Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 4 - July / Aug. of 2010
Vol. 43 nº 4 - July / Aug. of 2010
|
ORIGINAL ARTICLE
|
|
Endovascular treatment of scalp cirsoid aneurysms |
|
|
Autho(rs): Eduardo Wajnberg1 |
|
|
Keywords: Arteriovenous fistula; Cirsoid aneurysm; Cerebral angiography; Embolization. |
|
|
Abstract: INTRODUCTION
Cirsoid aneurysm, also known as serpentinum aneurysm or plexiform angioma, is a term corresponding to vascular malformations of the scalp, drained by dilated and tortuous veins generally presenting large varicosities. These lesions may be either congenital or traumatic in etiology, with the majority of the first ones becoming symptomatic only at the third decade of life. Sixty percent of affected individuals are male(1). The location of scalp cirsoid aneurysms is more or less evenly distributed among the frontal, temporal and parietal regions(1). The main complaint of the majority of patients with such vascular lesions is the presence of a pulsatile mass causing scalp deformity. In some cases, bruit or focal headache is reported. At clinical examination, most patients present a noticeable pulsatile tumor-like lesion surrounded by dilated vessels and an audible bruit at auscultation. However, the primary abnormality is a fistula that is clinically and angiographically evidenced by the secondary dilation of its draining veins. Arteriovenous fistulas originate in the embryonic vascular development and vary according to the phase where an abnormal growth takes place(2,3). As a result, angiography may demonstrate different findings such as the presence of a nidus or even an associated hemangioma in congenital cases(1,4-8). Considering that each lesion presents a range of typical angioarchitectural characteristics, the treatment should be tailored to each patient's circumstance. In some cases of major malformations with high-output fistulas, a combined endovascular/surgical approach and reconstruction of the scalp may be the best treatment method(8). The author reports a series of four patients with arteriovenous malformations of the scalp treated by endovascular approach. All the patients shared a common previous history of blunt head trauma progressing with the development of a pulsatile mass. All of them were treated with embolization either by transarterial approach or by direct puncture of the lesion with the utilization of liquid-type adhesives. No recurrence was observed during the follow-up period. MATERIALS AND METHODS Four patients with scalp cirsoid aneurysms were assisted by the group of Interventional Radiology at the Hospital Universitário Clementino Fraga Filho from the Federal University of Rio de Janeiro, RJ, Brazil, in the period from August/2004 to January/2009. The clinical findings and treatment methods are summarized on Table 1. All four patients presented a previous history of blunt cranial trauma and slow development of a pulsatile mass on the scalp. All the lesions were diagnosed with basis on their clinical characteristics and confirmed by angiography. Angiographically, all the patients presented cirsoid aneurysms consisting in direct, high-output arteriovenous fistulas, without the presence of any plexiform component or nidus. The patients were submitted to complete cerebral angiography with bilateral, selective injections into the internal and external carotid arteries to demonstrate the size and location of the afferent arteries and draining veins. All of the lesions were supplied by combinations of the superficial temporal, occipital and middle meningeal arteries. 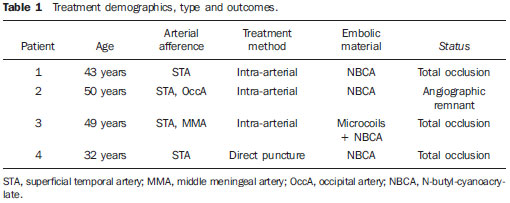 Embolization techniques Direct puncture embolization - The procedure was performed under sedation and local anesthesia. Following selective angiography, the lesions were punctured with a 21G Teflon needle at the level of the variceal dilatation proximal to the fistula. Angiography was performed with and without manual compression of the venous drainage in the region. In order to achieve a decrease in the circumferential flow around the lesion, a sterile, round metal ring was maintained in place on the dilated collector vein. Technically, direct venography should not demonstrate distal leakage of contrast medium through the metal ring borders indicating an appropriate venous compression. As a higher pressure is applied on the metal ring, the arterial flow can also be reduced, so that a complete flow reduction is achieved in the desired region. With the ring in place, N-butyl-cyanoacrylate (NBCA) mixed with lipiodol was injected into the collector vein. Then, the ring remains in place for some minutes and later is gradually removed. The NBCA concentration mixed with iodized oil was adjusted in accordance with the flow observed at angiography. Repeated punctures and injections were performed as a residual lesion was observed on a postembolization angiogram. Transarterial embolization - Transarterial embolization was performed with the standard microcatheterization technique, by femoral puncture and placement of a 6Fr system with a guide catheter in the external carotid artery. An Ultraflow 1.5Fr microcatheter (MTI Microtherapeutics; Irvine, CA, USA) was utilized for cyanoacrylate injection, and the embolization was performed with NBCA mixed with lipiodol at a concentration compatible with the flow velocity in the fistula. RESULTS All of the four patients included in the present series had malformations with high-output fistulas and were treated solely with embolization. In none of the reported cases, the presence of nidus in the malformations was observed, and in all of the cases the visualized angioarchitecture presented large arterial afferences in high-output fistulas towards large caliber varicose veins. One patient presented intracranial drainage through diploic veins towards the superficial middle cerebral vein and petrosal sinuses. Three patients were submitted to endovascular treatment by transarterial embolization and only one was treated by means of direct puncture of the venous segment. The selection of the method was based on the presence of deep afferent vessels to the fistula which were more easily managed by transarterial approach or, in cases where the venous dilatation was not so large, making direct puncture more difficult to be performed. For each patient in the present series, the elimination of the fistula was confirmed by angiography at the treatment conclusion and no recurrence was clinically recognized. All the patients presented satisfactory clinical and cosmetic outcomes and were clinically followed-up (follow-up period ranging between six and 32 months; mean, 20 months) to detect recurrence manifest as increase in volume or audible bruit. Follow-up angiography was not considered until a clinical suspicion of recurrence was raised, therefore none of the patients required such procedure. Cases description Patient 1 - A 43-year-old woman presented with a 5 × 6cm pulsatile mass on the right frontal region following a trauma in a car accident. Bilateral angiography of external carotid arteries demonstrated the large caliber of the superficial temporal artery and respective branches, with a direct fistula with the superficial temporal vein and superficial frontal veins. The fistula was easily demonstrated at angiography (Figure 1A). The treatment was performed by means of superselective microcatheterization of the superficial temporal artery with a flow-guided catheter and embolization with 1.5 ml NBCA at 33%. Total occlusion of the fistula and drainage vein was achieved (Figure 1B). 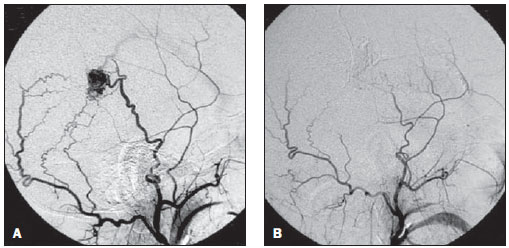 Figure 1. A: Pretreatment digital angiography of external carotid artery demonstrating arteriovenous fistula with draining vein dilatation, supplied by branches of the superficial temporal artery and, at a lower degree, by the left occipital artery. B: Digital angiography of external carotid artery following treatment with NBCA, demonstrating total occlusion of arteriovenous fistula and respective draining vein. Patient 3 - A 49-year-old man reported the presence of a mass on the preauricular region in association with pulsatile tinnitus, observed six months after a blunt injury in the region preceding the symptoms onset. The clinical examination demonstrated a pulsatile mass on the left preauricular region. Magnetic resonance angiography demonstrated the presence of a significant venous engorgement (Figures 2A and 2B) and a nodular lesion with absence of signal in this region. Angiography of the external carotid artery identified a high-output fistula between the artery and the superficial temporal vein that presented a large venous aneurysm. Additionally, intracranial drainage through the diploic veins (Figure 2C). Angiography performed under management of the proximal flow with a balloon-guided catheter clearly demonstrated a large fistula (Figure 2D) that was occluded with microcoils and NBCA. The fistula and respective drainage vein were completely occluded during embolization by arterial approach. The patient reported improvement of the tinnitus. 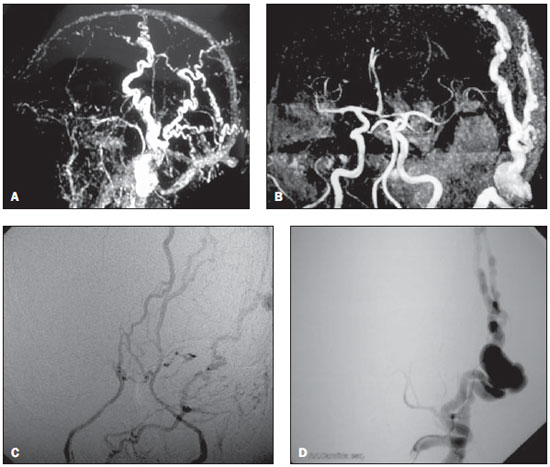 Figure 2. A: Magnetic resonance angiography with de TOF technique demonstrating marked superficial veins ectasia. B: Magnetic resonance angiography demonstrating dilated extracranial veins, without any detectable alteration in the intracranial circulation. C: Anteroposterior digital angiography of external carotid artery, at the venous phase, demonstrating the intracranial drainage of the fistula bilaterally through the cavernous and petrosal sinuses. D: Anteroposterior digital angiography of the external carotid artery, at the arterial phase, demonstrating arteriovenous fistula of the superficial temporal artery, with development of a large venous aneurysm in the preauricular region. DISCUSSION The management of scalp cirsoid aneurysms is complex. Therapeutic success is achieved with complete elimination of the abnormal arteriovenous communication with occlusion of all the drainage veins, otherwise recurrence is inevitable. Additionally, the treatment must be focused on the improvement of the cosmetic disfigurement that in most of cases is the patients' main preoccupation. Only 10% to 20% of these arteriovenous fistulas develop after penetrating cranial trauma. In 90% of the patients, the superficial temporal artery is the main afferent vessel to the fistula(9). In the remaining cases both the superficial temporal and occipital arteries are generally involved(9). The management of scalp cirsoid aneurysms is complex, particularly because of their high flow. Surgery has been the treatment of choice for a long time(2,7,10). Ligation of supply arteries is generally ineffective and should be avoided(2,6,11). With the developments in materials and endovascular techniques(5,12-14), a decrease in problems with the treatment of these patients has been observed. Previous studies report that embolization can completely occlude large arteriovenous fistulas, determining a significant clinical and even esthetic improvement in many patients(12-14), although a standard treatment for these rare lesions is still to be established. Generally, embolization performed as an adjuvant of surgical therapeutics is successful in the reduction of blood loss during the surgical excision of the lesion(5,13). It is known that embolization can heal an arteriovenous fistula of the scalp without determining its ischemia(14). Considering that these disfiguring masses are constituted mainly of large draining veins, these veins almost completely disappear after occlusion of the fistulous site and of the origin of these venous dilatations. In the present series, the lesions were managed solely by embolization. None of the cases required combined therapy. In the cases treated with direct puncture, NBCA injection was performed under mechanical compression of the draining veins for determining reduction in the blood flow (or even stasis) and to avoid the undesired escape of the liquid embolic material into the jugular vein or even into the pulmonary circulation. Embolization should be the primary therapy for this type of fistula. Surgical intervention should be reserved either for removal of residual fistulas that could not be occluded with embolization or for cases of more extensive fistulas. Presurgical embolization of arterial afferences is desirable because it makes the surgical procedure safer, reducing the risk for massive hemorrhage. In fact, proximal embolization does reduce the regional blood flow and has been a useful complement to surgery, but is rarely curative since the vascular endothelial growth factor is expressed by these lesions and will be responsible for their continuous growth(15). The selection of embolic materials must be based on the vascular architecture of the lesion as well as on the skill of the interventional radiologist. A combination of different embolic materials or even of several pathways to approach the nidus may be required(5,13). Although the etiology of these lesions still remains controversial, the hypothesis of either a congenital or traumatic origin has been generally accepted. In the present series, all the lesions could be directly related to trauma (most of them related to blunt trauma). Penetrating trauma is well described as cause for these lesions, including after hair transplant, temporomandibular joint arthroscopy and craniotomy for intracranial procedures(16-18). Congenital cirsoid aneurysms are actually more frequent than the traumatic ones, achieving an incidence of up to 80% in some series(18). Theories about their occurrence include persistence of arteriovenous fistulas. Although extremely rare, familial involvement has been described(19). The diagnosis is clinical in the majority of cases. Angiography is required for a better delineation of the lesion and to rule out the presence of an intracranial component(20). Such component may be consisted of an enlarged meningeal artery with afferent vessels crossing the diploe to feed the malformation. The diagnosis of scalp cirsoid aneurysm as well as its differentiation with sinus pericranii may be difficult and some confusion between these two types of lesion is present in the literature. In a strict sense, sinus pericranii corresponds to a collection of venous blood vessels firmly attached to the outer table of the skull directly communicating with the intracranial venous sinus by diploic veins through a bone defect(21,22). Indications for treatment include hemorrhage prevention, tinnitus alleviation or a noticeable presence of a cosmetic defect caused by the pulsatile mass. In the past, the treatment was essentially dependent on surgical excision or proximal ligation of supply arteries(22-24). Ligation of supply arteries is particularly problematic since this is not a curative technique besides causing loss of the arterial access to the fistula for embolization(25). Several forms of treatment for scalp cirsoid aneurysms including absolute alcohol embolization and microcoils have already been reported(13,26). Direct puncture embolization is aimed at occluding the beginning of the venous structure distal to the arteriovenous communication. Thus, with this technique, the occlusion of vascular structures does not involve any risk for ischemic skin complications. Immediate venous occlusion allows continuous embolic agent redistribution to the adjacent vascular spaces and an effective devascularization. For a temporary occlusion of the venous flow, the authors utilized a large ringshaped compression device (the so called cookie cutter technique), described by Duncan et al.(27), avoiding the unnecessary exposure of the operator's hand to radiation. In the present series, direct angiography with 21G Teflon needle was many times followed by adjustments of compression points, making the venous occlusion more effective. In most of lesions, a high-output arteriovenous fistula is associated with the venous aneurysm. Preoccupation that the embolic agent may pass to the pulmonary circulation must be always kept in mind. In order to avoid such an event, temporary manual compression during NBCA injection slows down the venous flow, preventing inadvertent embolization. Another measure to be adopted in the transarterial approach is the utilization of a balloon-guiding catheter for management of the proximal blood flow, performing the injection upon flow blockage. Recent developments in the design of microcatheters and in distal navigation techniques have allowed catheterization of afferent arteries proximal to the fistula. NBCA injection through a microcatheter may lead to complete devascularization of a scalp arteriovenous malformation without any risk for ischemia of the healthy adjacent tissue. CONCLUSIONS Endovascular management of cirsoid aneurysms is a safe and effective treatment alternative. Although this method may be effectively utilized as an adjuvant or complement to surgery, particularly in cases involving deep afferent structures, in most of times complete cure can be achieved on with the endovascular approach. The selection of the treatment method should be based on the lesion size, angioarchitecture, and clinical presentation. In general, satisfactory aesthetic outcomes can be achieved either by transarterial embolization or by direct puncture. REFERENCES 1. Coleman CC Jr, Hoopes JE. Congenital arteriovenous anomalies of the head and neck. Plast Reconstr Surg. 1971;47:354-64. 2. Rappaport I, Yim D. Congenital arteriovenous fistulas of the head and neck. Arch Otolaryngol. 1973;97:350-3. 3. Szilagyi DE, Elliott JP, DeRusso FJ, et al. Peripheral congenital arteriovenous fistulas. Surgery. 1965;57:61-81. 4. Fisher-Jeffes ND, Domingo Z, Madden M, et al. Arteriovenous malformations of the scalp. Neurosurgery. 1995;36:656-60. 5. Kaufman SL, Kumar AAJ, Roland JMA, et al. Transcatheter embolization in the management of congenital arteriovenous malformations. Radiology. 1980;137(1 Pt 1):21-9. 6. Khodadad G. Arteriovenous malformations of the scalp. Ann Surg. 1973;177:79-85. 7. Komatsu Y, Narushima K, Kobayashi E, et al. Congenital arteriovenous malformation of the scalp - case report. Neurol Med Chir (Tokyo). 1989;29:230-4. 8. Marotta TR, Berenstein A, Zide B. The combined role of embolization and tissue expanders in the management of arteriovenous malformations of the scalp. AJNR Am J Neuroradiol. 1994;15:1240-6. 9. Gurkanlar D, Gonul M, Solmaz I, et al. Cirsoid aneurysms of the scalp. Neurosurg Rev. 2006;29:208-12. 10. Schultz RC, Hermosillo CX. Congenital arteriovenous malformation of the face and scalp. Plast Reconstr Surg. 1980;65:496-501. 11. Ogawa Y, Inoue K. Electrothrombosis as a treatment of cirsoid angioma in the face and scalp and varicosis of the leg. Plast Reconstr Surg. 1982;70:310-8. 12. Barnwell SL, Halbach VV, Dowd CF, et al. Endovascular treatment of scalp arteriovenous fistulas associated with a large varix. Radiology. 1989;173:533-9. 13. Heilman CB, Kwan ES, Klucznik RP, et al. Elimination of a cirsoid aneurysm of the scalp by direct percutaneous embolization with thrombogenic coils. Case report. J Neurosurg. 1990;73:296-300. 14. Kasdon DL, Altemus LR, Stein BM. Embolization of a traumatic arteriovenous fistula of the scalp with radiopaque Gelfoam pledgets. Case report and technical note. J Neurosurg. 1976;44:753-6. 15. Waga S, Ohtsubo K, Handa J, et al. Extracranial congenital arterio-venous malformations. Surg Neurol. 1974;2:241-5. 16. Williams LR, Robinson JK, Yao JS. Hair transplantation producing arteriovenous fistulization. Ann Vasc Surg. 1986;1:241-3. 17. Preisler SA, Koorbusch GF, Olson RA. An acquired arteriovenous fistula secondary to temporomandibular joint arthroscopy: report of a case. J Oral Maxillofac Surg. 1991;49:187-90. 18. Morioka T, Nishio S, Hikita T. Traumatic arteriovenous fistulae of the scalp at the area of previous craniotomy. Surg Neurol. 1988;30:404-7. 19. Khodadad G. Familial cirsoid aneurysm of the scalp. J Neurol Neurosurg Psychiat. 1971;34:664-7. 20. Verbiest H. Results of artificial slow flow angiography with arteriovenous aneurysms in the supply area of the external or internal carotid arteries. Am J Roentgenol Radium Ther Nucl Med. 1972;116:1-15. 21. Lanzino G, Passacantilli E, Lemole GM Jr, et al. Scalp arteriovenous malformation draining into the superior sagittal sinus associated with an intracranial arteriovenous malformation: just a coincidence? Case report. Neurosurgery. 2003;52:440-3. 22. Vinas FC, Valenzuela S, Zuleta A. Literature review: sinus pericranii. Neurol Res. 1994;16:471-4. 23. Nagasaka S, Fukushima T, Goto K, et al. Treatment of scalp arteriovenous malformation. Neurosurgery. 1996;38:671-7. 24. Shenoy SN, Raja A. Scalp arteriovenous malformations. Neurol India. 2004;52:478-81. 25. Han MH, Seong SO, Kim HD, et al. Craniofacial arteriovenous malformation: preoperative embolization with direct puncture and injection of n-butyl cyanoacrylate. Radiology. 1999;211:661-6. 26. Mourao GS, Hodes JE, Gobin YP, et al. Curative treatment of scalp arteriovenous fistulas by direct puncture and embolization with absolute alcohol. Report of three cases. J Neurosurg. 1991;75:634-7. 27. Duncan IC, Fourie PA. Circumferential flow reduction during percutaneous embolotherapy of extracranial vascular malformations: the "cookie-cutter" technique. AJNR Am J Neuroradiol. 2003;24:1453-5. 1. Master, MD, Radiologist at Department of Radiology - Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro (HUCFF-UFRJ), Rio de Janeiro, RJ, Brazil Study developed at Department of Radiology - Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro (HUCFF-UFRJ), Rio de Janeiro, RJ, Brazil Mailing address: Dr. Eduardo Wajnberg Rua Lopes Quintas, 100/602, Jardim Botânico 22460-010. Rio de Janeiro, RJ, Brazil E-mail: eduardowj@gmail.com Received April 26, 2010 Accepted after revision June 18, 2010 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554