Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 4 - July / Aug. of 2007
Vol. 40 nº 4 - July / Aug. of 2007
|
ORIGINAL ARTICLE
|
|
Radiological evaluation of postoperative gastrointestinal alterations in patients submitted to Fobi-Capella surgery |
|
|
Autho(rs): Marina Celli Francisco, Simone Maluf Barella, Thiago Giansante Abud, Vanessa Sales Vilar, Samuel Reibscheid, Carlos Harou Arasaki, Jacob Szejnfeld |
|
|
Keywords: Morbid obesity, Gastroplasty, Upper gastrointestinal series, Bariatric surgery, Fobi-Capella |
|
|
Abstract:
IMDs, Residents, Departamento de Diagnóstico por Imagem da Universidade Federal de São Paulo-Escola Paulista de Medicina (Unifesp-EPM), São Paulo, SP, Brazil
INTRODUCTION Obesity is a severe public health problem, and, according to asurvey performed late in 2004 in a partnership between theInstituto Brasileiro de Geografia e Estatística (BrazilianInstitute of Geography and Statistics) and the Brazilian Ministryof Health, 40.6% of the Brazilian population above 20 years ofage is overweight, differently from 30 years ago when only 16% ofthe adult population was affected by obesity. It is estimatedthat one million Brazilians are morbidobese(1). The surgery for obesity management is indicated as analternative for treating morbid obesity resulting in a markedreduction of comorbidities in patients who have not showedresponse to appropriate clinical treatments. This surgery isregulated by the Brazilian health authorities since 2001, and isperformed in institutions that deliver services within theSistema Único de Saúde (SUS) (Brazilian PublicHealth System). According to the Ministry of Health statistics,during 2004 in Brazil, 2,014 bariatric surgeries were performedwithin the SUS(1). Several surgical techniques are currently available for morbidobesity management(2–4). Currently, Roux-en-Ygastric bypass (Fobi Capella bariatric surgery) is the mostfrequently utilized technique for treating morbid obesity,because of its high effectiveness and lowmorbimortality(5). This procedure involves thecreation of a gastric pouch of approximately 20 cc. The remainingstomach, as well as the duodenum and the first 50 cm of thejejunum remain permanently excluded from the digestive tract. Thesmall gastric pouch is anastomosed to an isolated jejunal loop ina Y configuration and its emptying process is limited by asilicone ring that reduces the gastric lumen to 12 mm. Secretionsoriginated from the excluded stomach and duodenum flow into thejejunum through an anastomosis measuring 100–159 cm, thisdistance being related to the patient's body mass index (BMI).The silicone ring is distally placed at about 5.5 cm from theesophagogastric transition and 1.5 cm proximal to thegastrojejunal anastomosis(6). The method of choice for evaluating alterations resulting frombariatric surgery is the upper gastrointestinal series.Innumerable studies report that some of these complications maybe structural (fistulas, intestinal obstruction, stenoses,internal hernias, marginal ulcers) or functional (nausea, emesis,diarrhea, dumping syndrome, constipation and gastroesophagealreflux disease)(3,7,8). The present study is aimed at reporting postoperativealterations resulting from Fobi-Capella surgery, diagnosed byupper gastrointestinal series.
MATERIALS AND METHODS Prospective radiological study of 41 patients submitted tobariatric surgery (Fobi Capella technique) with insertion of acontention ring, between May/2000 and June/2005. Thirty-three ofthese patients were women, and eight men, with ages rangingbetween 23 and 63 years (mean age 45.3 years). Postoperativeweight loss ranged between 22 kg and 71 kg (mean = 45.6 kg.). The radiological study was initiated with an upper abdominalplain radiograph. After that, under radioscopic control, thepatient was orally given small amounts of 50% barium sulfate, forevaluating the morphology and emptying of esophagus, stomach andanastomosis. Then, the amount of barium ingested was adequatelyincreased, usually up to no more than 150 cc, according to theradiologist control. Radiographs were routinely taken in thefollowing positions: orthostatic, for anteroposterior and obliqueviews; lateral orthostatic; dorsal decubitus in the rightanterior oblique view; ventral decubitus (Schatzky'sposition). Other radiographic views were taken under radioscopic control.A proximal jejunal radiograph completed the study. Patientsweighting more than 130 kg were evaluated only in the orthostaticposition, because the radiological table could not support such aweight.
RESULTS Postoperative alterations have been found in 51.2% of studies, the most frequent being gastroesophageal reflux disease, followed by seven cases of hiatal hernia, with three patients presenting with both alterations (Table 1).
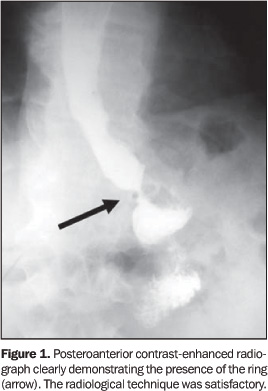
DISCUSSION Obesity is a chronic and universal disease whose prevalencecontinues to increase at concerning rates, especially in Westerncountries. In the last 30 years, the obese population increasedmore than 90%(9). Bariatric surgery was firstly reported in 1954 by Kremer etal., in a study describing a jejunoileal bypass. The term"bariatric" is originally derived from the Greek baros,meaning "weight", and iatrike, meaning"treatment"(10). In 1986, Mathias Fobidescribed the gastric bypass technique reported by the presentstudy(11). In the last years, bariatric surgery has gained acceptance both from the medical community and the public in general. It is considered as a relatively safe surgery(12) (Figure 1).
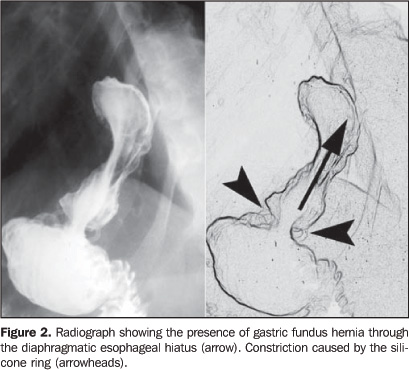
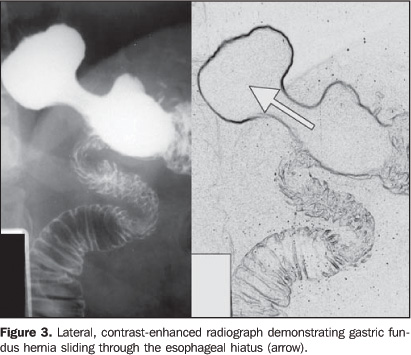
With the remarkable increase in the incidence of morbidobesity, gastroplasty surgeries, particularly Fobi-Capellasurgeries, have become increasingly frequent, so the knowledge ofthe technique and possible alterations and complications becomemore and more significant, considering that the clinicalexamination of these patients is impaired by the obesity itself.Many times, the radiologist is the first to detect complicationsas a result from this surgery. By this reason, it is extremelyimportant that the specialist knows the possible complications aswell as their appearance in imaging studies. An extensive literature review has shown that 72.6% of thepatients submitted to bariatric surgery were women, a data thatalso has shown to be more prevalent in the present casuistic,corresponding to 80.5% of the patients submitted to thisprocedure. Mean age was 38.97 years, a little below the mean ageof the population included in the present study (45.3 years). Themortality rate described in the literature is 0.5%. An analysisof 936 gastroplasty surgeries has demonstrated a mean weight lossof 39.45 kg, a little below the 45.6 kg found in the presentstudy(13). Upper gastrointestinal series have shown alterations in 51.2% of patients, however, not all gastroesophageal reflux diseases and hiatal hernias should be considered as postoperative surgical complications, considering that a preoperative examination has not been performed. With the exclusion of these complications, the total of remaining complications would correspond to 14.3%, a little below the percentage reported in the literature (20–25%)(14). In another study performed by Arasaki et al., who have also performed the surgeries in the present study, 23% of patients have presented postoperative gastroesophageal reflux disease when a standard-sized silicone ring was utilized, and only 8% with a little larger ring, therefore it may be concluded that the resulting lower esophageal sphincter function may be related to some cases of postoperative gastroesophageal reflux disease(6) (Figures 2 and 3).
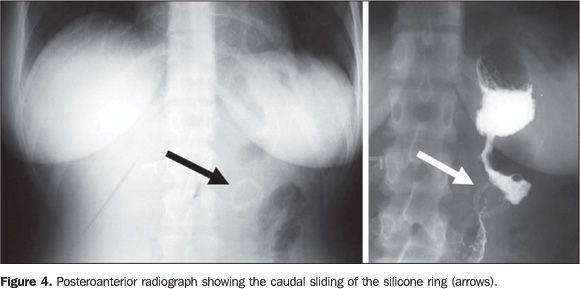
In the present casuistic, 4.8% of patients presented sliding of the silicone ring, and in 2.4% of cases, the ring could not be visualized because of its removal due the patient´s intolerance. Closset et al., who have followed-up 214 patients, have reported the ring removal in 4.2% of cases(15). Plain radiography plays an extremely significant role in the definition of the silicone ring presence and topography (Figure 4).
Stenosis of gastrojejunal anastomosis was found in only onepatient (2.4%), a little below the percentages reported by theliterature (3–27%)(14–18). DeMaria et al. haveevaluated 281 patients and reported this event in 6.6% ofcases(17). Ulcers may be caused by exposure to gastric acids from thegastrojejunal anastomosis or by ischemia. Studies in theliterature report ulcers occurrence in 1% to 5% of cases,however, no case of ulcer was found in the presentstudy(14–17). The present study has found one case of bezoar (2.4%), whilethe literature reports a 1.9% incidence(19).Also, one case of enterocutaneous fistula was found, whileCapella et al. report a low incidence of thiscomplication(20).
CONCLUSION In the present study, upper gastrointestinal series hasclearly demonstrated postoperative alterations in patientssubmitted to Fobi-Capella surgery. Gastroesophageal refluxdisease (19.5%) and hiatal hernia (17%) cannot be attributed tothe surgery, considering that a preoperative examination was notperformed. The radiological technique has been considered assatisfactory. The plain radiograph is mandatory for demonstratingthe silicone ring presence and topography.
REFERENCES 1. Obesidade: SUS realiza três novos tipos de cirurgia para redução do estômago. [Acessado em: 23/7/2005]. Disponível em: http:/portal.saude.gov.br/portal [ ] 2. Buchwald H; Consensus Conference Panel. Bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. J Am Coll Surg 2005;200:593–604. [ ] 3. Capella JF, Capella RF. An assessment of vertical banded gastroplasty – Roux-en-Y gastric bypass for the treatment of morbid obesity. Am J Surg 2002;183:117–123. [ ] 4. Capella RF, Capella JF, Mandec H, Nath P. Vertical banded gastroplasty – gastric bypass: preliminary report. Obes Surg 1991;1:389–395. [ ] 5. Garrido ABJ. Cirurgia em obesos mórbidos: experiência pessoal. Arq Bras Endocrinol Metab 2000;44:106–113. [ ] 6. Arasaki CH, Del Grande JC, Yanagita ET, Alves AK, Oliveira DR. Incidence of regurgitation after the banded gastric bypass. Obes Surg 2005;15: 1408–1417. [ ] 7. Huang CS, Farraye FA. Complications following bariatric surgery. Tech Gastrointest Endosc 2006; 8:54–65. [ ] 8. Smith C, Gardiner R, Kubicka RA, Dieschbourg JJ. Radiology of gastric restrictive surgery. RadioGraphics 1985;5:193–216. [ ] 9. Faria OP, Pereira VA, Gangoni CMC, et al. Obesos mórbidos tratados com gastroplastia redutora com bypass gástrico em Y de Roux: análise de 160 pacientes. Brasília Med 2002;39:26–34. [ ] 10. Salameh JR. Bariatric surgery: past and present. Am J Med Sci 2006;331:194–200. [ ] 11. Fobi MAL, Fleming AW. Vertical banded gastroplasty vs gastric bypass in the treatment of obesity. J Natl Med Assoc 1986;78:1091–1098. [ ] 12. Nguyen NT, Silver M, Robinson M, et al. Result of a National Audit of Bariatric Surgery Performed at Academic Centers; a 2004 University HealthSystem Consortium Benchmarking Project. Arch Surg 2006;141:445–450. [ ] 13. Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–1737. [ ] 14. Sandrasegaran K, Rajesh A, Lall C, Gómez GA, Lappas JC, Maglinte DD. Gastrointestinal complications of bariatric Roux-en-Y gastric bypass surgery. Eur Radiol 2005;15:254–262. [ ] 15. Closset J, Mehdi A, Barea M, Buedts K, Gelin M, Houben JJ. Results of silastic ring vertical gastroplasty more than 6 years after surgery: analysis of a cohort of 214 patients. Obes Surg 2004;14: 1233–1236. [ ] 16. Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 2000;232:515–529. [ ] 17. DeMaria EJ, Sugerman HJ, Kellum JM, Meador JG, Wolfe LG. Results of 281 consecutive total laparoscopic Roux-en-Y gastric bypasses to treat morbid obesity. Ann Surg 2002;235:640–647. [ ] 18. Higa KD, Boone KB, Ho T, Davies OG. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg 2000;135:1029–1033. [ ] 19. Ferraz AAB, Sá VCT, Arruda PCL, Leão CS, Campos JM, Ferraz EM. Obstrução gastrointestinal por fitobezoar na cirurgia bariátrica. Rev Col Bras Cir 2006;33:35–38. [ ] 20. Capella JF, Capella RF. The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass? Am J Surg 1996;171:74–79. [ ]
Received September 7, 2006. Accepted after revision November 27, 2006.
* Study developed in the Departamento de Diagnóstico por Imagem da Universidade Federal de São Paulo-Escola Paulista de Medicina (Unifesp-EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554