelphia, PA: WB Saunders; 1995. p. 3613-27. 3. Wenaden AET, Szyszko TA, Saifuddin A. Imaging of periosteal reactions associated with focal lesions of bone. Clin Radiol. 2005;60:439-56. 4. van Trommel MF, Kroon HM, Bloem JL, et al. MR imaging based strategies in limb salvage surgery for osteosarcoma of the distal femur. Skeletal Radiol. 1997;26:636-41. 5. Onikul E, Fletcher BD, Parham DM, et al. Accuracy of MR imaging for estimating intraosseous extent of osteosarcoma. AJR Am J Roentgenol. 1996;167:1211-5. 6. Frouge C, Vanel D, Coffre C, et al. The role of magnetic resonance imaging in the evaluation of Ewing sarcoma. A report of 27 cases. Skeletal Radiol. 1988;17:387-92. 7. Codman EA. Registry of bone sarcoma; part I, twenty-five criteria for establishing diagnosis of osteogenic sarcoma; part II, 13 registered cases of 5 year cures analyzed according to these criteria. Surg Gynecol Obstet. 1926;42:381-93. 8. Spaeth HJ, Chandnani VP, Beltran J, et al. Magnetic resonance imaging detection of early experimental periostitis. Comparison of magnetic resonance imaging, computed tomography, and plain radiography with histopathologic correlation. Invest Radiol. 1991;26:304-8. 9. Greenfield GB, Warren DL, Clark RA. MR imaging of periosteal and cortical changes of bone. Radiographics. 1991;11:611-23. 10. Dosdá R, Martí-Bonmatí L, Menor F, et al. Comparison of plain radiographs and magnetic resonance images in the evaluation of periosteal reaction and osteoid matrix in osteosarcomas. MAGMA. 1999;9:72-80. 1. PhDs., Professors at Centro de Ciências das Imagens e Física Médica (CCIFM), Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil 2. MD, Resident at Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil 3. PhD, Volunteer Faculty at Centro de Ciências das Imagens e Física Médica (CCIFM), Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil 4. MD, Radiologist, Clínica de Diagnóstico por Imagem Tomoson, Araçatuba, SP, Brazil 5. PhD, Professor, Department of Locomotor Apparatus Biomechanics, Medicine and Rehabilitation, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRP-USP), Ribeirão Preto, SP, Brazil 6. Master, Physician Assistant at the Service of Radiodiagnosis, Centro de Ciências das Imagens e Física Médica (CCIFM), Hospital das Clínicas, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil Study developed at the Service of Radiodiagnosis of Centro de Ciências das Imagens e Física Médica (CCIFM), Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (HCFMRP-USP), Ribeirão Preto, SP, Brazil Mailing address: Dr. Marcello Henrique Nogueira-Barbosa Avenida Bandeirantes, 3900, Campus Universitário 14048-900. Ribeirão Preto, SP, Brazil E-mail: marcello@fmrp.usp.br Received February 11, 2010 Accepted after revision March 26, 2010 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554